J Korean Med Assoc.
2008 Jan;51(1):45-52.
Stereotactic Body Radiation Therapy
- Affiliations
-
- 1Department of Radiation Oncology, Korea Institute of Radiological and Medical Sciences, Korea. mskim@kcch.re.kr
Abstract
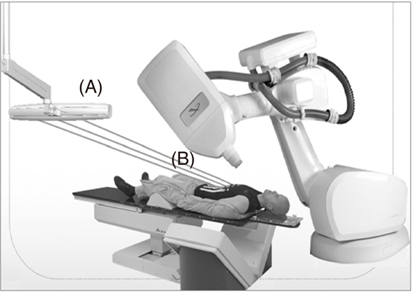
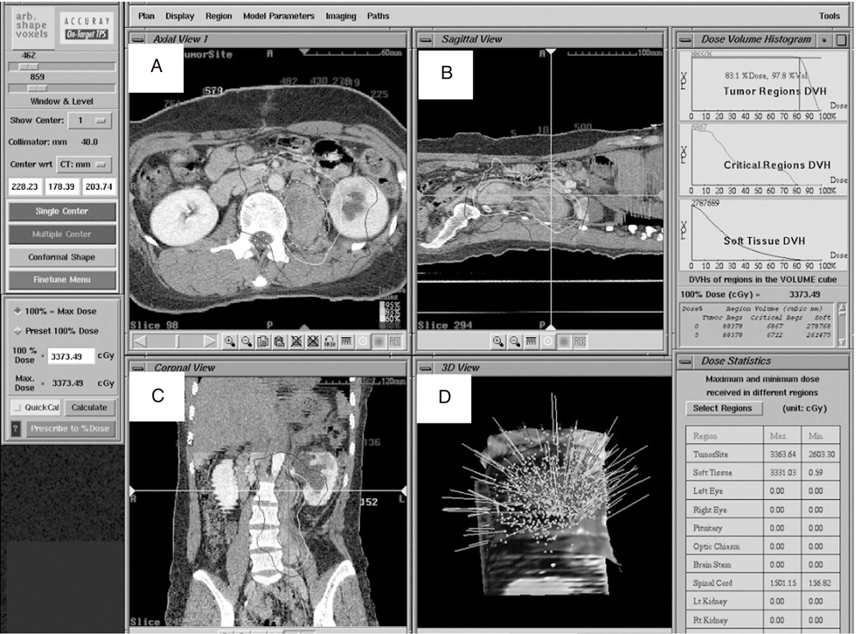
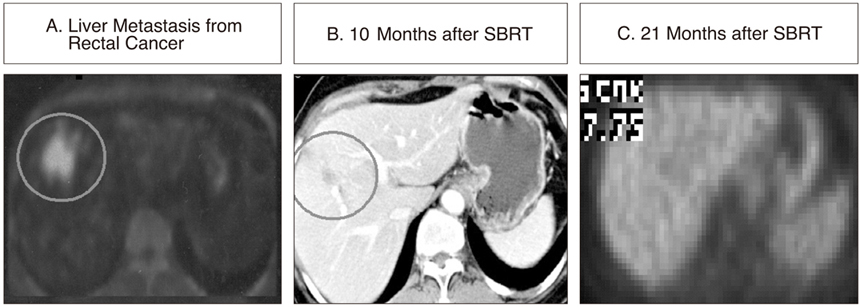
- Stereotactic Body Radiation Therapy (SBRT) is extracranial stereotactic radiosurgery or stereotactic radiation therapy, a newly emerging radiotherapy treatment method to deliver a high dose of radiation to the target, utilizing either a single dose or a small number of fractions with a high degree of precision within the body. The ability to deliver a single or a few fractions of high-dose ionizing radiation with a high targeting accuracy and rapid dose falloff gradients encompassing tumors with a patient provides the basis for the development of SBRT. A few fractions, the use of fiducial as a marker, image guidance and multiple radiation beam, and gating through a skin marker are unique technologies as compared to the conventional fractionated radiotherapy. The most common sites for these treatments are lung and liver, which are considered to parallel organs at risk. Recently, it was confirmed that prostate, spinal/paraspinal, head and neck, and pancreas tumors could be new candidates for these novel treatments. The preliminary reports show promising results with a relatively low complication rate. This article provides an overview of SBRT, the indication, descriptions of method including radiation dose and fraction size, the clinical data of lung and liver tumor, and discussions on potential areas of future investigations.
MeSH Terms
Figure
Reference
-
1. Nagata Y, Matsuo Y, Takayama K, Norkhisa Y, Mizowaki T, Mitumori M, Shibuya K, Yano S, Narita Y, Hiraoka M. Current status of stereotactic body radiotherapy for lung cancer. Int J Clin Oncol. 2007. 12:3–7.
