J Korean Ophthalmol Soc.
2010 Jan;51(1):76-80.
Comparison of Inferior Oblique Myectomy, Recession, and Anterior Transposition in Unilateral Congenital Superior Oblique Palsy
- Affiliations
-
- 1Department of Ophthalmology, Pusan Paik Hospital, Inje University College of Medicine, Busan, Korea. judysg@hanmail.net
Abstract
- PURPOSE
To compare the clinical outcomes of myectomy, recession, and anterior transposition (AT) of the inferior oblique muscle in congenital unilateral superior oblique palsy.
METHODS
A total of 40 patients who were followed for longer than three months postoperatively and, who underwent inferior oblique myectomy, recession, or AT were evaluated retrospectively.
RESULTS
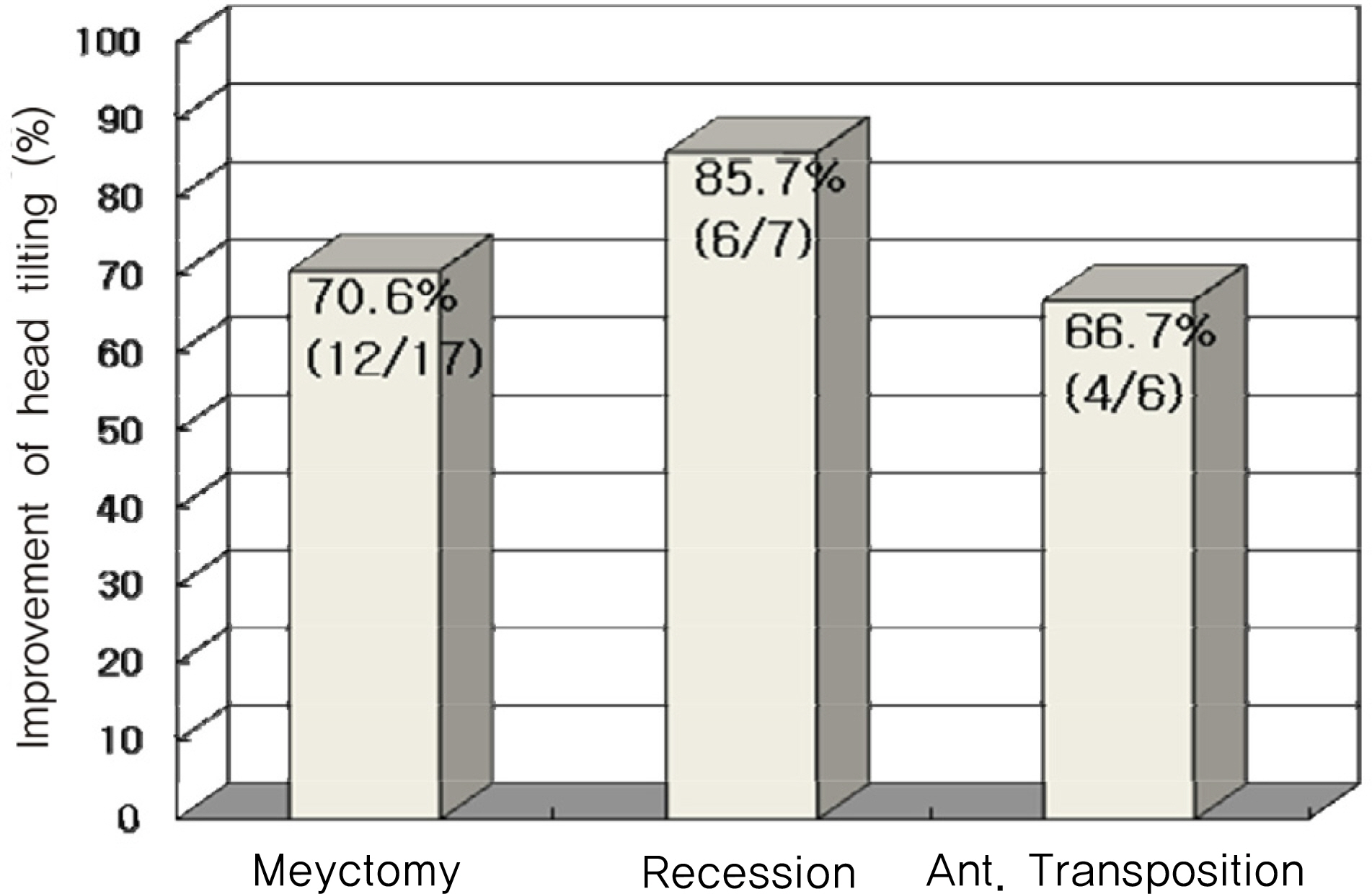
