J Korean Ophthalmol Soc.
2014 Apr;55(4):498-505.
The Difference in Filaments between Corneal Occlusion and Keratoconjunctivitis Sicca
- Affiliations
-
- 1Department of Ophthalmology, Chung-Ang University College of Medicine, Seoul, Korea. jck50ey@kornet.net
Abstract
- PURPOSE
To examine histopathological findings of filamentary keratitis due to corneal occlusion.
METHODS
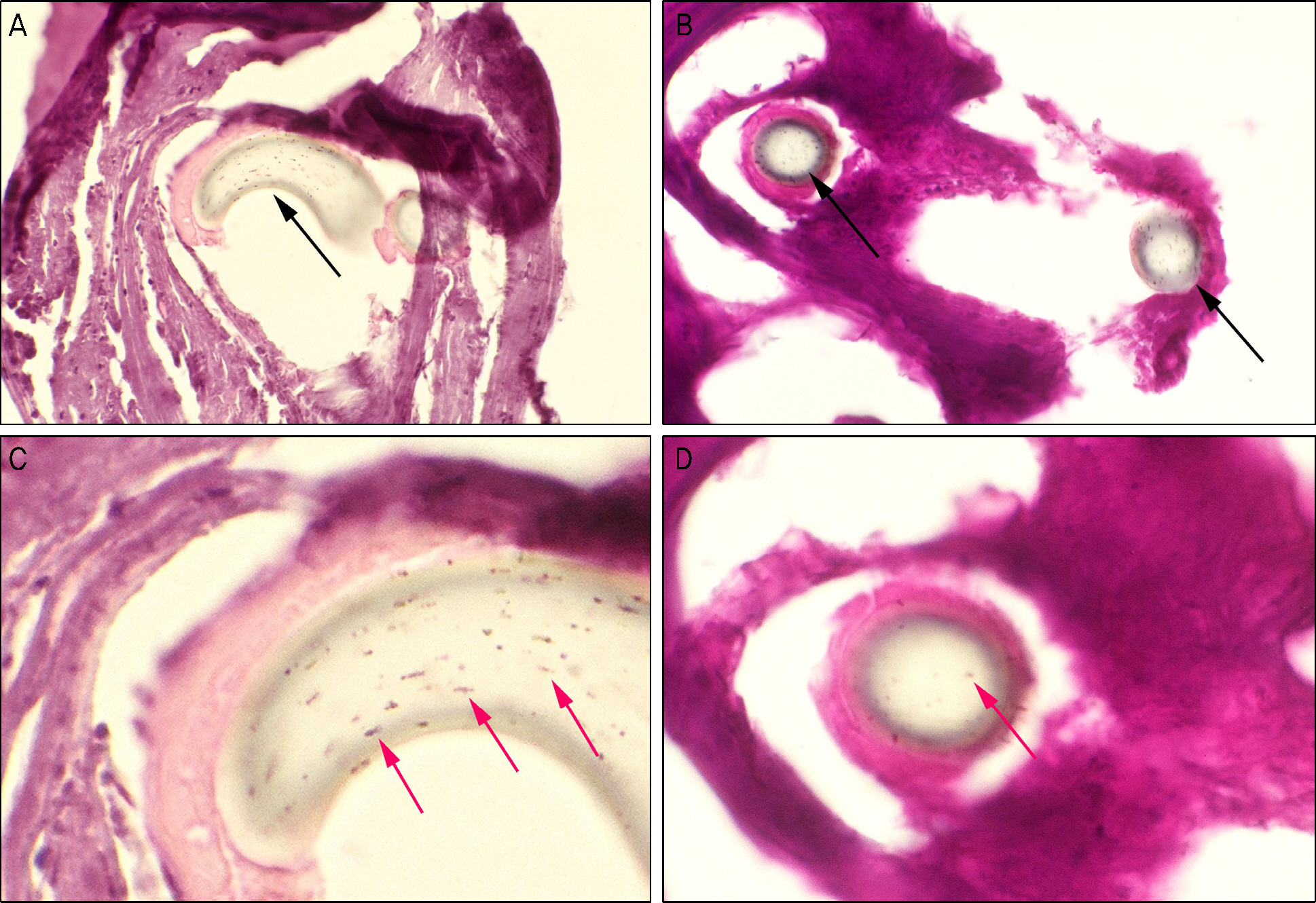
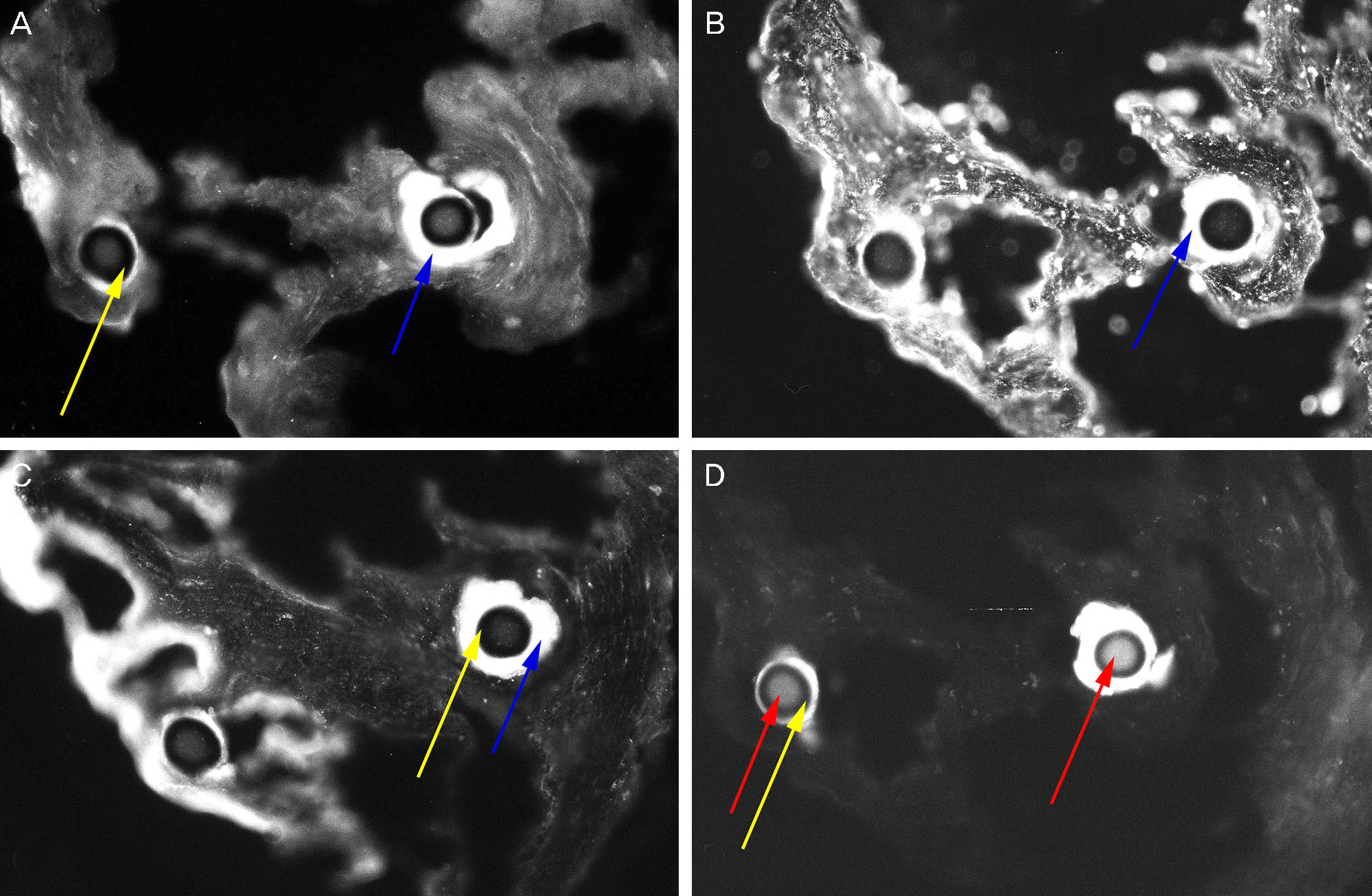
We analyzed filamentary keratitis in 11 eyes with corneal occlusion due to blepharospasm, ptosis and paralytic strabismus, 11 eyes with keratoconjunctivitis sicca, and 13 eyes with both corneal occlusion and keratoconjunctivitis sicca. The following protocols were used for filament analyses: slit lamp examination for counting filament numbers, impression cytology for grading mucin content, and histopathology (hematoxylin and eosin staining) and immunohistochemistry (with AE1/AE3, MUC1, 5AC, 16) for histological analysis.
