J Korean Med Assoc.
2011 Jan;54(1):22-34.
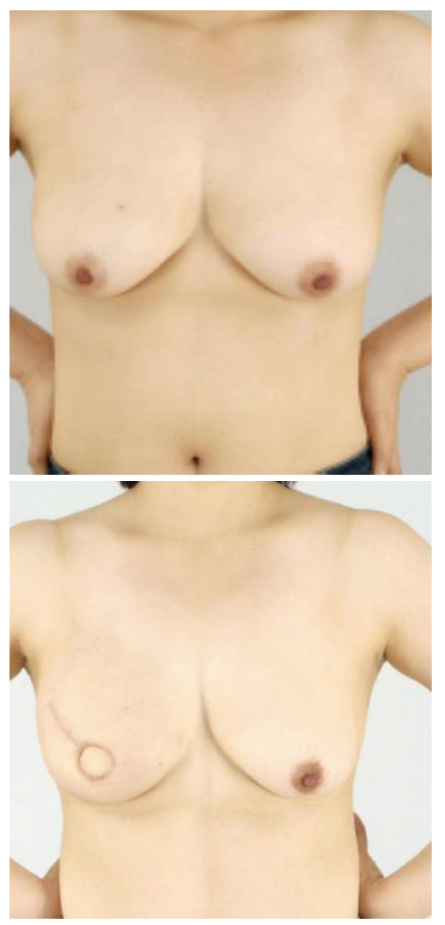
Breast reconstruction using the transverse rectus abdominis musculocutaneous (TRAM) free flap
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Seoul National University College of Medicine, Seoul, Korea. minnkw@snu.ac.kr
Abstract
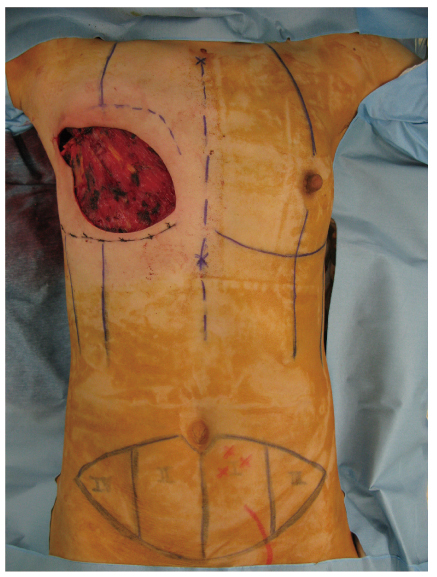
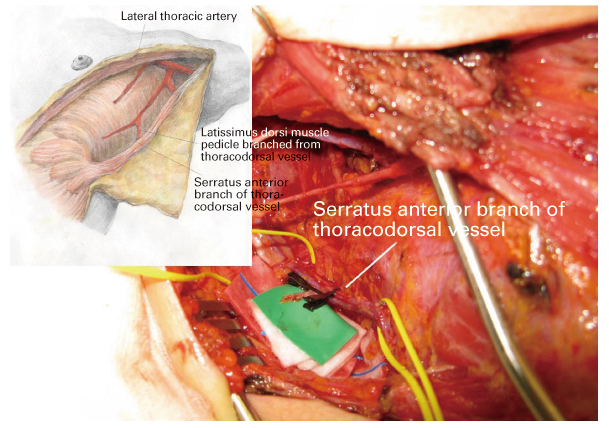
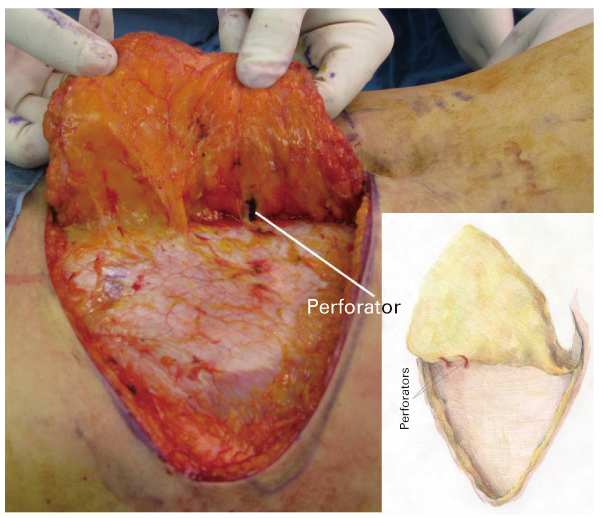
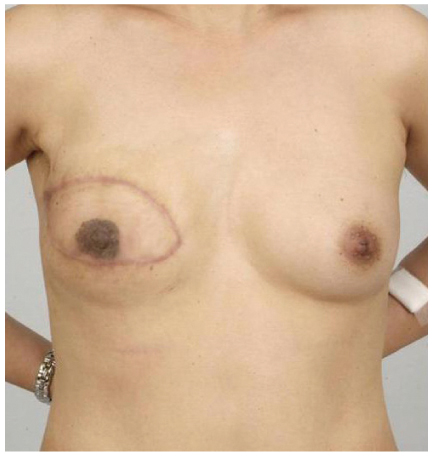
- Breast reconstruction is achieved through surgical procedures following mastectomy after breast cancer or trauma using implants or autologous tissue to restore the breast morphology. Reconstruction can physically and emotionally restore a patient's self confidence after the loss of a breast. The method of breast reconstruction is determined by several factors, such as the patient's general medical condition, the extent of the mastectomy, and donor site suitability when opting for autologous flap transplantation. Generally, we can classify breast reconstruction procedures into two broad categories: breast implantation after tissue expansion of the skin of the chest, and flaps using autologous tissue. Of the breast reconstruction methods using autologous tissue, the transverse rectus abdominis musculocutaneous free flap is advantageous over the the transverse rectus abdominis musculocutaneous (TRAM) pedicled flap in that it is easy to obtain the desired shape of the breast, the inframammary fold is maintained, and there is decreased donor site morbidity because the rectus abdominis muscle can be utilized sparingly. Moreover, the TRAM free flap can have an abdominoplasty effect in women who have excessive abdominal fat. However, the procedure is time consuming because microanastomosis of the pedicle and recipient vessel is necessary after flap elevation. Although there are several issues, such as the high cost of surgery, which should be resolved, breast reconstruction can provide support to many women who are emotionally and physically distressed due to breast cancer.
MeSH Terms
Figure
Reference
-
