J Korean Ophthalmol Soc.
2014 Jan;55(1):138-142.
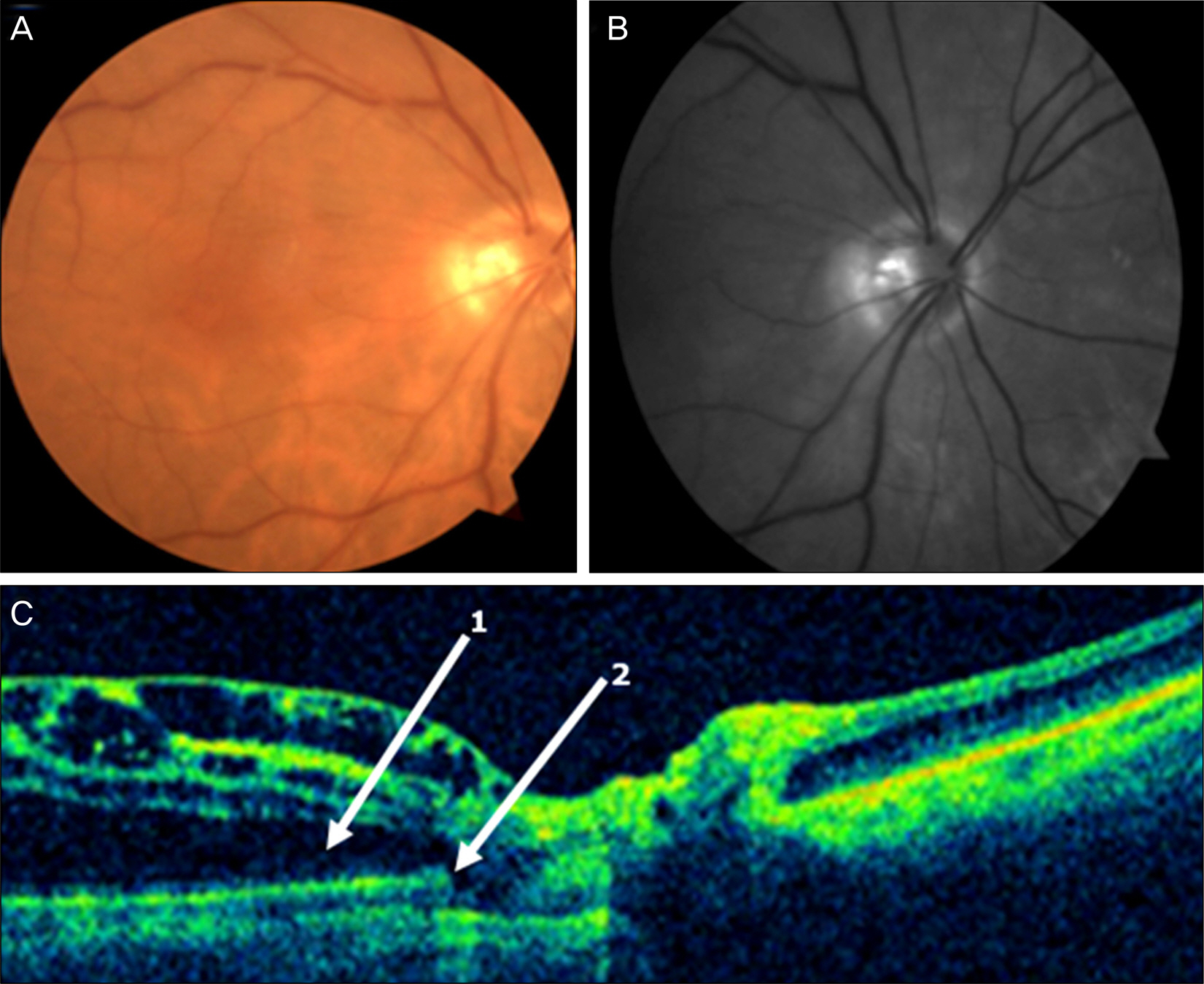
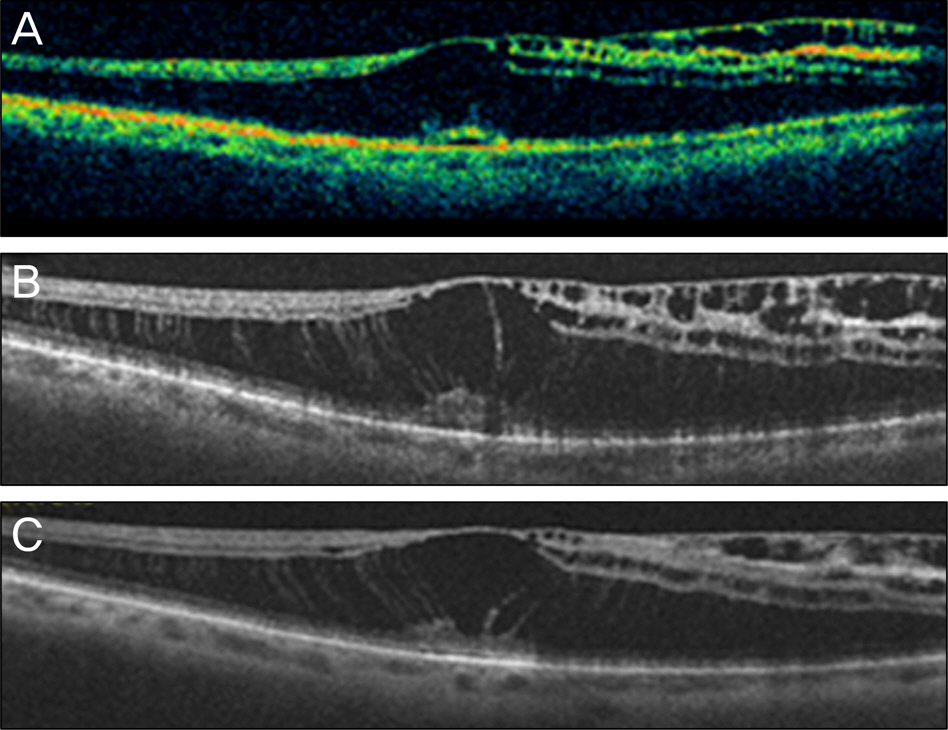
A Case of Serous Macular Detachment Preceding Macular Retinoschisis in an Optic Pit
- Affiliations
-
- 1Department of Ophthalmology, Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea. sungpyo@hanafos.com
- 2Department of Ophthalmology, Edward S. Harkness Eye Institute, Columbia University Medical Center, New York, USA.