RESULTS
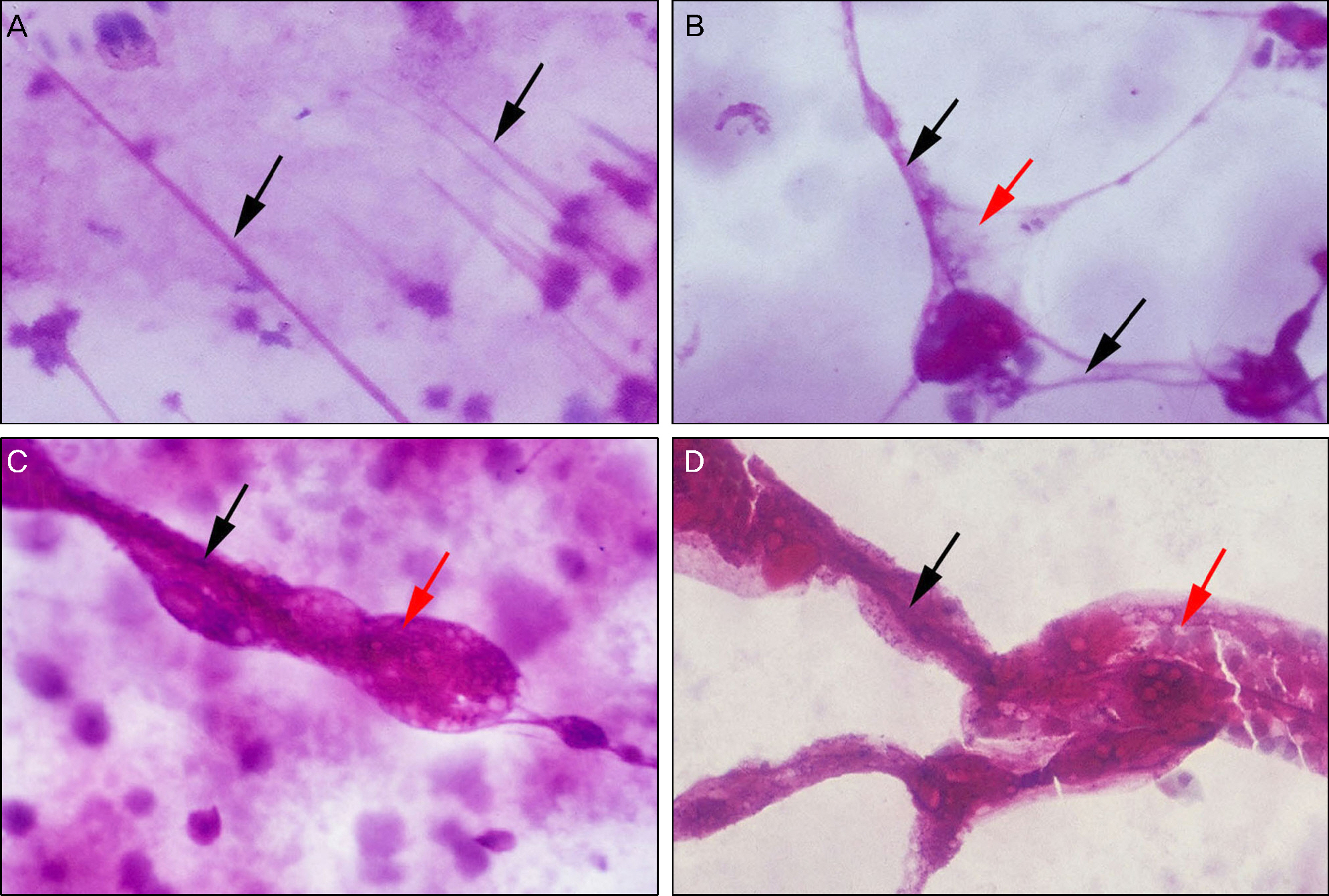
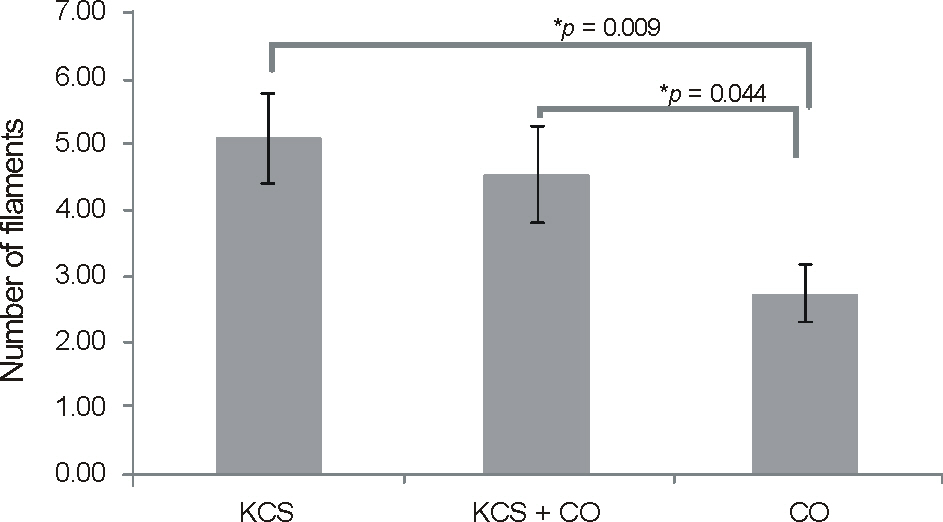
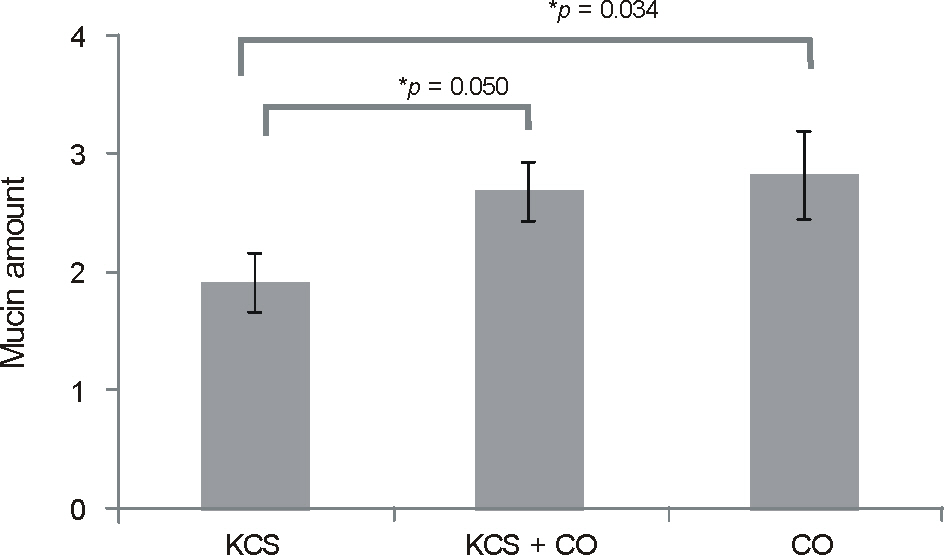
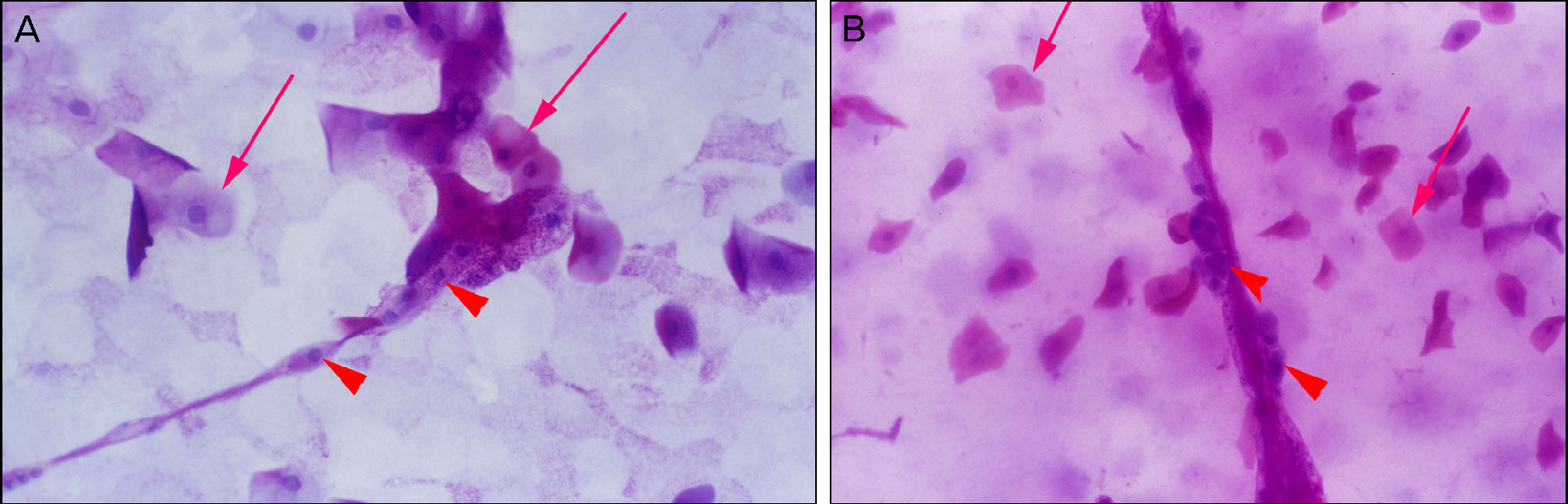
Slit lamp biomicrosopy showed a significantly smaller number of filaments in the corneal occlusion group (11 eyes, 2.7 +/- 1.4) than the keratoconjunctivitis sicca group (11 eyes, 5.1 +/- 2.2, p = 0.009). In impression cytology, the standard photograph grade of mucin content was significantly higher in the corneal occlusion group (2.7 +/- 0.9) than the keratoconjunctivitis sicca group (1.9 +/- 0.8, p = 0.034). On pathological exam, filaments