J Korean Neurosurg Soc.
2014 Sep;56(3):224-229. 10.3340/jkns.2014.56.3.224.
Long-Term Clinical and Radiologic Outcomes of Minimally Invasive Posterior Cervical Foraminotomy
- Affiliations
-
- 1Department of Neurosurgery, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea. neuriac@skku.edu
- KMID: 2339961
- DOI: http://doi.org/10.3340/jkns.2014.56.3.224
Abstract
OBJECTIVE
To report long-term clinical and radiological outcomes of minimally invasive posterior cervical foraminotomy (MI-PCF) performed in patients with unilateral single-level cervical radiculopathy.
METHODS
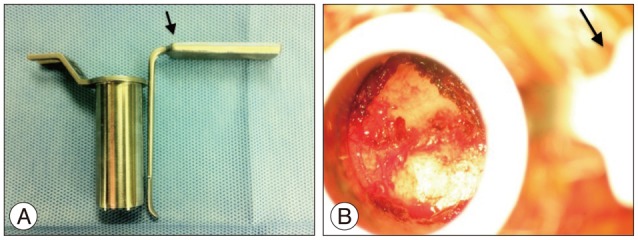
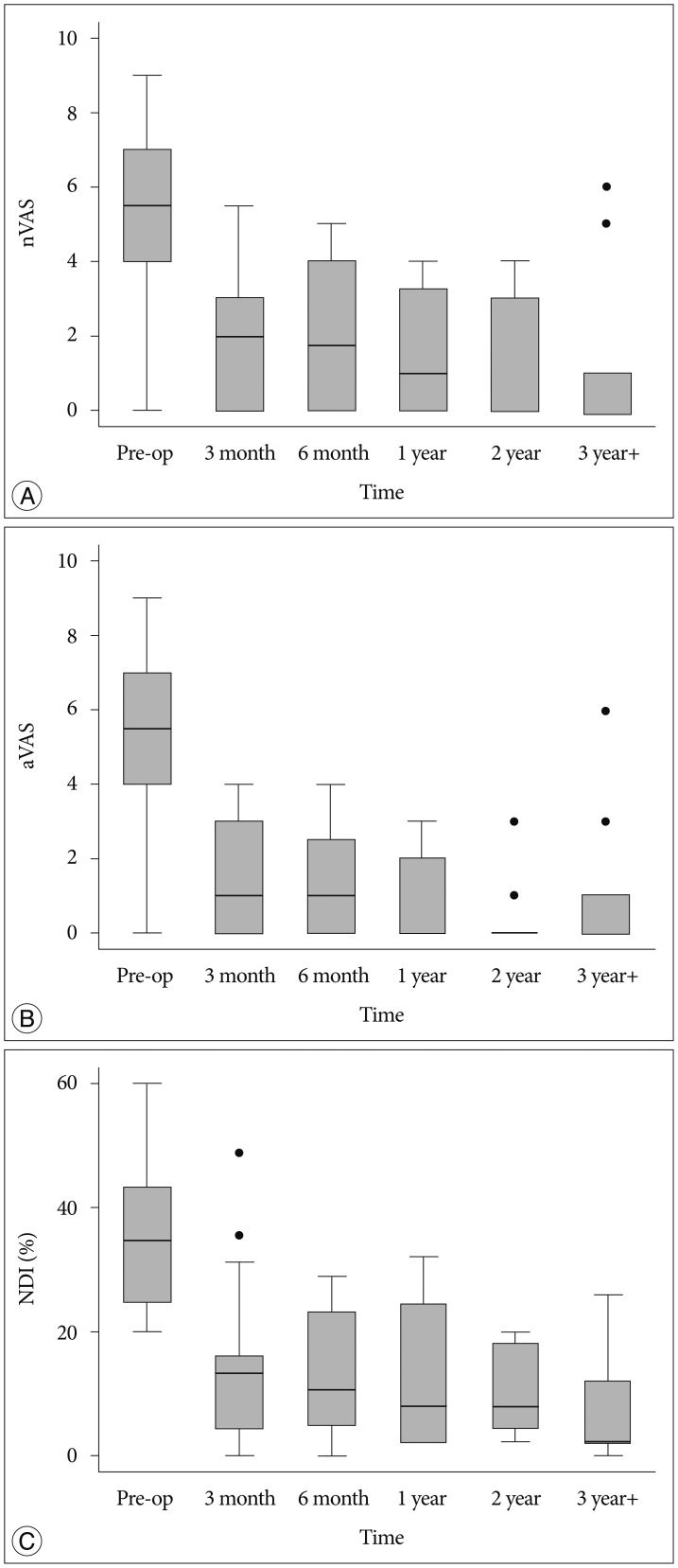
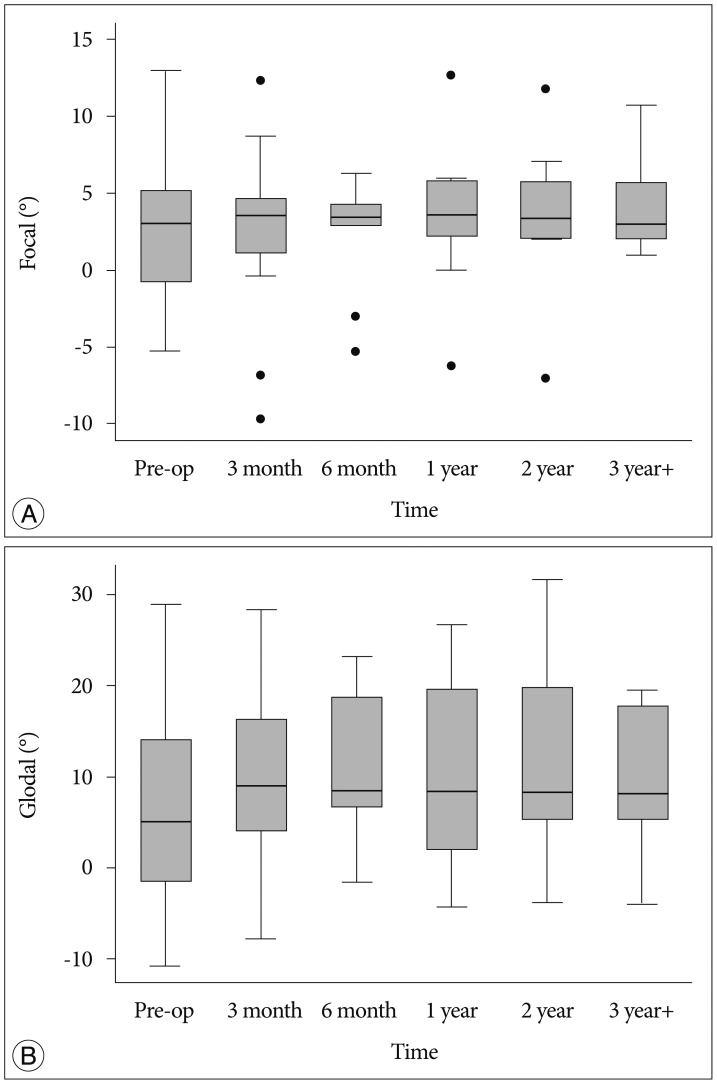
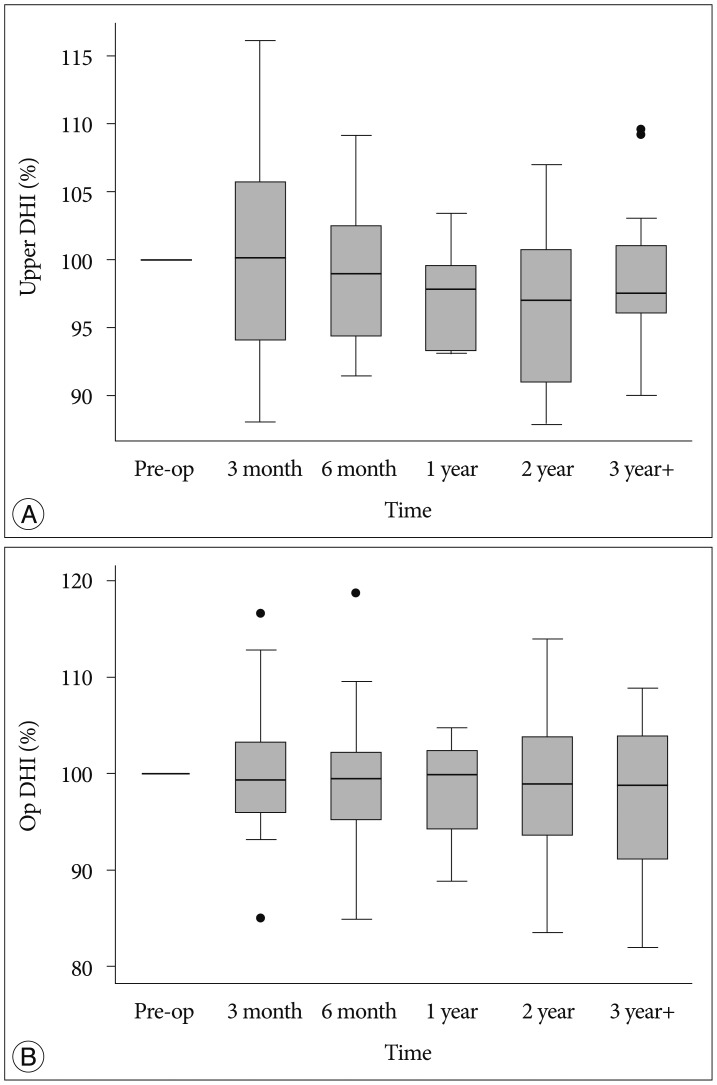
Of forty-six patients who underwent MI-PCF for unilateral single-level radiculopathy between 2005 and 2013, 33 patients were included in the study, with a mean follow-up of 32.7 months. Patients were regularly followed for clinical and radiological assessment. Clinical outcome was measured by visual analogue scale (VAS) for the neck/shoulder and arm, and the neck disability index (NDI). Radiological outcome was measured by focal/global angulation