1. Atisha D, Alderman AK, Lowery JC, Kuhn LE, Davis J, Wilkins EG. Prospective analysis of long-term psychosocial outcomes in breast reconstruction: two-year postoperative results from the Michigan Breast Reconstruction Outcomes Study. Ann Surg. 2008. 247:1019–1028.
Article2. Pomahac B, Recht A, May JW, Hergrueter CA, Slavin SA. New trends in breast cancer management: is the era of immediate breast reconstruction changing? Ann Surg. 2006. 244:282–288.3. Yamada A, Harii K, Hirabayashi S, Kawashima T, Asato H. Breast reconstruction with the free TRAM flap after breast cancer surgery. J Reconstr Microsurg. 1992. 8:1–6.
Article4. Tran NV, Chang DW, Gupta A, Kroll SS, Robb GL. Comparison of immediate and delayed free TRAM flap breast reconstruction in patients receiving postmastectomy radiation therapy. Plast Reconstr Surg. 2001. 108:78–82.
Article5. Giacalone PL, Rathat G, Daures JP, Benos P, Azria D, Rouleau C. New concept for immediate breast reconstruction for invasive cancers: feasibility, oncological safety and esthetic outcome of post-neoadjuvant therapy immediate breast reconstruction versus delayed breast reconstruction: a prospective pilot study. Breast Cancer Res Treat. 2010. 122:439–451.
Article6. Elliott LF, Seify H, Bergey P. The 3-hour muscle-sparing free TRAM flap: safe and effective treatment review of 111 consecutive free TRAM flaps in a private practice setting. Plast Reconstr Surg. 2007. 120:27–34.
Article7. Vega S, Smartt JM Jr, Jiang S, Selber JC, Brooks CJ, Herrera HR, Serletti JM. 500 Consecutive patients with free TRAM flap breast reconstruction: a single surgeon's experience. Plast Reconstr Surg. 2008. 122:329–339.
Article8. Andrades P, Fix RJ, Danilla S, Howell RE 3rd, Campbell WJ, De la Torre J, Vasconez LO. Ischemic complications in pedicle, free, and muscle sparing transverse rectus abdominis myocutaneous flaps for breast reconstruction. Ann Plast Surg. 2008. 60:562–567.
Article9. Nahabedian MY, Tsangaris T, Momen B. Breast reconstruction with the DIEP flap or the muscle-sparing (MS-2) free TRAM flap: is there a difference? Plast Reconstr Surg. 2005. 115:436–444.
