J Korean Neurosurg Soc.
2012 Sep;52(3):250-253.
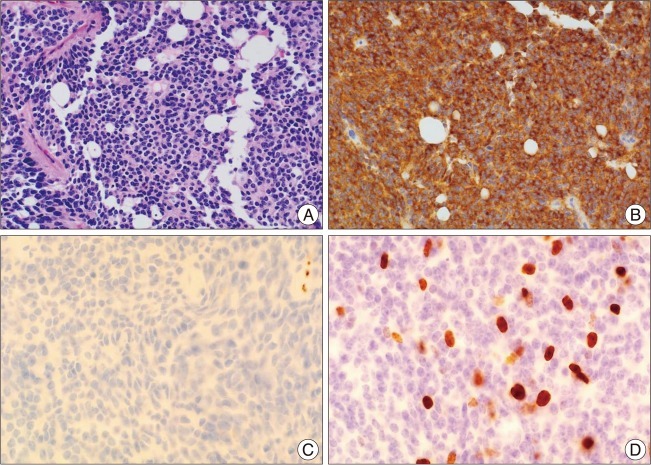
Cerebellar Liponeurocytoma with an Unusually Aggressive Histopathology : Case Report and Review of the Literature
- Affiliations
-
- 1Department of Neurosurgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. jilee@skku.edu
- 2Department of Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
Abstract
- We report a rare case of cerebellar liponeurocytoma with an unusually aggressive histopathology. A 49-year-old man presented with a four-month history of headache, vertigo, and progressive swaying gait. Magnetic resonance imaging showed a 3x3.5 cm sized relatively well-demarcated round mass lesion in the fourth ventricle, characterized by high signal intensity on T2-weighted images. Postcontrast images revealed strong enhancement of the solid portion and the cyst wall. The patient underwent suboccipital craniectomy and tumor removal. The pathologic diagnosis was cerebellar liponeurocytoma. Adjuvant radiotherapy was offered due to concerns related to the high proliferative index (Ki-67, 13.68%) of the tumor. At the last routine postoperative follow-up visit (12 months), the patient complained of no specific symptom and there was no evidence of tumor recurrence. However, long-term follow-up and the analysis of similar cases are necessary because of the low number of reports and the short follow-up of cases.
Keyword
MeSH Terms
Figure
Reference
-
1. Aker FV, Ozkara S, Eren P, Peker O, Armağan S, Hakan T. Cerebellar liponeurocytoma/lipidized medulloblastoma. J Neurooncol. 2005; 71:53–59. PMID: 15719276.
Article2. Alkadhi H, Keller M, Brandner S, Yonekawa Y, Kollias SS. Neuroimaging of cerebellar liponeurocytoma. Case report. J Neurosurg. 2001; 95:324–331. PMID: 11780904.3. Bechtel JT, Patton JM, Takei Y. Mixed mesenchymal and neuroectodermal tumor of the cerebellum. Acta Neuropathol. 1978; 41:261–263. PMID: 206094.
Article4. Buccoliero AM, Caldarella A, Bacci S, Gallina P, Taddei A, Di Lorenzo N, et al. Cerebellar liponeurocytoma : morphological, immunohistochemical, and ultrastructural study of a relapsed case. Neuropathology. 2005; 25:77–83. PMID: 15822821.
Article5. Cacciola F, Conti R, Taddei GL, Buccoliero AM, Di Lorenzo N. Cerebellar liponeurocytoma. Case report with considerations on prognosis and management. Acta Neurochir (Wien). 2002; 144:829–833. PMID: 12181694.6. Châtillon CE, Guiot MC, Roberge D, Leblanc R. Cerebellar liponeurocytoma with high proliferation index : treatment options. Can J Neurol Sci. 2009; 36:658–661. PMID: 19831140.
Article7. Davis DG, Wilson D, Schmitz M, Markesbery WR. Lipidized medulloblastoma in adults. Hum Pathol. 1993; 24:990–995. PMID: 8068063.
Article8. Giangaspero F, Cenacchi G, Roncaroli F, Rigobello L, Manetto V, Gambacorta M, et al. Medullocytoma (lipidized medulloblastoma). A cerebellar neoplasm of adults with favorable prognosis. Am J Surg Pathol. 1996; 20:656–664. PMID: 8651344.9. González-Cámpora R, Weller RO. Lipidized mature neuroectodermal tumour of the cerebellum with myoid differentiation. Neuropathol Appl Neurobiol. 1998; 24:397–402. PMID: 9821171.
Article10. Horstmann S, Perry A, Reifenberger G, Giangaspero F, Huang H, Hara A, et al. Genetic and expression profiles of cerebellar liponeurocytomas. Brain Pathol. 2004; 14:281–289. PMID: 15446583.
Article11. Jackson TR, Regine WF, Wilson D, Davis DG. Cerebellar liponeurocytoma. Case report and review of the literature. J Neurosurg. 2001; 95:700–703. PMID: 11596966.12. Jenkinson MD, Bosma JJ, Du Plessis D, Ohgaki H, Kleihues P, Warnke P, et al. Cerebellar liponeurocytoma with an unusually aggressive clinical course : case report. Neurosurgery. 2003; 53:1425–1427. discussion 1428. PMID: 14633310.13. Kleihues P, Louis DN, Scheithauer BW, Rorke LB, Reifenberger G, Burger PC, et al. The WHO classification of tumors of the nervous system. J Neuropathol Exp Neurol. 2002; 61:215–225. discussion 226-229. PMID: 11895036.
Article14. Orlandi A, Marino B, Brunori M, Greco R, Spagnoli LG. Lipomatous medulloblastoma. Clin Neuropathol. 1997; 16:175–179. PMID: 9266140.15. Owler BK, Makeham JM, Shingde M, Besser M. Cerebellar liponeurocytoma. J Clin Neurosci. 2005; 12:326–329. PMID: 15851097.
Article16. Soylemezoglu F, Soffer D, Onol B, Schwechheimer K, Kleihues P. Lipomatous medulloblastoma in adults. A distinct clinicopathological entity. Am J Surg Pathol. 1996; 20:413–418. PMID: 8604807.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Aneurysm of Distal Posterior Inferior Cerebellar Artery:Case Report with Review of the Literature
- Cerebellar Glioblastoma Presenting as a Cerebellar Hemorrhage in a Child
- Giant cerebellar cavernous malformation in children: A case report and literature review
- Capillary Telangiectasia of the Posterior Fossa Presenting with Repeated Cerebellar Hemorrhage
- Cerebellopontine Angle Medulloblastoma: Case Report