Korean J Radiol.
2015 Dec;16(6):1364-1372. 10.3348/kjr.2015.16.6.1364.
Ultrasonographic Diagnosis of Biliary Atresia Based on a Decision-Making Tree Model
- Affiliations
-
- 1Department of Radiology, Seoul National University College of Medicine, Seoul 03080, Korea. cheonje@snu.ac.kr
- KMID: 2344293
- DOI: http://doi.org/10.3348/kjr.2015.16.6.1364
Abstract
OBJECTIVE
To assess the diagnostic value of various ultrasound (US) findings and to make a decision-tree model for US diagnosis of biliary atresia (BA).
MATERIALS AND METHODS
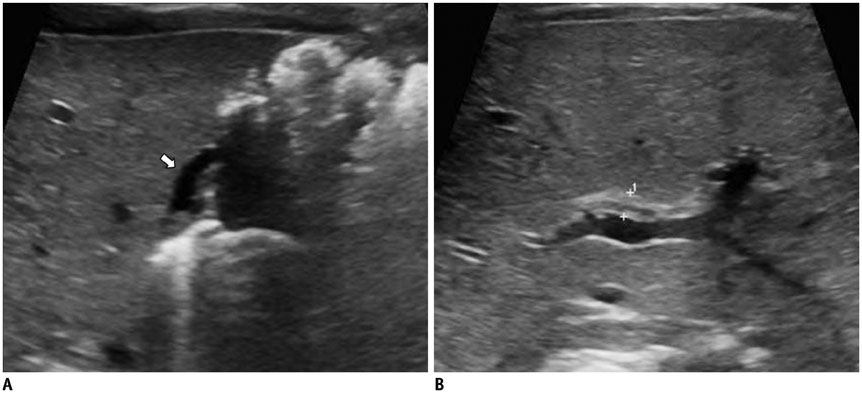
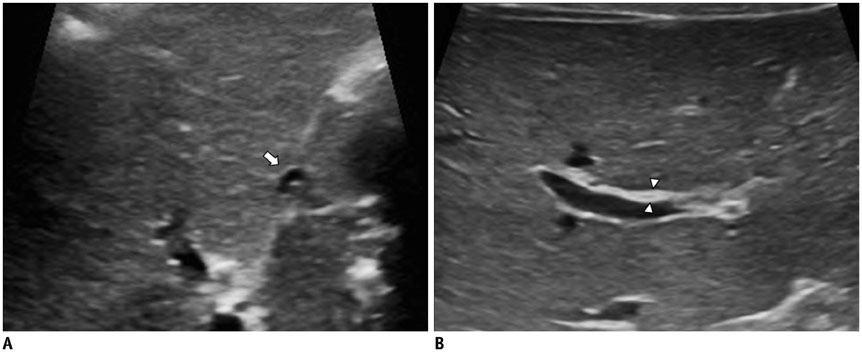
From March 2008 to January 2014, the following US findings were retrospectively evaluated in 100 infants with cholestatic jaundice (BA, n = 46; non-BA, n = 54): length and morphology of the gallbladder, triangular cord thickness, hepatic artery and portal vein diameters, and visualization of the common bile duct. Logistic regression analyses were performed to determine the features that would be useful in predicting BA. Conditional inference tree analysis was used to generate a decision-making tree for classifying patients into the BA or non-BA groups.
RESULTS
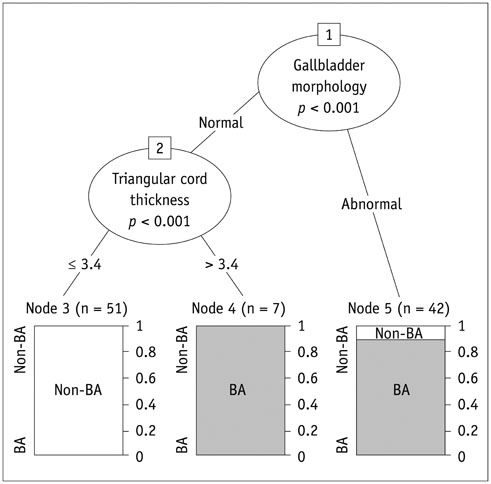
Multivariate logistic regression analysis showed that abnormal gallbladder morphology and greater triangular cord thickness were significant predictors of BA (p = 0.003 and 0.001; adjusted odds ratio: 345.6 and 65.6, respectively). In the decision-making tree using conditional inference tree analysis, gallbladder morphology and triangular cord thickness (optimal cutoff value of triangular cord thickness, 3.4 mm) were also selected as significant discriminators for differential diagnosis of BA, and gallbladder morphology was the first discriminator. The diagnostic performance of the decision-making tree was excellent, with sensitivity of 100% (46/46), specificity of 94.4% (51/54), and overall accuracy of 97% (97/100).
