J Korean Ophthalmol Soc.
2013 Dec;54(12):1882-1887.
The Outcome of Graded Inferior Oblique Recession in the Congenital Unilateral Superior Oblique Palsy
- Affiliations
-
- 1Department of Ophthalmology, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea.
- 2Department of Ophthalmology, Yeungnam University College of Medicine, Daegu, Korea. mmk@med.yu.ac.kr
Abstract
- PURPOSE
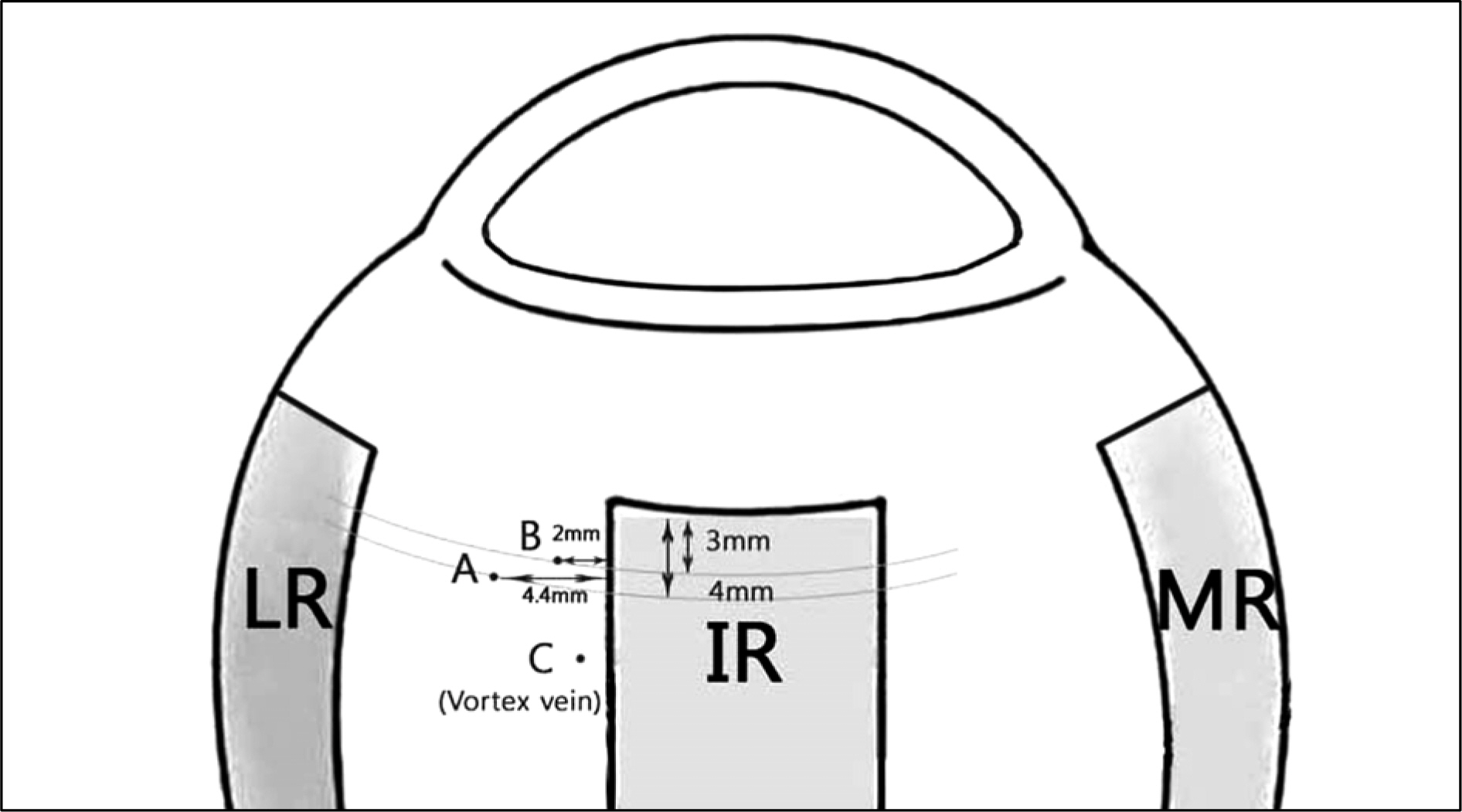
To examine changes in vertical deviation and improvement in head tilt after graded inferior oblique (IO) recession surgery in patients with congenital unilateral superior oblique palsy (SOP). Frequency of inferior oblique overaction (IOOA) or bilateral SOP in the contralateral eye after surgery was also investigated.
METHODS
We retrospectively reviewed medical records of 65 patients who had undergone graded IO recession surgery in unilateral congenital SOP with at least 1 year of postoperative follow-up. Postoperative vertical deviation was classified as excellent (under 3 prism diopters, PD), good (4-7 PD) or poor (over 8 PD). The occurrence of IOOA was considered if more than 2 IOOAs were observed in the contralateral eye after surgery.
RESULTS
Forty-five of the 65 patients (69%) obtained excellent results and 67.3% had improvement in head tilt after surgery. IOOA in the contralateral eye was not observed in any patients before surgery. Postoperative IOOA in the contralateral eye occurred in 9 patients (13.8%) and a diagnosis of masked bilateral SOP was made in 1 patient (1.5%).
CONCLUSIONS
The graded IO recession procedures are considered to be an effective surgical method for the treatment of unilateral congenital SOP. However, IOOA or masked bilateral SOP occurring in the contralateral eye was observed in 15.3% of the patients undergoing surgery.
