J Korean Ophthalmol Soc.
2013 Oct;54(10):1561-1566.
Analysis of Eye Drops Applying Behavior in Glaucoma Patients
- Affiliations
-
- 1Department of Ophthalmology and Visual Science, Yeouido St. Mary's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea. marypark@catholic.ac.kr
Abstract
- PURPOSE
This study was conducted to understand the eye drop application method in patients with glaucoma.
METHODS
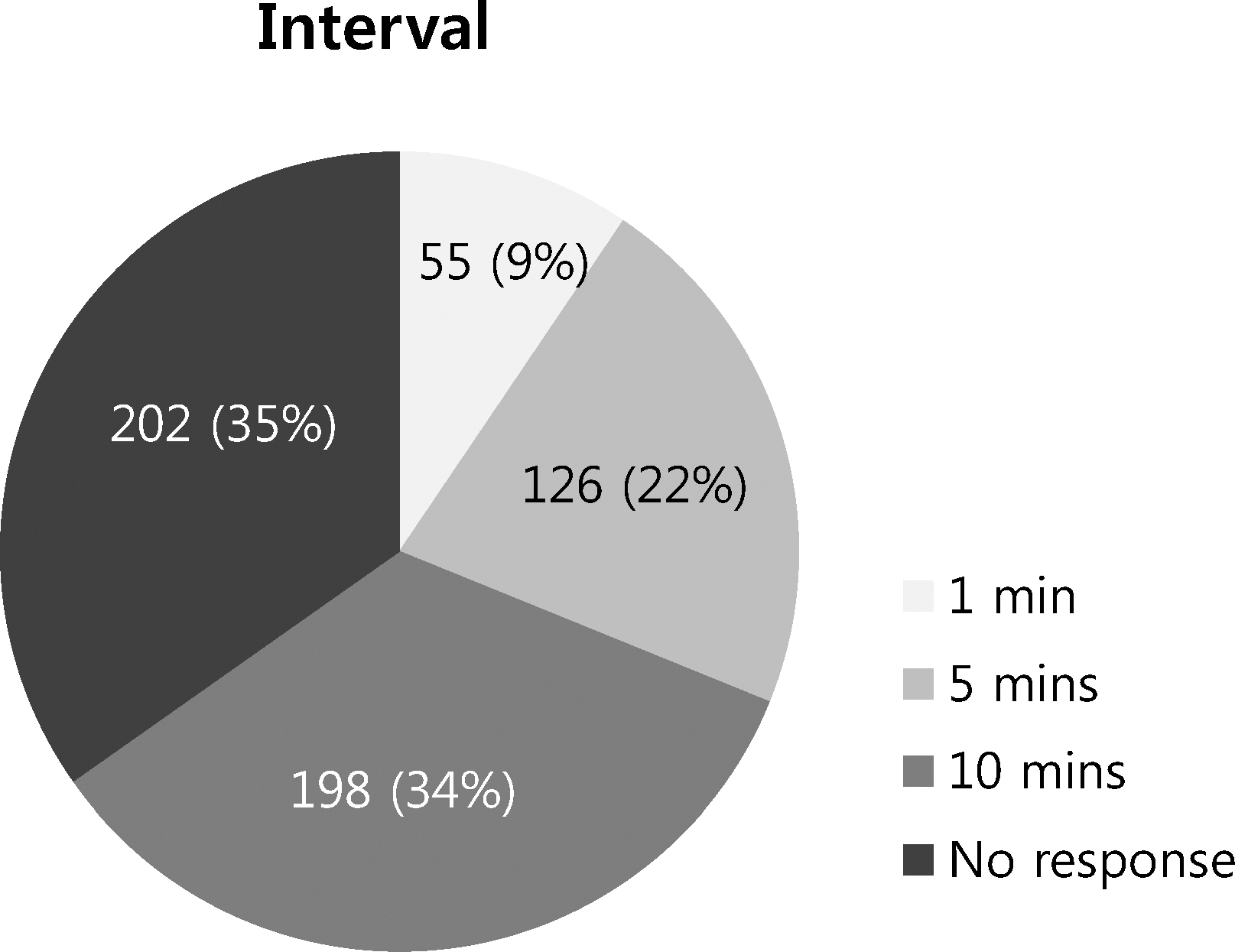
A survey was performed in 5 hospitals on patients diagnosed with glaucoma using eye drops for more than 1 month. Variables associated with eye drop application such as pressing on a dacryocyst after application, time interval between multiple eye drop medications, hygienic management of an eye dropper and shaking a bottle of eye drops before use were evaluated.