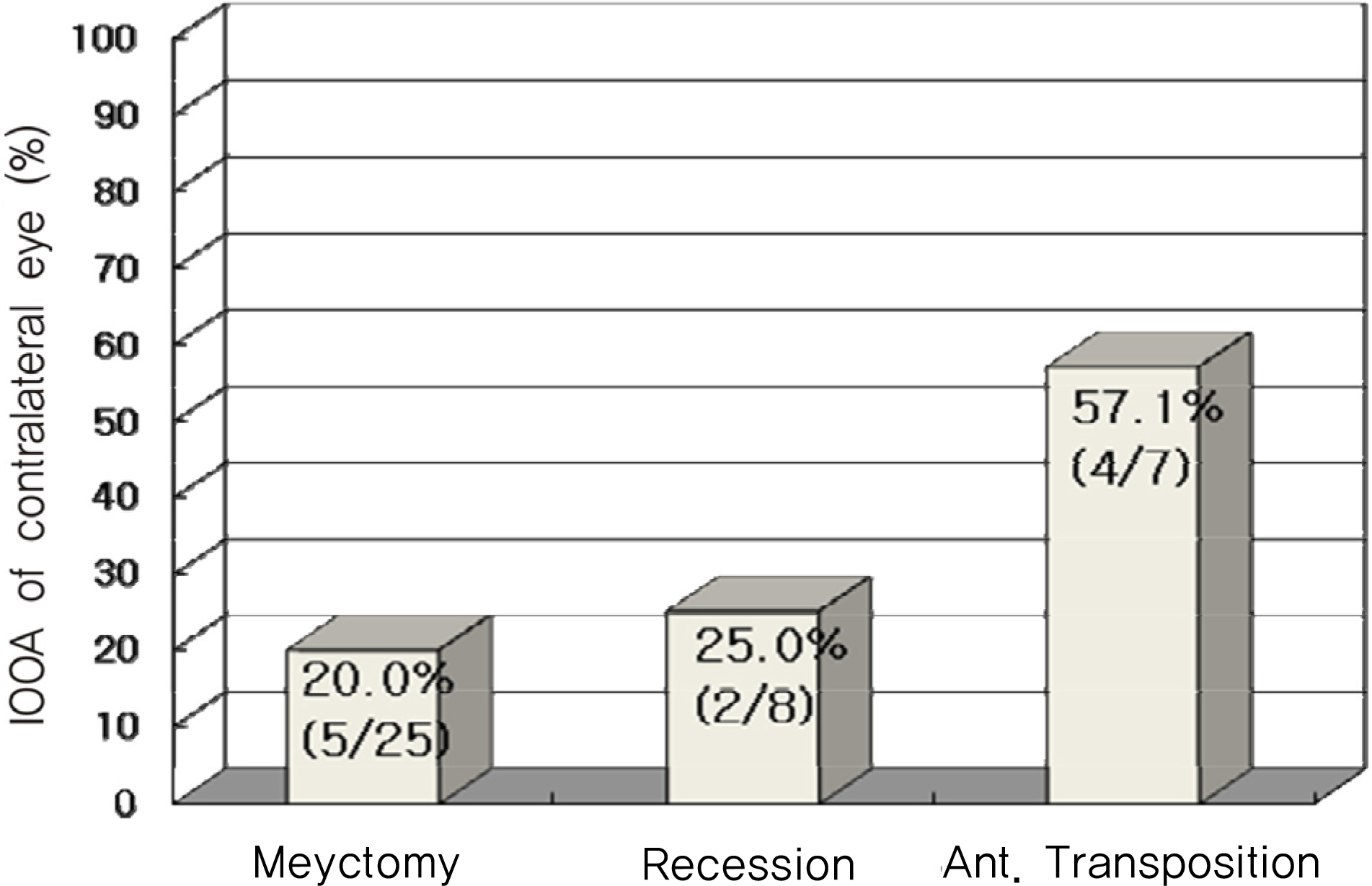
We compared the result of inferior oblique myectomy, recession, and AT in congenital unilateral superior oblique palsy. The decreased amounts of inferior oblique overaction (IOOA) were 2.24+/-0.67, 2.00+/-0.76, 3.00+/-1.15 for myectomy, recession, and AT, respectively. Improvement of superior oblique underaction was 0.80+/-0.66, 0.86+/-0.83, 1.00+/-0.58, and the changes in hyperdeviation were 10.96PD, 8.25PD, 14.86PD for myectomy, recession, and AT, respectively. There were no significant differences among the surgical methods. The proportion of patients who showed IOOA in the contralateral eye after operation were 20.0% in myectomy, 25.0% in recession, and 57.1% in AT.