Keyword
Figure
Reference
-
References
1. Von Noorden GK, Murray E, Wong SY. Superior oblique paralysis: a review of 270 cases. Arch Ophthalmol. 1986; 104:1771–6.2. Jin YH. Strabismology. Ulsan University Press;2001. p. 341–52.3. Flander M, Draper J. Superior oblique palsy: diagnosis and treatment. Can J Ophthalmol. 1990; 25:17–24.4. Rosenbaum AL, Santiago AP. Clinical strabismus management: principles and surgical techniques. Philadelphia: Saunders;1999. p. 226–7.5. Gonzalez C. Denervation of the inferior oblique: current status and long-term results. Trans Sect Ophthalmol Am Acad Ophthalmol Otolaryngol. 1976; 81:899–906.6. Helveston EM, Haldi BA. Surgical weakening of the inferior oblique. Int Ophthalmol Clin. 1976; 16:113–26.7. Raab EL, Costenbader FD. Unilateral surgery for inferior oblique overaction. Arch Ophthalmol. 1973; 90:180–2.8. Parks MM. The overacting inferior oblique muscle. Am J Ophthalmol. 1974; 77:787–97.9. Kraft SP, Scott WE. Masked bilateral superior oblique palsy: clin-ical features and diagnosis. J Pediatr Ophthalmol Strabismus. 1986; 23:264–72.10. Esmail F, Flanders M. Masked bilateral superior oblique palsy. Can J Ophthalmol. 2003; 38:476–81.11. Jin YH. Strabismology. Ulsan University Press;2001. p. 179.12. Rosenbaum AL, Santiago AP. Clinical strabismus management: principles and surgical techniques. Philadelphia: Saunders;1999. p. 17.13. Parks MM. Atlas of Strabismus Surgery. Philadelpia: Harper and Row Publishers;1983. p. 167–87.14. Simons BD, Saunders TG, Siatkowski RM. . Outcome of sur-gical management of superior oblique palsy: a study of 123 cases. Binocul Vis Strabismus Q. 1998; 13:273–82.15. Shin KS, Yoo JM. The effect of modified anterior transposition of the inferior oblique muscle for hypertropia in superior oblique muscle palsy with inferior oblique muscle overaction. J Korean Ophthalmol Soc. 2003; 44:384–9.16. Duane A. Tenotomy of inferior oblique and consideration of the conditions that may call for the operation. Br Med J. 1906; 2:1867–70.17. White JW. Surgery of the inferior oblique at or near the insertion. Trans Am Ophthalmol Soc. 1942; 40:118–26.18. Wright KW. Pediatric ophthalmology and Strabismus. St. Louse: CV Mosby;1995. p. 287–91.19. Burke JP, Scott WE, Kutshke PJ. Anterior transposition of the in-ferior oblique muscle for dissociated vertical deviation. Ophthalmology. 1993; 100:245–50.20. Kim SJ, Moon SH, Ahn JW. The effect of modified anterior trans-position of the inferior oblique muscle. J Korean Ophthalmol Soc. 1997; 38:479–84.21. Parks MM. Inferior oblique weakening procedures. Int Ophthalmol Clin. 1985; 25:107–17.22. Parks MM. A study of weakening surgical procedures for eliminating overaction of the inferior oblique. Trans Am Ophthalmol Soc. 1971; 69:163–87.23. Parks MM. The weakening surgical procedures for eliminating overaction of the inferior oblique muscle. Am J Ophthalmol. 1972; 73:107–22.24. Fink WH. Oblique muscle surgery from the anatomic viewpoint. Am J Ophthalmol. 1951; 34:261–81.25. Apt L, Call NB. Inferior oblique muscle recession. Am J Ophthalmol. 1978; 85:95–100.26. Hong JS, Kim MM. Long-term outcome of graded inferior oblique recession. J Korean Ophthalmol Soc. 2006; 47:127–32.27. Lee KH, Kyung SE, Chang MH. The effect of minimal amount in-ferior oblique recession in superior oblique palsy. J Korean Ophthalmol Soc. 2009; 50:253–9.28. Kim JW, Kim MM. The effect of inferior oblique weakening proce-dures in the congenital superior oblique palsies. J Korean Ophthalmol Soc. 2004; 45:1893–8.29. Wright KW. Color atlas of strabismus surgery: cranial nerve palsy. 3th ed.Los Angeles: Springer;2007. p. 76–87.30. Von Noorden GK, Campos EC. Binocular vision and ocular motility: theory and management of strabismus. 6th ed.St. Louis: Mo Mosby;2002. p. 377–95.31. Saunders RA, Kruger SJ, Lall-Trail JK, Rust PF. A 10-year overview of double elevator muscle weakening procedures. Arch Ophthalmol. 2007; 125:634–8.32. Meyer DR, Simon JW, Kansora M. Primary infratarsal lower eye-lid retractor lysis to prevent eyelid retraction after inferior rectus muscle recession. Am J Ophthalmol. 1996; 122:331–9.33. Cho YA. The evaluation and treatment of superior oblique muscle palsy. J Korean Ophthalmol Soc. 1988; 29:363–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Graded Recession and Anteriorization on Unilateral Superior Oblique Palsy
- Comparison of Inferior Oblique Myectomy, Recession, and Anterior Transposition in Unilateral Congenital Superior Oblique Palsy
- Long-term Outcome of Graded Inferior Oblique Recession
- The Effect of Minimal Amount Inferior Oblique Recession in Superior Oblique Palsy
- Superior Oblique Palsy