Abstract
- PURPOSE
To report a case of serous macular detachment preceding macular retinoschisis in an optic pit patient successfully treated by vitrectomy with internal limiting membrane peeling.
CASE SUMMARY
A 76 year old female visited our clinic for visual disturbance in her right eye. Fundus photograph revealed optic pit and OCT showed macular retinoschisis in her right eye. She was followed up in our clinic. The patient revisited our clinic because of sudden decrease of visual acuity in her right eye 3 days before. At that time, the patient's best-corrected visual acuity was 0.05. Macular retinoschisis, subretinal fluid and serous retinal detachment were observed in her right eye on OCT. She was diagnosed with serous retinal detachment associated with optic pit and pars plana vitrectomy was performed. During vitrectomy, we found adhesion and defect of posterior hyaloid membrane which covered the optic pit. Therefore, subretinal fluid was drained via membrane defect and posterior vitreous detachment and fluid-gas exchange were induced. Sixteen days after surgery, we found a macular hole in her right eye on OCT. Pars plana vitrectomy was performed with internal limiting membrane peeling. One month after surgery, macular detachment was not observed. Six months after surgery, the patient's best corrected visual acuity was 0.63 and the macula was reattached completely.
CONCLUSIONS
Optic pit maculopathy can be progressed rapidly in aged patients and macular hole would be ocurred as a complication. Additional study will be needed to figure out the role of internal limiting membrane and tractional force of posterior vitreous in these patients.
MeSH Terms
Figure
Reference
-
References
1. Brown GC, Shields JA, Goldberg RE.Congenital pits of the optic nerve head. Ophthalmol. 1980; 87:51–65.
Article2. Brown GC, Shields JA, Patty BE, Goldberg RE.Congenital pits of the optic nerve head. I. Experimental studies in collie dogs. Arch Ophthalmol. 1979; 97:1341–4.3. Krivoy D, Gentile R, Liebmann JM. . Imaging congenital optic disc pits and associated maculopathy using optical coherence tomography. Arch Ophthalmol. 1996; 114:165–70.
Article4. Kuhn F, Kover F, Szabo I, Mester V.Intracranial migration of sili-cone oil from an eye with optic pit. Graefes Arch Clin Exp Ophthalmol. 2006; 244:1360–2.
Article5. Lincoff H, Lopez R, Kreissig I. . Retinoschisis associated with optic nerve pits. 1988; Retina. 2012; 32(Suppl 1):61–7.
Article6. Postel EA, Pulido JS, McNamara JA, Johnson MW.The etiology and treatment of macular detachment associated with optic nerve pits and related anomalies. Trans Am Ophthalmol Soc. 1998; 96:73–93.7. Akiba J, Kakehashi A, Hikichi T, Trempe CL.Vitreous findings in cases of optic nerve pits and serous macular detachment. Am J Ophthalmol. 1993; 116:38–41.
Article8. Christoforidis JB, Terrell W, Davidorf FH.Histopathology of optic nerve pit-associated maculopathy. Clin Ophthalmol. 2012; 6:1169–74.
Article9. Hirakata A, Okada AA, Hida T.Long-term results of vitrectomy without laser treatment for macular detachment associated with an optic disc pit. Ophthalmology. 2005; 112:1430–5.
Article10. Lincoff H, Yannuzzi L, Singerman L. . Improvement in visual function after displacement of the retinal elevations emanating from optic pits. Arch Ophthalmol. 1993; 111:1071–9.
Article11. Lincoff H, Kreissig I.Optical coherence tomography of pneumatic displacement of optic disc pit maculopathy. Br J Ophthalmol. 1998; 82:367–72.
Article12. Inoue M, Shinoda K, Ishida S.Vitrectomy combined with glial tis-sue removal at the optic pit in a patient with optic disc pit maculop-athy: a case report. J Med Case Rep. 2008; 2:103.
Article13. Hirakata A, Hida T, Ogasawara A, Iizuka N.Multilayered reti-noschisis associated with optic disc pit. Jpn J Ophthalmol. 2005; 49:414–6.
Article14. Gregory-Roberts EM, Mateo C, Corcóstegui B. . Optic disk pit morphology and retinal detachment: optical coherence tomog-raphy with intraoperative correlation. Retina. 2013; 33:363–70.15. Haruta M, Kamada R, Umeno Y, Yamakawa R.Vitrectomy for op-tic disc pit-associated maculopathy with or without preoperative posterior vitreous detachment. Clin Ophthalmol. 2012; 6:1361–4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Optic Disc Pit
- A Case of Vitrectomy without Laser for Serous Macular Detachment Associated with Optic Disc Pit
- A Case of Serous Macular Detachment Associated with Tractional Fibrous Tissue in an Optic Pit Patient
- A Case of Surgically Treated Serous Macular Detachment Associated With Optic Disc Pit
- Case of Macular Hole after Surgery in Macular Detachment with Optic Disc Pit in a Child