Article10. Schaverien MV, Perks AG, McCulley SJ. Comparison of outcomes and donor-site morbidity in unilateral free TRAM versus DIEP flap breast reconstruction. J Plast Reconstr Aesthet Surg. 2007. 60:1219–1224.
Article11. Scheer AS, Novak CB, Neligan PC, Lipa JE. Complications associated with breast reconstruction using a perforator flap compared with a free TRAM flap. Ann Plast Surg. 2006. 56:355–358.
Article12. Dayhim F, Wilkins EG. The impact of Pfannenstiel scars on TRAM flap complications. Ann Plast Surg. 2004. 53:432–435.
Article13. Collin TW, Coady MS. Is pregnancy contraindicated following free TRAM breast reconstruction? J Plast Reconstr Aesthet Surg. 2006. 59:556–559.
Article14. Rosson GD, Williams CG, Fishman EK, Singh NK. 3D CT angiography of abdominal wall vascular perforators to plan DIEAP flaps. Microsurgery. 2007. 27:641–646.
Article15. Giunta RE, Geisweid A, Feller AM. The value of preoperative Doppler sonography for planning free perforator flaps. Plast Reconstr Surg. 2000. 105:2381–2386.
Article16. Munhoz AM, Aldrighi CM. Breast cancer local recurrence after mastectomy and TRAM flap reconstruction: incidence and treatment options. Plast Reconstr Surg. 2006. 118:1664–1665.
Article17. Moran SL, Nava G, Behnam AB, Serletti JM. An outcome analysis comparing the thoracodorsal and internal mammary vessels as recipient sites for microvascular breast reconstruction: a prospective study of 100 patients. Plast Reconstr Surg. 2003. 111:1876–1882.
Article18. Lorenzetti F, Kuokkanen H, von Smitten K, Asko-Seljavaara S. Intraoperative evaluation of blood flow in the internal mammary or thoracodorsal artery as a recipient vessel for a free TRAM flap. Ann Plast Surg. 2001. 46:590–593.
Article19. Hammond DC, Simon AM, Khuthaila DK, Hoberman L, Sohn S. Latissimus dorsi flap salvage of the partially failed TRAM flap breast reconstruction. Plast Reconstr Surg. 2007. 120:382–389.
Article20. Kronowitz SJ, Kuerer HM, Hunt KK, Ross MI, Massey PR, Ensor JE, Robb GL. Impact of sentinel lymph node biopsy on the evolution of breast reconstruction. Plast Reconstr Surg. 2006. 118:1089–1099.
Article21. Minn KW, Hong KY, Lee SW. Preoperative TRAM free flap volume estimation for breast reconstruction in lean patients. Ann Plast Surg. 2010. 64:397–401.
Article22. Ritter EF, Cronan JC, Rudner AM, Serafin D, Klitzman B. Improved microsurgical anastomotic patency with low molecular weight heparin. J Reconstr Microsurg. 1998. 14:331–336.
Article23. Cohn AB, Walton RL. Immediate autologous breast reconstruction using muscle-sparing TRAM flaps with superficial epigastric system turbocharging: a salvage option. J Reconstr Microsurg. 2006. 22:153–156.
Article24. Glasberg SB, D'Amico RA. Use of regenerative human acellular tissue (AlloDerm) to reconstruct the abdominal wall following pedicle TRAM flap breast reconstruction surgery. Plast Reconstr Surg. 2006. 118:8–15.
Article25. Saulis AS, Mustoe TA, Fine NA. A retrospective analysis of patient satisfaction with immediate postmastectomy breast reconstruction: comparison of three common procedures. Plast Reconstr Surg. 2007. 119:1669–1676.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Breast reconstruction using pedicled transverse rectus abdominis musculocutaneous (TRAM) flap
- The Free Transverse Rectus Abdominis Myocutaneous(TRAM) Flap for Immediate Breast Reconstruction
- Breast Reconstruction with Free Transverse Rectus Abdominis Myocutaneous Flap Complicated by Deep Vein Thrombosis-associated Pulmonary Thrombo-embolism
- Various Abdominal Flaps for Breast Reconstruction: Pedicled TRAM, Free TRAM, Muscle-sparing TRAM, DIEP, and SIEA Flaps
- Breast Reconstruction Using the Pedicled Transverse Rectus Abdominis Myocutaneous (Tram) Flap