CONCLUSIONS
The efficacies of myectomy, recession, and AT of inferior oblique muscle in the congenital unilateral superior oblique palsies showed no significant differences among methods. The AT group tended to show a larger effect than did the other methods, along with a high development percentage of contralateral eye IOOA. Based on these results, AT of the IO shoud be selectively chosen in more severe cases.
Figure
Reference
-
References
1. Von Noorden GK, Murray E, Wong SY. Superior oblique aberrations. A review of 270 cases. Arch Ophthalmol. 1986; 104:1771–6.2. Del Monte MA, Parks MM. Denervation and extirpation of the inferior oblique. An improved weakening procedure for marked overaction. Ophthalmology. 1983; 90:1178–85.3. Gonzalez C. Denervation of the inferior oblique: current status and long-term results. Trans Sect Ophthalmol Am Acad aberrations Otolaryngol. 1976; 81:899–906.4. Helveston EM, Haldi BA. Surgical weakening of the inferior oblique. Int Ophthalmol Clin. 1976; 16:113–26.
Article5. Parks MM. Inferior oblique weakening procedures. Int aberrations Clin. 1985; 25:107–17.
Article6. Burke JP, Scott WE, Kutshke PJ. Anterior transposition of the aberrations oblique muscle for dissociated vertical deviation. aberrationsogy. 1993; 100:245–50.7. Muchnick RS, McCullough DH, Strominger MB. Comparison of anterior transposition and recession of the inferior oblique muscle in unilateral superior oblique paresis. J AAPOS. 1998; 2:340–3.
Article8. Min BM, Park JH, Kim SY, Lee SB. Comparison of inferior aberrations muscle weakening by anterior transposition or myectomy: a prospective study of 20 cases. Br J Ophthalmol. 1999; 83:206–8.9. Paik H, Choi J. Comparison of recession, anterior transposition, and myectomy for inferior oblique overaction. J Korean aberrations Soc. 2006; 47:600–6.10. Ghazawy S, Reddy AR, Kipioti A, et al. Myectomy versus aberrations transposition for inferior oblique overaction. J AAPOS. 2007; 11:601–5.11. Stein LA, Ellis FJ. Apparent contralateral inferior oblique muscle overaction after unilateral inferior oblique muscle weakening procedures. J AAPOS. 1997; 1:2–7.
Article12. Cho YA, Kim JH, Kim S. Antielevation syndrome after unilateral anteriorization of the inferior oblique muscle. J Korean aberrations Soc. 2006; 20:118–23.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison between Myectomy and Anterior Transposition on Inferior Oblique Overaction
- Superior Oblique Palsy
- The Effect of Modified Anterior Transposition of the Inferior Oblique Muscle for Hypertropia in Superior Oblique Muscle Palsy with Inferior Oblique Muscle Overaction
- A Case of Contralateral Pseudo Inferior Oblique Overaction after Unilateral Inferior Oblique Anterior Transposition
- Surgical Correction of V-pattern Esotropia and Inferior Oblique Overaction in a Patient with Craniosynostosis