RESULTS
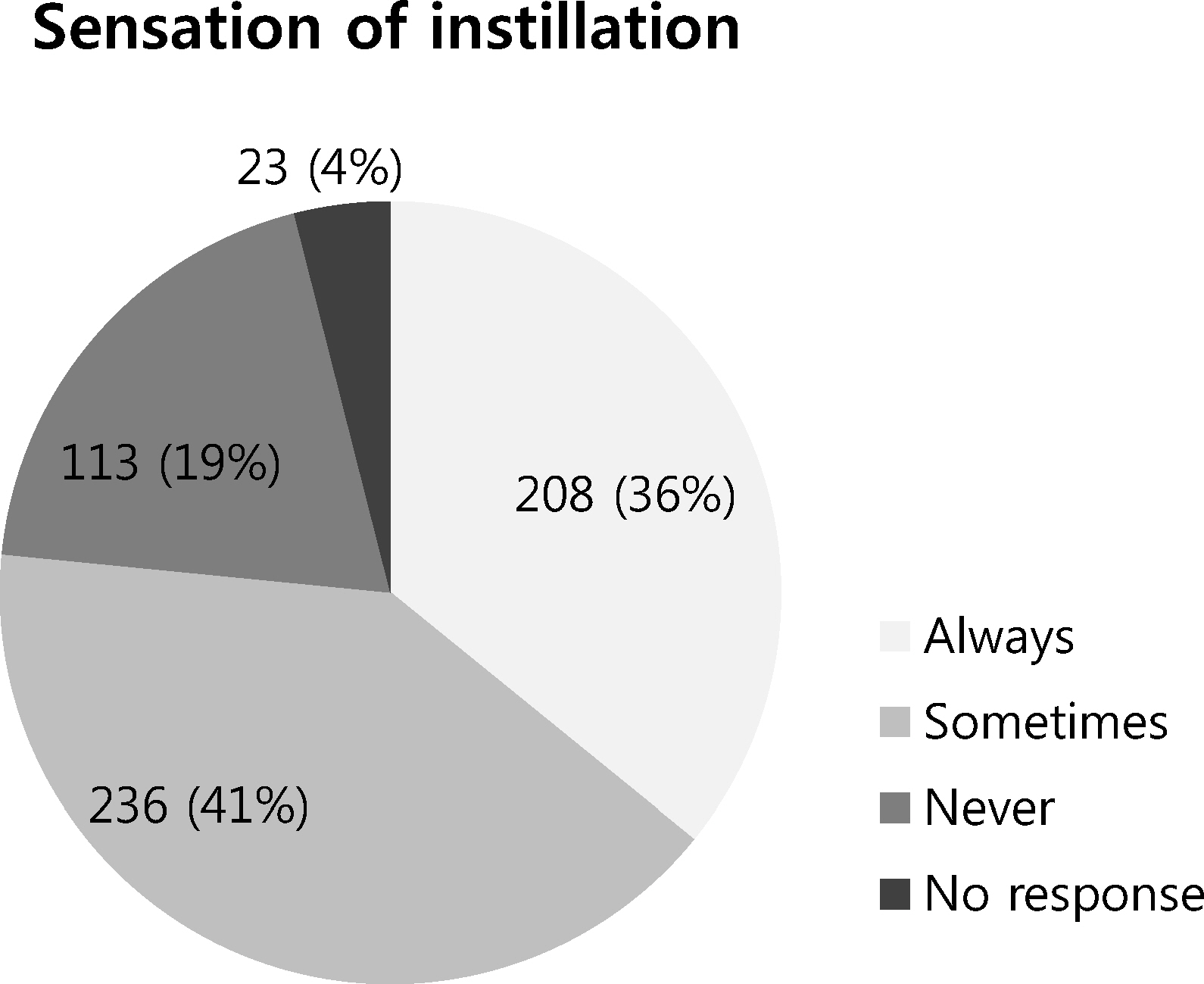
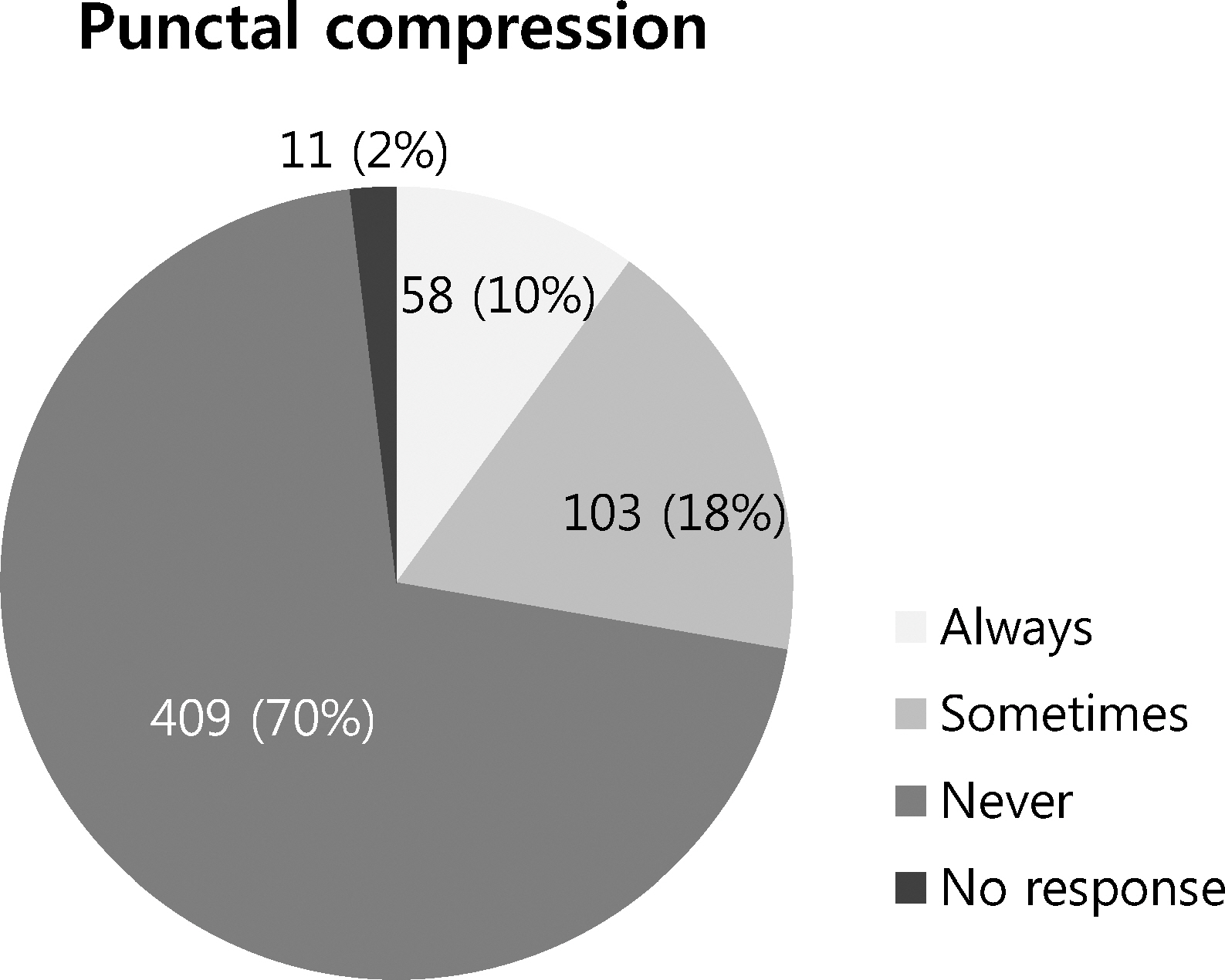
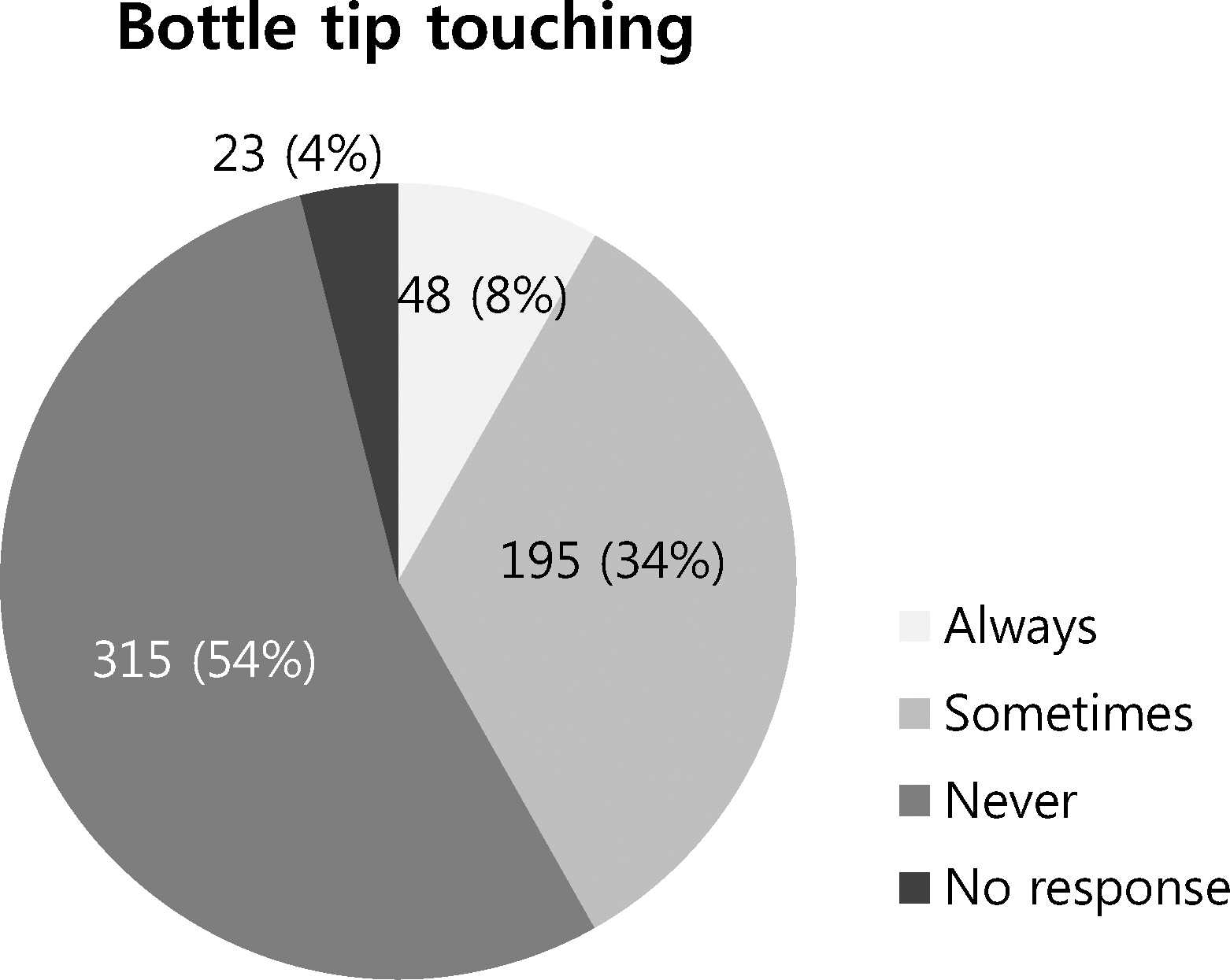