and disc height index (DHI). Outcomes after MI-PCF were evaluated as changes of clinical and radiological parameters from the baseline. Mixed effect model with random patients' effect was used to test for differences in the clinical and radiological parameters repeat measures.
RESULTS
There were no complications and all patients had an uneventful recovery during the early postoperative period. VAS scores for neck/shoulder and arm improved significantly in the early postoperative period (3 months) and were maintained with time (p<0.001). NDI improved significantly post-operatively and tended to decrease gradually during the follow-up period (p<0.001). There were no statistically significant changes in focal and global angulation at follow-up. Percent DHIs of the upper adjacent or operated disc were maintained without significant changes with time. During the follow-up, same site recurrence was not noted and adjacent segment disease requiring additional surgery occurred in two patients (6%) on the contra-lateral side.
CONCLUSION
MI-PCF provides long-term pain relief and functional restoration, accompanied by good long-term radiological outcome.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Long-Term Outcome of Posterior Cervical Inclinatory Foraminotomy
Juneyoung Heo, Jae Chil Chang, Hyung-Ki Park
J Korean Neurosurg Soc. 2016;59(4):374-378. doi: 10.3340/jkns.2016.59.4.374.
Reference
-
1. Adamson TE. Microendoscopic posterior cervical laminoforaminotomy for unilateral radiculopathy : results of a new technique in 100 cases. J Neurosurg. 2001; 95(1 Suppl):51–57. PMID: 11453432.
Article2. Cağlar YS, Bozkurt M, Kahilogullari G, Tuna H, Bakir A, Torun F, et al. Keyhole approach for posterior cervical discectomy : experience on 84 patients. Minim Invasive Neurosurg. 2007; 50:7–11. PMID: 17546536.
Article3. Chang JC, Park HK, Choi SK. Posterior cervical inclinatory foraminotomy for spondylotic radiculopathy preliminary. J Korean Neurosurg Soc. 2011; 49:308–313. PMID: 21716632.
Article4. Clark JG, Abdullah KG, Steinmetz MP, Benzel EC, Mroz TE. Minimally invasive versus open cervical foraminotomy : a systematic review. Global Spine J. 2011; 1:9–14. PMID: 24353931.5. Clarke MJ, Ecker RD, Krauss WE, McClelland RL, Dekutoski MB. Same-segment and adjacent-segment disease following posterior cervical foraminotomy. J Neurosurg Spine. 2007; 6:5–9. PMID: 17233284.