Article2. D'Souza WD, Nazareth DP, Zhang B, Ewyoung C, Suntharalingam M, Kwok Y, Yu CX, Regine WF. The use of gated and 4D CT imaging in planning for stereotactic body radiation therapy. Med Dosi. 2007. 32:92–101.3. Kavanagh BD, Scheftera TE, Wersall PJ. Liver, renal and retroperitoneal tumors:stereotactic radiotherapy. Front Radiat Ther Oncol. 2007. 40:415–426.4. Fowler JF, Tome WA, Welsh JS. Kavanagh BD, Tirnmerman RD, editors. The radiobiology of stereotactic body radiation therapy (SBRT). Stereotactic Body Radiation Therapy. 2004. 1st ed. Philadelphia: Lippincott Williams & Wilkins;7–14.5. Uematsu M, Shioda A, Suda A, Fukui T, Ozeki Y, Wong JR, Kusano S. Computed tomography-guided frameless stereotactic radiotherapy for stage I non-small-cell lung cancer: a 5-year experience. Int J Radiat Oncol Biol Phys. 2001. 51:666–670.
Article6. Nagata Y, Negoro Y, Aoki T, Mizowaki T, Takayama K, Kokubo M, Araki N, Mitsumori M, Sasai K, Shibamoto Y, Koga S, Yano S, Hiraoka M. Clinical outcomes of 3D conformal hypofractionated single high-dose radiotherapy for one or two lung tumors using a stereotactic body frame. Int J Radiat Oncol Biol Phys. 2002. 52:1041–1046.
Article7. Hara R, Itami J, Kondo T, Aruga T, Abe Y, Ito M, Fuse M, Shinohara D, Nagaoka T, Kobiki T. Stereotactic single high dose irradiation of lung tumors under respiratory gating. Radiother Oncol. 2002. 63:159–163.
Article8. Onishi H, Araki T, Shirato H, Nagata Y, Hiraoka M, Gomi K, Yamashita T, Niibe Y, Karasawa K, Hayakawa K, Takai Y, Kimura T, Hirokawa Y, Takeda A, Ouchi A, Hareyama M, Kokubo M, Hara R, Itami J, Yamada K. Stereotactic hypofractionated high-dose irradiation for stage I non-small cell lung carcinoma: clinical outcomes in 245 subjects in a Japanese multiinstitutional study. Cancer. 2004. 101:1623–1631.
Article9. Lee SW, Choi EK, Park HJ, Ahn SD, Kim JH, Kim KJ, Yoon SM, Kim YS, Yi BY. Stereotactic body frame based fractionated radiosurgery on consecutive days for primary or metastatic tumors in the lung. Lung Cancer. 2003. 40:309–315.
Article10. Nesbitt JC, Putnam JB Jr, Walsh GL, Roth JA, Mountain CF. Survival in early stage non-small cell lung cancer. Ann Thorac Surg. 1995. 60:466–472.11. Fry WA, Menck HR, Winchester DP. The National cancer data base report on lung cancer. Cancer. 1996. 77:1947–1955.
Article12. Wingo PA, Tong T, Bolden S. Cancer statistics, 1995. CA Cancer J Clin. 1995. 45:8–30.
Article13. Blomgren H, Lax I, Naslund I, Svanstrom R. Stereotactic high dose fraction radiation therapy of extracranial tumors using an accelerator. Acta Oncolgica. 1995. 34:861–870.
Article14. Nakagawa K, Aoki Y, Tago M, Terahara A, Ohtomo K. Megavoltage CT-assisted stereotactic radiosurgery for thoracic tumors: original research in the treatment of thoracic neoplasms. Int J Radiat Oncol Biol Phys. 2000. 48:449–457.
Article15. Wulf J, Hädinger U, Oppitz U, Thiele W, Ness-Dourdoumas R, Flentje M. Stereotactic radiotherapy of targets in the lung and liver. Strahlenther Onkol. 2001. 177:645–655.
Article16. Timmerman R, Papiez L, McGarry R, Likes L, DesRosiers C, Frost S, Williams M. Extracranial stereotactic radioablation: results of a phase I study in medically inoperable stage I non-small cell lung cancer. Chest. 2003. 124:1946–1955.17. Hof H, Herfarth KK, Münter M, Hoess A, Motsch J, Wannenmacher M, Debus JJ. Stereotactic single dose radiotherapy of stage I non-small-cell lung cancer. Int J Radiat Oncol Biol Phys. 2003. 56:335–341.
Article18. Hawkins MA, Dawson LA. Radiation therapy for hepatocellular carcinoma from palliation to cure. Cancer. 2006. 15:1653–1663.19. Blomgren H, Lax I, Näslund I, Svanstörm R. Stereotactic high dose fraction radiation therapy of extracranial tumors using an accelerator. Clinical experience of the first thirty one patients. Acta Oncol. 1995. 34:861–870.
Article20. Lunsford LD, Flickinger JC, Larson D. Radiosurgery for tumors in the body: clinical experience using a new method. J Radiosurg. 1998. 1:63–74.
Article21. Herfarth KK, Debus J, Lohr F, Bahner ML, Rhein B, Fritz P, Höss A, Schlegel W, Wannenmacher MF. Stereotactic single-dose radiation therapy of liver tumors: results of a phase I/II trial. J Clin Oncol. 2001. 19:164–170.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Stereotactic Body Radiotherapy for Early Stage Lung Cancer
- Role of Radiation Therapy for Non-small Cell Lung Cancer: Focused on Stereotactic Ablative Radiation Therapy in Stage I
- Stereotactic body radiation therapy for pancreatic cancer: a potential ally in the era of immunotherapy?
- Stereotactic Body Radiation Therapy for Hepatocellular Carcinoma
- Stereotactic body radiotherapy for solitary spine metastasis