showed a central filament with peripheral mucin. The central filaments were composed of core and cortex, and the core contained multiple deformed nuclei. However, the cortex was not stained by AE1/AE3, MUC1, 5AC, 16.
CONCLUSIONS
Filamentary keratitis due to corneal occlusion showed a smaller number of filaments and higher mucin content than filamentary keratitis induced by keratoconjunctivitis sicca and should be considered during treatment.
MeSH Terms
Figure
Reference
-
References
1. Beetham WP. Filamentary Keratitis. Trans Am Ophthalmol Soc. 1935; 33:413–35.2. Wright P. Filamentary keratitis. Trans Ophthalmol Soc U K. 1975; 95:260–6.3. Albietz J, Sanfilippo P, Troutbeck R, Lenton LM. Management of filamentary keratitis associated with aqueous-deficient dry eye. Optom Vis Sci. 2003; 80:420–30.
Article4. Diller R, Sant S. A case report and review of filamentary keratitis. Optometry. 2005; 76:30–6.
Article5. Kakizaki H, Zako M, Mito H, Iwaki M. Filamentary keratitis improved by blepharoptosis surgery: two cases. Acta Ophthalmol Scand. 2003; 81:669–71.
Article6. Tanioka H, Yokoi N, Komuro A, et al. Investigation of the corneal filament in filamentary keratitis. Invest Ophthalmol Vis Sci. 2009; 50:3696–702.
