J Korean Ophthalmol Soc.
2014 Jul;55(7):1115-1120.
A Case of Ocular Syphilis Presenting as Bilateral Optic Neuritis
- Affiliations
-
- 1Department of Ophthalmology, Jeju National University School of Medicine, Jeju, Korea. amario@naver.com
- 2Department of Surgery, Jeju National University School of Medicine, Jeju, Korea.
Abstract
- PURPOSE
To report a case of ocular syphilis presenting as bilateral optic neuritis.
CASE SUMMARY
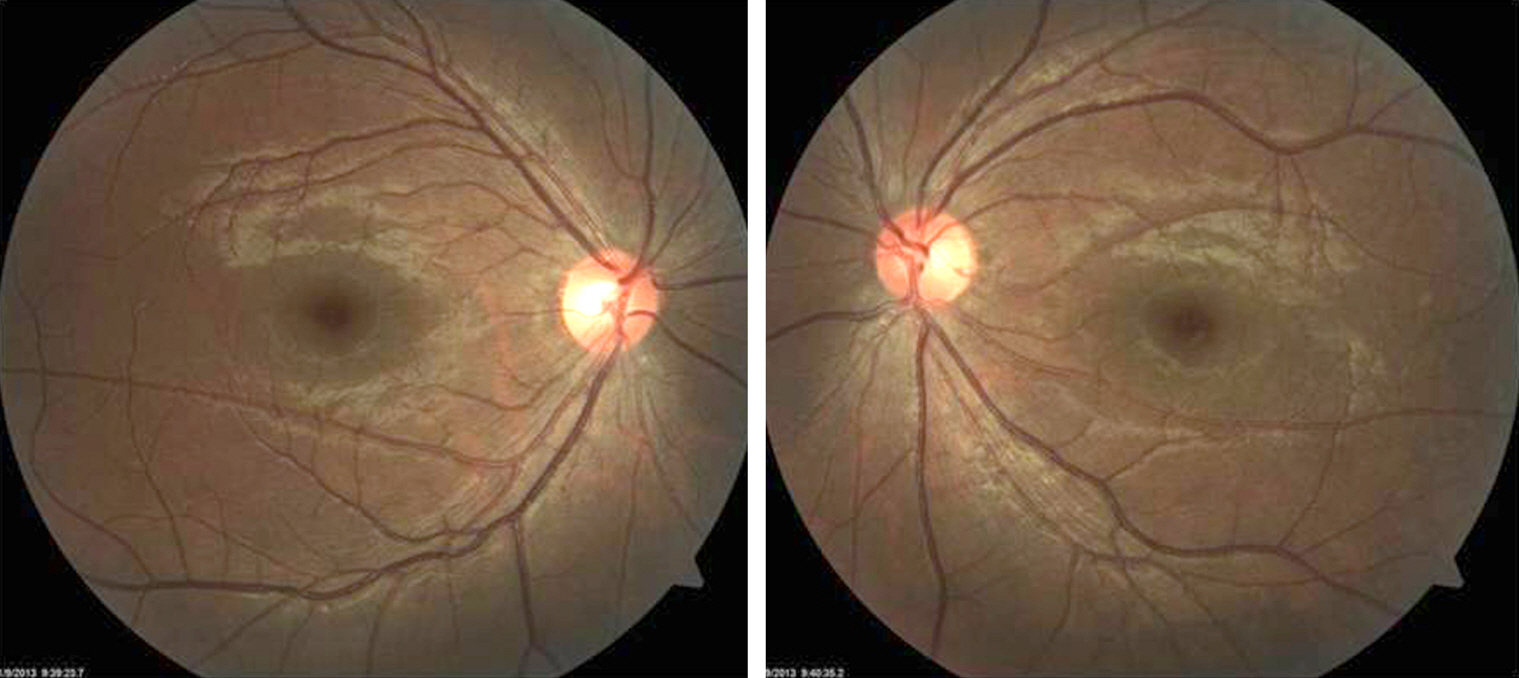
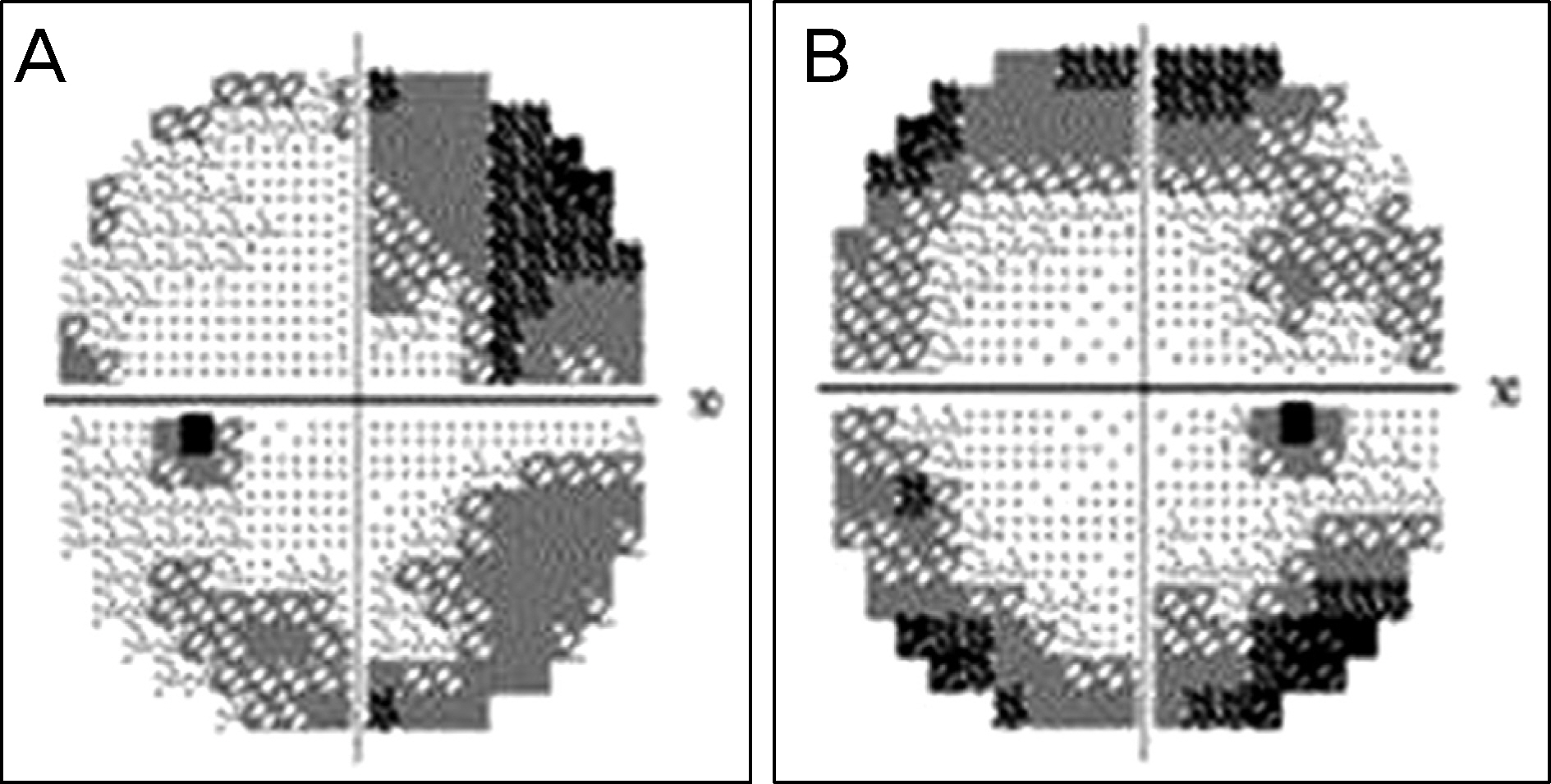
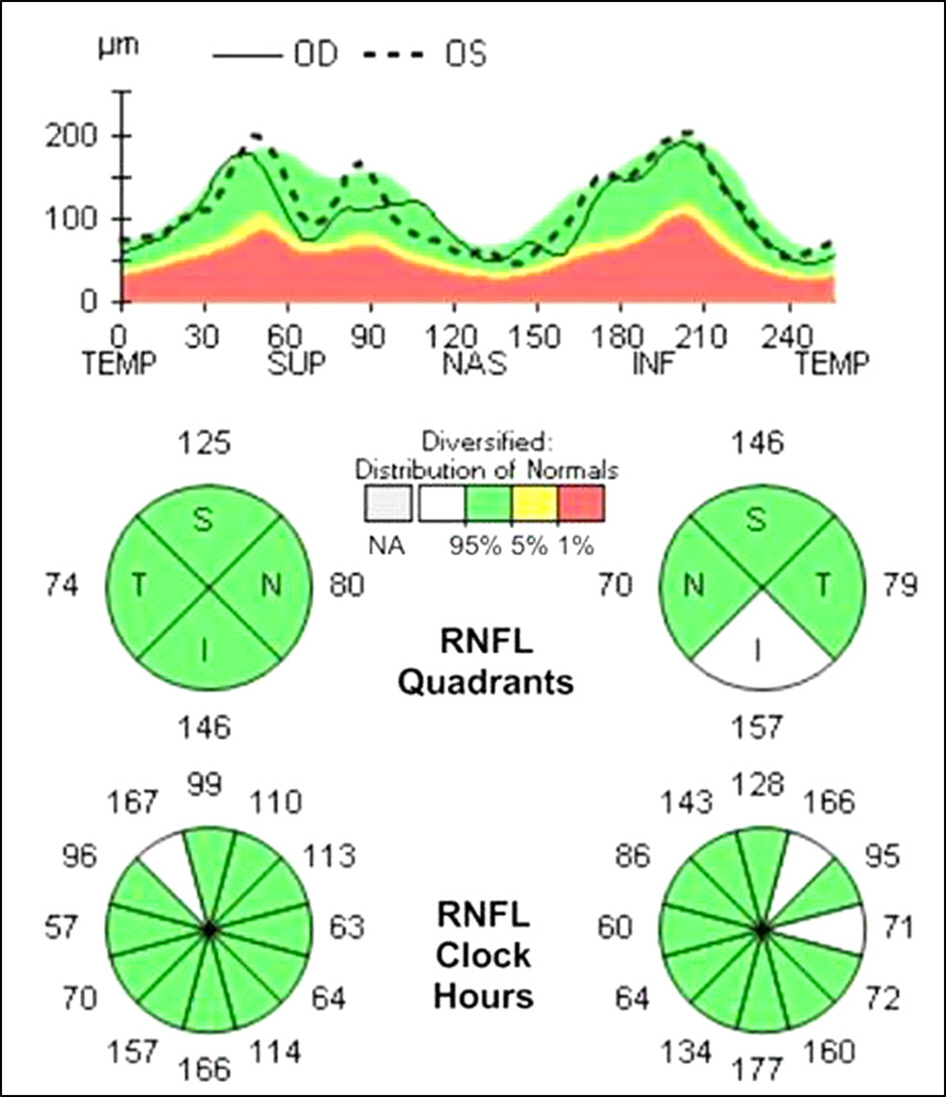
A 25-year-old man presented with visual difficulty in both eyes that had begun 2 weeks previously. Best corrected visual acuity was 0.7 in the right eye and 0.1 in the left eye. Anterior segment was normal. On fundoscopic examination, optic disc swelling was found in both eyes. Color vision was abnormal in the left eye. The visual field (VF) showed peripheral constriction in the right eye and generalized reduction in the left eye. Fluorescein angiography revealed early, bilateral leakage of dye from the optic disc with multiple hot spots in the chorioretinal level. Serology was positive for fluorescent treponemal antibody absorbance (FTA-ABS) IgM, IgG and rapid plasma reagin test. A test of the cerebrospinal fluid was positive for venereal diseases research laboratory and FTA-ABS IgG. A diagnosis of syphilitic optic neuritis was made and the patient was treated with antibiotics. Six months later, visual acuity was 1.0 in the right eye and 0.8 in the left eye. There was no disc swelling on both fundoscopy and optical coherence tomographs. VF also improved after treatment, with the restoration of central vision.
CONCLUSIONS
Syphilis can present as optic neuritis. Clinicians should consider serologic examination for syphilis and then initiate appropriate antibiotic treatment.