Article6. Fessler RG, Khoo LT. Minimally invasive cervical microendoscopic foraminotomy : an initial clinical experience. Neurosurgery. 2002; 51(5 Suppl):S37–S45. PMID: 12234428.7. Fleiss JL. Reliability of measurement : The design and analysis of clinical experiments. Hoboken, NJ: John Wiley & Sons, Inc.;1999. p. 1–32.8. Foley KT, Smith MM. Microendoscopic discectomy. Tech Neurosurg. 1997; 3:301–307.9. Franzini A, Messina G, Ferroli P, Broggi G. Minimally invasive disc preserving surgery in cervical radiculopathies : the posterior microscopic and endoscopic approach. Acta Neurochir Suppl. 2011; 108:197–201. PMID: 21107959.10. Frykholm R. Deformities of dural pouches and strictures of dural sheaths in the cervical region producing nerve-root compression; a contribution to the etiology and operative treatment of brachial neuralgia. J Neurosurg. 1947; 4:403–413. PMID: 20260241.
Article11. Gala VC, O'Toole JE, Voyadzis JM, Fessler RG. Posterior minimally invasive approaches for the cervical spine. Orthop Clin North Am. 2007; 38:339–349. abstract v. PMID: 17629982.
Article12. Hosono N, Yonenobu K, Ono K. Neck and shoulder pain after laminoplasty. A noticeable complication. Spine (Phila Pa 1976). 1996; 21:1969–1973. PMID: 8883196.13. Inoue H, Ohmori K, Miyasaka K, Hosoe H. Radiographic evaluation of the lumbosacral disc height. Skeletal Radiol. 1999; 28:638–643. PMID: 10591927.
Article14. Jagannathan J, Sherman JH, Szabo T, Shaffrey CI, Jane JA. The posterior cervical foraminotomy in the treatment of cervical disc/osteophyte disease : a single-surgeon experience with a minimum of 5 years' clinical and radiographic follow-up. J Neurosurg Spine. 2009; 10:347–356. PMID: 19441994.
Article15. Kwon YJ. Early surgical results of minimally invasive posterior foraminotomy using tubular retractor for cervical radiculopathy. J Korean Soc Spine Surg. 2007; 14:67–72.
Article16. Lawton CD, Smith ZA, Lam SK, Habib A, Wong RH, Fessler RG. Clinical outcomes of microendoscopic foraminotomy and decompression in the cervical spine. World Neurosurg. 2014; 81:422–427. PMID: 23246739.
Article17. Lee H, Nicholson LL, Adams RD, Maher CG, Halaki M, Bae SS. Development and psychometric testing of Korean language versions of 4 neck pain and disability questionnaires. Spine (Phila Pa 1976). 2006; 31:1841–1845. PMID: 16845361.
Article18. Minamide A, Yoshida M, Yamada H, Nakagawa Y, Maio K, Kawai M, et al. Clinical outcomes of microendoscopic decompression surgery for cervical myelopathy. Eur Spine J. 2010; 19:487–493. PMID: 19956984.
Article19. Perez-Cruet MJ, Fessler RG, Perin NI. Review : complications of minimally invasive spinal surgery. Neurosurgery. 2002; 51(5 Suppl):S26–S36. PMID: 12234427.20. Scoville WB, Dohrmann GJ, Corkill G. Late results of cervical disc surgery. J Neurosurg. 1976; 45:203–210. PMID: 939979.
Article21. Scoville WB, Whitcomb BB. Lateral rupture of cervical intervertebral disks. Postgrad Med. 1966; 39:174–180. PMID: 5903648.
Article22. Skovrlj B, Gologorsky Y, Haque R, Fessler RG, Qureshi SA. Complications, outcomes, and need for fusion after minimally invasive posterior cervical foraminotomy and microdiscectomy. Spine J. 2014; [Epub ahead of print].
Article23. Vernon H, Mior S. The Neck Disability Index: a study of reliability and validity. J Manipulative Physiol Ther. 1991; 14:409–415. PMID: 1834753.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Posterior Endoscopic Cervical Discectomy
- Early Surgical Results of Minimally Invasive Posterior Foraminotomy using Tubular Retractor for Cervical Radiculopathy
- Fully-Endoscopic Posterior Cervical 2-Level Foraminotomy With Total Pediculectomy for Adjacent-Level Foraminal Stenosis in Severe Degenerative Spondylolisthesis: A Technical Note With 1-Year Follow-up
- Management of a Rare Case of C2–3 Cervical Foraminal Disc Herniation by Unilateral Biportal Endoscopic Foraminotomy
- Posterior Endoscopic Cervical Decompression: Review and Technical Note