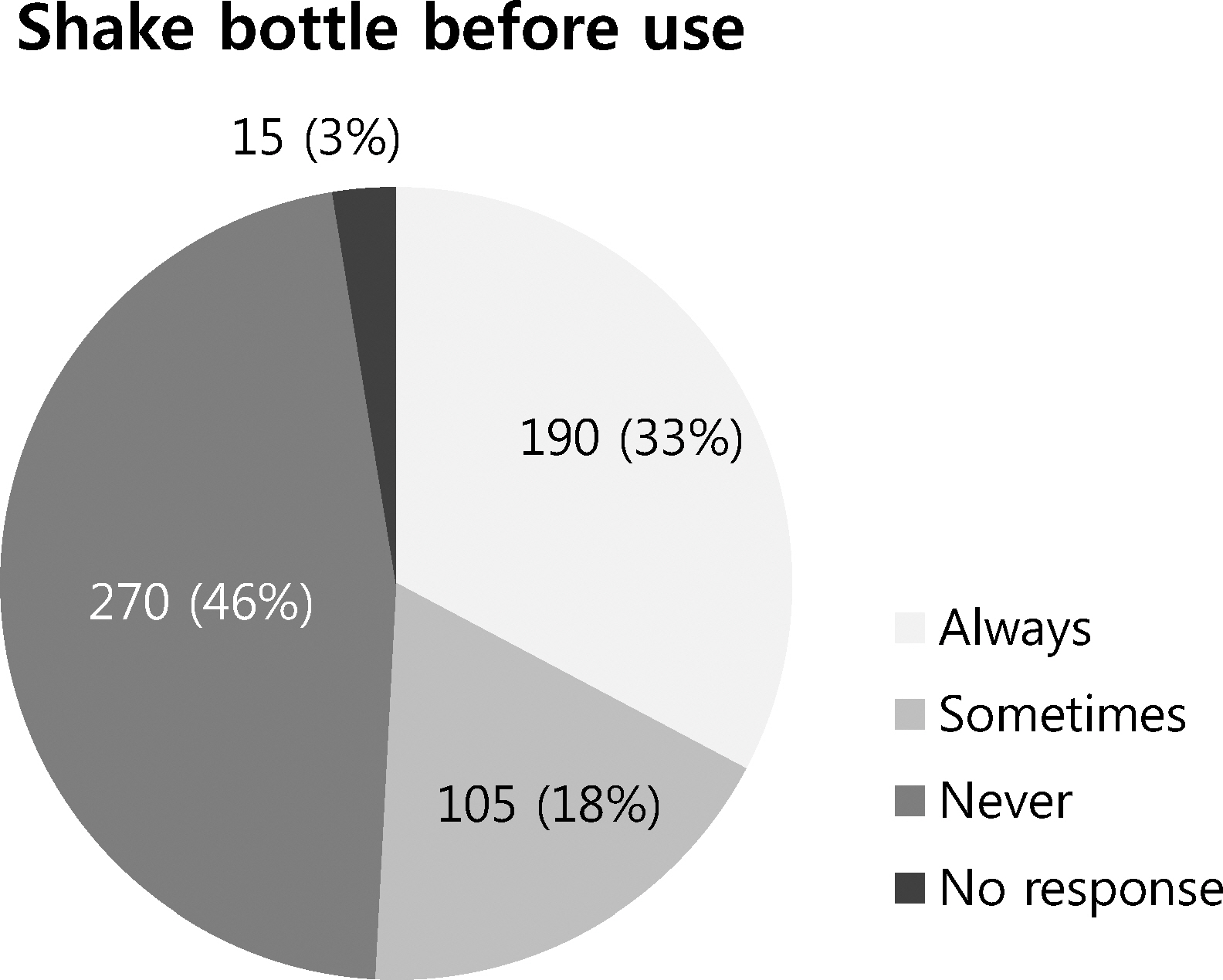
A total of 581 patients were surveyed in the present study. Regarding pressing on a dacryocyst after applying eye drops, 58 (10%) patients responded always, 103 patients (18%) sometimes, and 409 patients (70%) never. Three hundred fifteen patients (54%) did not touch the eye dropper to their eyes, 190 patients (33%) always shook the eye drop bottle before use and 106 patients (18%) shook the bottle sometimes.