MeSH Terms
-
Adult
Anti-Bacterial Agents
Cerebrospinal Fluid
Color Vision
Constriction
Diagnosis
Fluorescein Angiography
Humans
Immunoglobulin G
Immunoglobulin M
Neurosyphilis
Optic Neuritis*
Papilledema
Plasma
Sexually Transmitted Diseases
Syphilis*
Treponema pallidum
Visual Acuity
Visual Fields
Anti-Bacterial Agents
Immunoglobulin G
Immunoglobulin M
Figure
Reference
-
References
1. Doris JP, Saha K, Jones NP, Sukthankar A. Ocular syphilis: the new epidemic. Eye (Lond). 2006; 20:703–5.
Article2. Gaudio PA. Update on ocular syphilis. Curr Opin Ophthalmol. 2006; 17:562–6.
Article3. Muldoon EG, Hogan A, Kilmartin D, et al. Syphilis consequences and implications in delayed diagnosis: five cases of secondary syphilis presenting with ocular symptoms. Sex Transm Infect. 2010; 86:512–3.
Article4. Bandettini di Poggio M, Primavera A, Capello E, et al. A case of secondary syphilis presenting as optic neuritis. Neurol Sci. 2010; 31:365–7.
Article5. Parker SE, Pula JH. Neurosyphilis presenting as asymptomatic optic perineuritis. Case Rep Ophthalmol Med. 2012; 2012:621872.
Article6. Lee JS, Lee SC, Lee MI, Kwon OW. Syphilitic neuroretinitis initially diagnosed as acute retinal necrosis: a report of two cases. J Korean Ophthalmol Soc. 1990; 31:1207–13.7. Kim EH, Lee JE. A case of vitritis as the primary manifestation without retinitis in ocular syphilis with AIDS. J Korean Ophthalmol Soc. 2006; 47:1177–82.8. Lee YH, Nam K, Kim JY. Cilioreitnal artery occlusion as the first clinical manifestation of ocular syphilis. J Korean Ophthalmol Soc. 2011; 52:1254–8.9. Hyun SH, Lee DY, Nam DH. A case of episcleritis as a manifestation of neurosyphilis. J Korean Ophthalmol Soc. 2013; 54:829–33.
Article10. Smith GT, Goldmeier D, Migdal C. Neurosyphilis with optic neuritis: an update. Postgrad Med J. 2006; 82:36–9.
Article11. Tamesis RR, Foster CS. Ocular syphilis. Ophthalmology. 1990; 97:1281–7.
Article12. Barile GR, Flynn TE. Syphilis exposure in patients with uveitis. Ophthalmology. 1997; 104:1605–9.
Article13. Kuo IC, Kapusta MA, Rao NA. Vitritis as the primary manifestation of ocular syphilis in patients with HIV infection. Am J Ophthalmol. 1998; 125:306–11.
Article14. Lorentzen SE. Syphilitic optic neuritis; A case report. Acta Ophthalmol. 1967; 45:769–72.15. Browning DJ. Posterior segment manifestations of active ocular syphilis, their response to a neurosyphilis regimen of penicillin therapy, and the influence of human immunodeficiency virus status on response. Ophthalmology. 2000; 107:2015–23.
Article16. Oh HG, Yang KI. A case of optic perineuritis associated with seronegative neurosyphilis. J Korean Geriatr Soc. 2007; 11:98–100.17. Miller NR, Newman NJ, BIousse V, Kerrison JB. Walsh and Hoyt's Clinical Neuro-Ophthalmology. 6th ed.3. Philadelphia: Lippincott Williams & Wilkins;2005. p. 3091–111.18. Parker JDJ. Uncommon complications of early syphilis: Hepatitis, periostitis, iritis with papillitis, and meningitis. Br J Vener Dis. 1972; 48:32–6.
Article19. Marra CM. Syphilis and human immunodeficiency virus; prevention and politics. Arch Neurol. 2004; 61:1505–8.20. Margo CE, Hamed LM. Ocular syphilis. Surv Ophthalmol. 1992; 37:203–20.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Neurosyphilis with Acute Optic Neuritis and Trochlear Nerve Palsy in Human Immunodeficiency Virus Infected Male
- Ocular Syphilis Presenting as both Optic Neuritis and Chorioretinitis in both Eyes
- Reversible Bilateral Optic Neuritis with No Light Perception
- Clinical Survey of 110 Cases of Optic Atrophy
- A Case of Bilateral Optic Neuritis in Tsutsugamushi Infection