Article7. Choi SK, Paek NH, Hong WS. Clinical observation of the filamentary keratitis. J Korean Ophthalmol Soc. 1974; 15:323–6.8. Unal M, Sarici A. Filamentary keratopathy caused by corneal occlusion by large-angle paralytic strabismus. Cornea. 2006; 25:1105–6.9. Scott AB, Kennedy RA, Stubbs HA. Botulinum A toxin injection as a treatment for blepharospasm. Arch Ophthalmol. 1985; 103:347–50.
Article10. Berke RN. Congenital ptosis; a classification of 200 cases. Arch Ophthal. 1949; 41:188–97.11. Gilbard JP, Farris RL, Santamaria J 2nd. Osmolarity of tear micro-volumes in keratoconjunctivitis sicca. Arch Ophthalmol. 1978; 96:677–81.
Article12. Gao J, Schwalb TA, Addeo JV, et al. The role of apoptosis in the pathogenesis of canine keratoconjunctivitis sicca: the effect of topical Cyclosporin A therapy. Cornea. 1998; 17:654–63.13. Fox RI, Chan R, Michelson JB, et al. Beneficial effect of artificial tears made with autologous serum in patients with keratoconjunctivitis sicca. Arthritis Rheum. 1984; 27:459–61.
Article14. Baum JL. The Castroviejo Lecture. Prolonged eyelid closure is a risk to the cornea. Cornea. 1997; 16:602–11.15. Good WV, Whitcher JP. Filamentary keratitis caused by corneal occlusion in large-angle strabismus. Ophthalmic Surg. 1992; 23:66.
Article16. Merjava S, Neuwirth A, Tanzerova M, Jirsova K. The spectrum of cytokeratins expressed in the adult human cornea, limbus and per-ilimbal conjunctiva. Histol Histopathol. 2011; 26:323–31.17. Moore JC, Tiffany JM. Human ocular mucus. Chemical studies. Exp Eye Res. 1981; 33:203–12.
Article18. Argüeso P, Spurr-Michaud S, Russo CL, et al. MUC16 mucin is expressed by the human ocular surface epithelia and carries the H185 carbohydrate epitope. Invest Ophthalmol Vis Sci. 2003; 44:2487–95.19. Inatomi T, Spurr-Michaud S, Tisdale AS, Gipson IK. Human corneal and conjunctival epithelia express MUC1 mucin. Invest Ophthalmol Vis Sci. 1995; 36:1818–27.20. Inatomi T, Spurr-Michaud S, Tisdale AS, et al. Expression of secre-tory mucin genes by human conjunctival epithelia. Invest Ophthalmol Vis Sci. 1996; 37:1684–92.21. Absolon MJ, Brown CA. Acetylcysteine in keratoconjunctivitis sicca. Br J Ophthalmol. 1968; 52:310–6.
Article22. Hamilton W, Wood TO. Filamentary keratitis. Am J Ophthalmol. 1982; 93:466–9.
Article23. Fayet B, Bernard JA, Ammar J, et al. Treatment of dry eye by tem-porary punctum plug. Comparison with a control group. J Fr Ophtalmol. 1990; 13:123–33.24. Tuberville AW, Frederick WR, Wood TO. Punctal occlusion in tear deficiency syndromes. Ophthalmology. 1982; 89:1170–2.
Article25. Gumus K, Lee S, Yen MT, Pflugfelder SC. Botulinum toxin injection for the management of refractory filamentary keratitis. Arch Ophthalmol. 2012; 130:446–50.
Article26. Kitazawa K, Yokoi N, Watanabe A, et al. Eyelid surgery for refractory filamentary keratitis. Nihon Ganka Gakkai Zasshi. 2011; 115:693–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Keratoconjunctivitis Sicca Associated Idiopathic Hypereosinophilic Syndrome
- Ocular Manifestations of Systemic Lupus Erythematosus
- Sjogren's Syndrome
- Microvascular autologous submandibular gland transplantation in severe cases of keratoconjunctivitis sicca
- Amblyopia and Strabismus by Monocular Corneal Opacity Following Suspected Epidemic Keratoconjunctivitis in Infancy