CONCLUSIONS
When using eye drops for glaucoma to reduce the intraocular pressure, most patients are committing errors, reducing the effect of treatment and likely causing side effects. When prescribing eye drops to glaucoma patients, the physician should educate patients on the proper method of application.
Figure
Reference
-
References
1. Kass MA, Heuer DK, Higginbotham EJ. . The ocular hypertension treatment study: A randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002; 120:701–13. discussion 829-30.2. The effectiveness of intraocular pressure reduction in the treatment of normal-tension glaucoma. collaborative normal-tension glaucoma study group. Am J Ophthalmol. 1998; 126:498–505.3. Patel SC, Spaeth GL. Compliance in patients prescribed eyedrops for glaucoma. Ophthalmic Surg. 1995; 26:233–6.
Article4. Chang JS Jr, Lee DA, Petursson G. . The effect of a glaucoma medication reminder cap on patient compliance and intraocular pressure. J Ocul Pharmacol. 1991; 7:117–24.
Article5. Ashburn FS Jr, Goldberg I, Kass MA. Compliance with ocular therapy. Surv Ophthalmol. 1980; 24:237–48.
Article6. Ritun R, Shield M, Krupin T. The glaucomas. 1996.7. Simel DL, Simel PJ. Does lacrimal duct occlusion decrease intraocular pressure in patients refractory to medical treatment for glaucoma? A randomized, sham-controlled, crossover trial. J Clin Epidemiol. 1988; 41:859–65.
Article8. Fraunfelder FT. Extraocular fluid dynamics: How best to apply topical ocular medication. Trans Am Ophthalmol Soc. 1976; 74:457–87.9. Ellis PP, Wu PY, Pfoff DS. . Effect of nasolacrimal occlusion on timolol concentrations in the aqueous humor of the human eye. J Pharm Sci. 1992; 81:219–20.
Article10. Zimmerman TJ, Kooner KS, Kandarakis AS, Ziegler LP. Improving the therapeutic index of topically applied ocular drugs. Arch Ophthalmol. 1984; 102:551–3.
Article11. Foster PJ, Buhrmann R, Quigley HA, Johnson GJ. The definition and classification of glaucoma in prevalence surveys. Br J Ophthalmol. 2002; 86:238–42.
Article12. Ahn DH, Lee YG, Hong YJ. Factors affecting compliance with prescribed eyedrops for glaucoma. J Korean Ophthalmol Soc. 1998; 39:2145–51.13. Chung PH, Chin TF, Lach JL. Kinetics of the hydrolysis of pilocarpine in aqueous solution. J Pharm Sci. 1970; 59:1300–6.
Article14. Kass MA, Hodapp E, Gordon M. . Patient administration of eyedrops: Observation. part II. Ann Ophthalmol. 1982; 14:889–93.15. Kholdebarin R, Campbell RJ, Jin YP, Buys YM. Multicenter study of compliance and drop administration in glaucoma. Can J Ophthalmol. 2008; 43:454–61.
Article16. Zimmerman TJ, Diestelhorst M, Suverkrup R. Practical aspects of controlling glaucoma medically or how to make your glaucoma medicines work for you. glaucoma editorial. Klin Monbl Augenheilkd. 1980; 209:717–28.17. Mishima S, Gasset A, Klyce SD Jr, Baum JL. Determination of tear volume and tear flow. Invest Ophthalmol. 1966; 5:264–76.18. R RA.Shields textbook of glaucoma. 2011.19. Nourry H, Viard C, Cambourieu C, Warnet JM. A relevant choice for corticoid eye drops: Solution or suspension? J Fr Ophtalmol. 2011; 34:691–6.20. Kwon KA, Diestelhorst M. Süverkrüp R. Dosage problems in suspension eyedrops. Klin Monbl Augenheilkd. 1996; 209(2-3):144–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Study of Ocular Side Effects after the Use of Anti-Glaucoma Topical Medication
- Video-recording the Eyedrop Instillation Techniques of Glaucoma Patients
- Assessment of Glaucoma Medication Compliance
- Ocular Hypotensive Effects of beta-Adrenergic Blocking Agent: Timolol maleate
- Eye Drop Chart for Improvement of Topical Eye Drops Administration and Adherence