CONCLUSION
Abnormal gallbladder morphology and greater triangular cord thickness (> 3.4 mm) were the most useful predictors of BA on US. We suggest that the gallbladder morphology should be evaluated first and that triangular cord thickness should be evaluated subsequently in cases with normal gallbladder morphology.
Keyword
MeSH Terms
-
Area Under Curve
Biliary Atresia/*diagnosis/ultrasonography
Common Bile Duct/ultrasonography
Decision Making
Diagnosis, Differential
Female
Gallbladder/ultrasonography
Hepatic Artery/ultrasonography
Humans
Infant
Infant, Newborn
Jaundice, Obstructive/complications/diagnosis
Logistic Models
Male
Portal Vein/ultrasonography
ROC Curve
Retrospective Studies
Sensitivity and Specificity
Figure
Reference
-
1. Balistreri WF, Grand R, Hoofnagle JH, Suchy FJ, Ryckman FC, Perlmutter DH, et al. Biliary atresia: current concepts and research directions. Summary of a symposium. Hepatology. 1996; 23:1682–1692.2. Valayer J. Conventional treatment of biliary atresia: long-term results. J Pediatr Surg. 1996; 31:1546–1551.3. Ikeda S, Sera Y, Ohshiro H, Uchino S, Akizuki M, Kondo Y. Gallbladder contraction in biliary atresia: a pitfall of ultrasound diagnosis. Pediatr Radiol. 1998; 28:451–453.4. Park WH, Choi SO, Lee HJ, Kim SP, Zeon SK, Lee SL. A new diagnostic approach to biliary atresia with emphasis on the ultrasonographic triangular cord sign: comparison of ultrasonography, hepatobiliary scintigraphy, and liver needle biopsy in the evaluation of infantile cholestasis. J Pediatr Surg. 1997; 32:1555–1559.5. Nicotra JJ, Kramer SS, Bellah RD, Redd DC. Congenital and acquired biliary disorders in children. Semin Roentgenol. 1997; 32:215–227.6. Visrutaratna P. Biliary atresia: making the diagnosis by the gallbladder ghost triad. Pediatr Radiol. 2003; 33:902. author reply 903.7. Lee HJ, Lee SM, Park WH, Choi SO. Objective criteria of triangular cord sign in biliary atresia on US scans. Radiology. 2003; 229:395–400.8. Park WH, Choi SO, Lee HJ. Technical innovation for noninvasive and early diagnosis of biliary atresia: the ultrasonographic "triangular cord" sign. J Hepatobiliary Pancreat Surg. 2001; 8:337–341.9. Choi SO, Park WH, Lee HJ, Woo SK. "Triangular cord": a sonographic finding applicable in the diagnosis of biliary atresia. J Pediatr Surg. 1996; 31:363–366.10. Weinberger E, Blumhagen JD, Odell JM. Gallbladder contraction in biliary atresia. AJR Am J Roentgenol. 1987; 149:401–402.11. Azuma T, Nakamura T, Nakahira M, Harumoto K, Nakaoka T, Moriuchi T. Pre-operative ultrasonographic diagnosis of biliary atresia--with reference to the presence or absence of the extrahepatic bile duct. Pediatr Surg Int. 2003; 19:475–477.12. Kim WS, Cheon JE, Youn BJ, Yoo SY, Kim WY, Kim IO, et al. Hepatic arterial diameter measured with US: adjunct for US diagnosis of biliary atresia. Radiology. 2007; 245:549–555.13. Lee MS, Kim MJ, Lee MJ, Yoon CS, Han SJ, Oh JT, et al. Biliary atresia: color doppler US findings in neonates and infants. Radiology. 2009; 252:282–289.14. El-Guindi MA, Sira MM, Konsowa HA, El-Abd OL, Salem TA. Value of hepatic subcapsular flow by color Doppler ultrasonography in the diagnosis of biliary atresia. J Gastroenterol Hepatol. 2013; 28:867–872.15. Hothorn T, Hornik K, Zeileis A. Unbiased recursive partitioning: a conditional inference framework. J Comput Graph Stat. 2006; 15:651–674.16. Zhou LY, Wang W, Shan QY, Liu BX, Zheng YL, Xu ZF, et al. Optimizing the US diagnosis of biliary atresia with a modified triangular cord thickness and gallbladder classification. Radiology. 2015; 277:181–191.17. Farrant P, Meire HB, Mieli-Vergani G. Ultrasound features of the gall bladder in infants presenting with conjugated hyperbilirubinaemia. Br J Radiol. 2000; 73:1154–1158.18. Farrant P, Meire HB, Mieli-Vergani G. Improved diagnosis of extraheptic biliary atresia by high frequency ultrasound of the gall bladder. Br J Radiol. 2001; 74:952–954.19. Ohi R, Masaki N. The jaundiced infant: biliary atresia and other obstructions. In : O'Neill JA, Rowe MI, Grosfeld JL, Fonkalsrud EW, Coran AG, editors. Pediatric surgery. Philadelphia: Mosby Elsevier;1998. p. 1465–1481.20. Burton EM, Babcock DS, Heubi JE, Gelfand MJ. Neonatal jaundice: clinical and ultrasonographic findings. South Med J. 1990; 83:294–302.21. Kirks DR, Coleman RE, Filston HC, Rosenberg ER, Merten DF. An imaging approach to persistent neonatal jaundice. AJR Am J Roentgenol. 1984; 142:461–465.22. Takamizawa S, Zaima A, Muraji T, Kanegawa K, Akasaka Y, Satoh S, et al. Can biliary atresia be diagnosed by ultrasonography alone? J Pediatr Surg. 2007; 42:2093–2096.23. Park WH, Choi SO, Lee HJ. The ultrasonographic 'triangular cord' coupled with gallbladder images in the diagnostic prediction of biliary atresia from infantile intrahepatic cholestasis. J Pediatr Surg. 1999; 34:1706–1710.24. Lee SY, Kim GC, Choe BH, Ryeom HK, Jang YJ, Kim HJ, et al. Efficacy of US-guided percutaneous cholecystocholangiography for the early exclusion and type determination of biliary atresia. Radiology. 2011; 261:916–922.25. Kanegawa K, Akasaka Y, Kitamura E, Nishiyama S, Muraji T, Nishijima E, et al. Sonographic diagnosis of biliary atresia in pediatric patients using the "triangular cord" sign versus gallbladder length and contraction. AJR Am J Roentgenol. 2003; 181:1387–1390.26. Tan Kendrick AP, Phua KB, Ooi BC, Subramaniam R, Tan CE, Goh AS. Making the diagnosis of biliary atresia using the triangular cord sign and gallbladder length. Pediatr Radiol. 2000; 30:69–73.27. Humphrey TM, Stringer MD. Biliary atresia: US diagnosis. Radiology. 2007; 244:845–851.28. Mittal V, Saxena AK, Sodhi KS, Thapa BR, Rao KL, Das A, et al. Role of abdominal sonography in the preoperative diagnosis of extrahepatic biliary atresia in infants younger than 90 days. AJR Am J Roentgenol. 2011; 196:W438–W445.29. Han SJ, Kim MJ, Han A, Chung KS, Yoon CS, Kim D, et al. Magnetic resonance cholangiography for the diagnosis of biliary atresia. J Pediatr Surg. 2002; 37:599–604.30. Norton KI, Glass RB, Kogan D, Lee JS, Emre S, Shneider BL. MR cholangiography in the evaluation of neonatal cholestasis: initial results. Radiology. 2002; 222:687–691.31. Liu B, Cai J, Xu Y, Peng X, Zheng H, Huang K, et al. Three-dimensional magnetic resonance cholangiopancreatography for the diagnosis of biliary atresia in infants and neonates. PLoS One. 2014; 9:e88268.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum: Ultrasonographic Diagnosis of Biliary Atresia Based on a Decision-Making Tree Model
- Ultrasonographic diagnosis of biliary atresia in infants
- Overview of Biliary Atresia
- A Case of Congenital Biliary Atresia associated with Ectopic Pancreatic Tissue
- Public Health Nurses' Decision Making Models and Their Knowledge Structure