J Korean Ophthalmol Soc.
2013 Sep;54(9):1321-1326.
Clinical Usefulness of a Thermal-Massaging System for Treatment of Dry Eye with Meibomian Gland Dysfunction
- Affiliations
-
- 1Department of Ophthalmology, Kim's Eye Hospital, Konyang University College of Medicine, Myung-Gok Eye Research Institute, Seoul, Korea. jlchung@kimeye.com
Abstract
- PURPOSE
To evaluate the clinical usefulness of KCL 990(R) for the treatment of dry eye with meibomian gland dysfunction (MGD).
METHODS
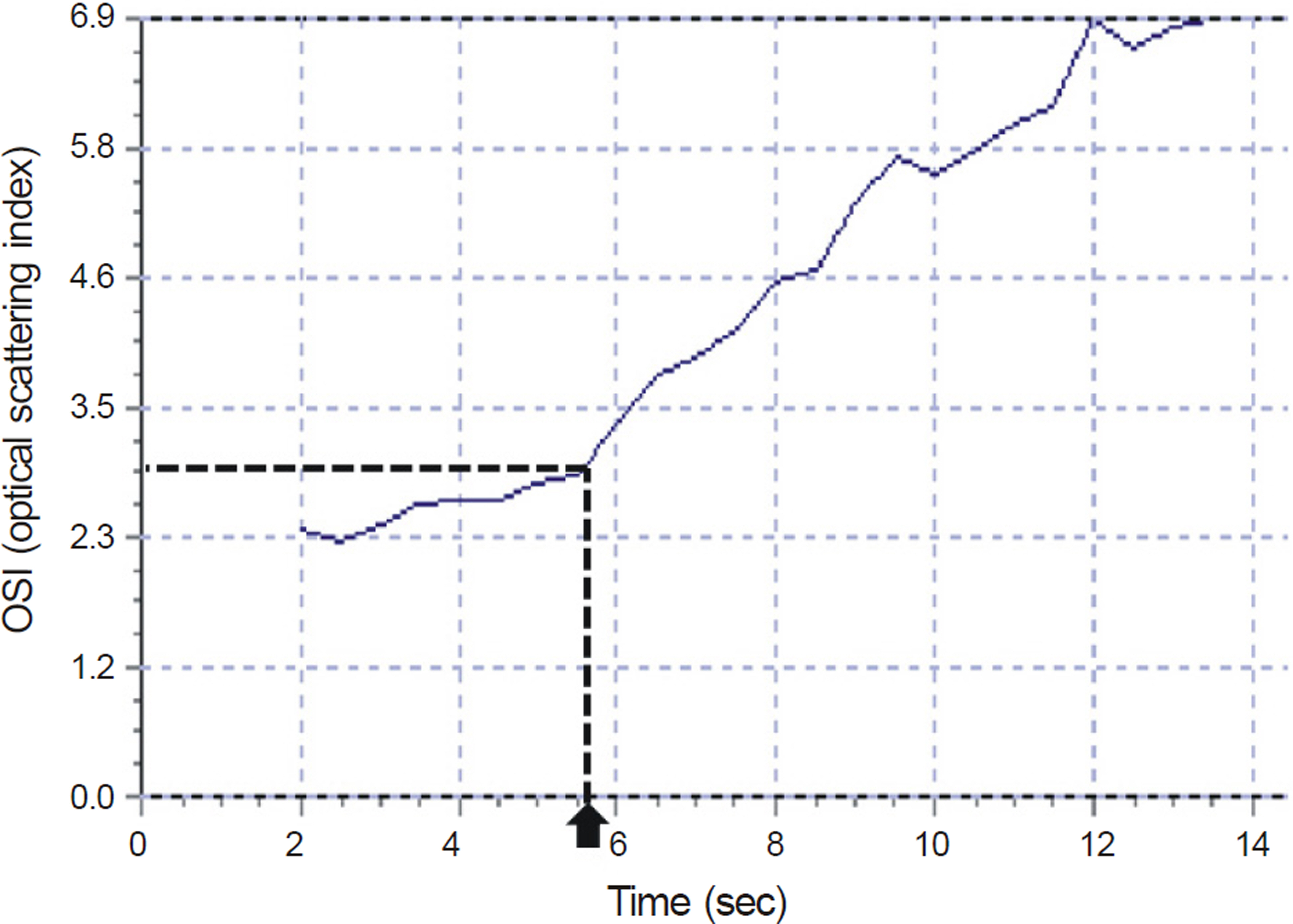
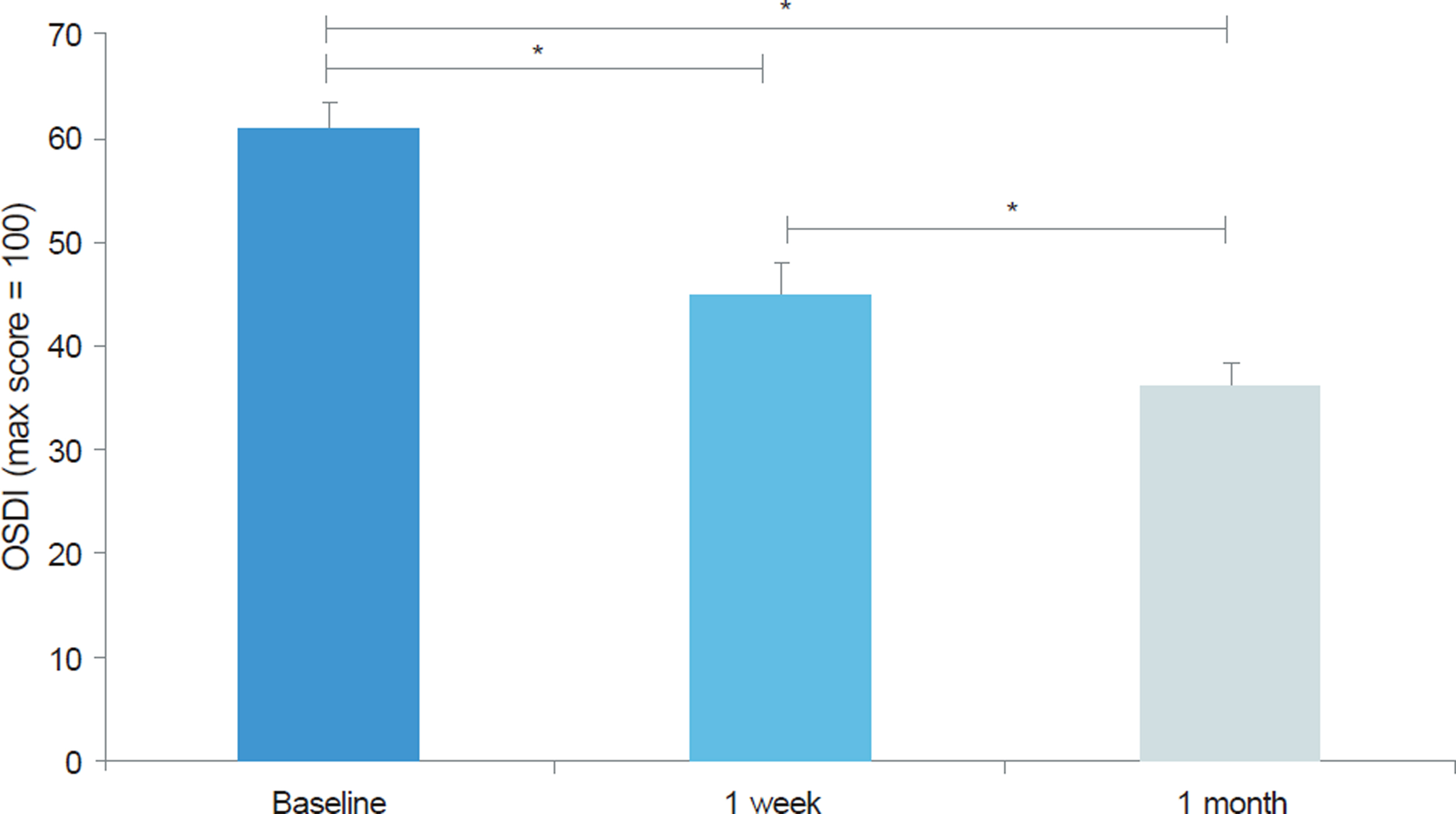
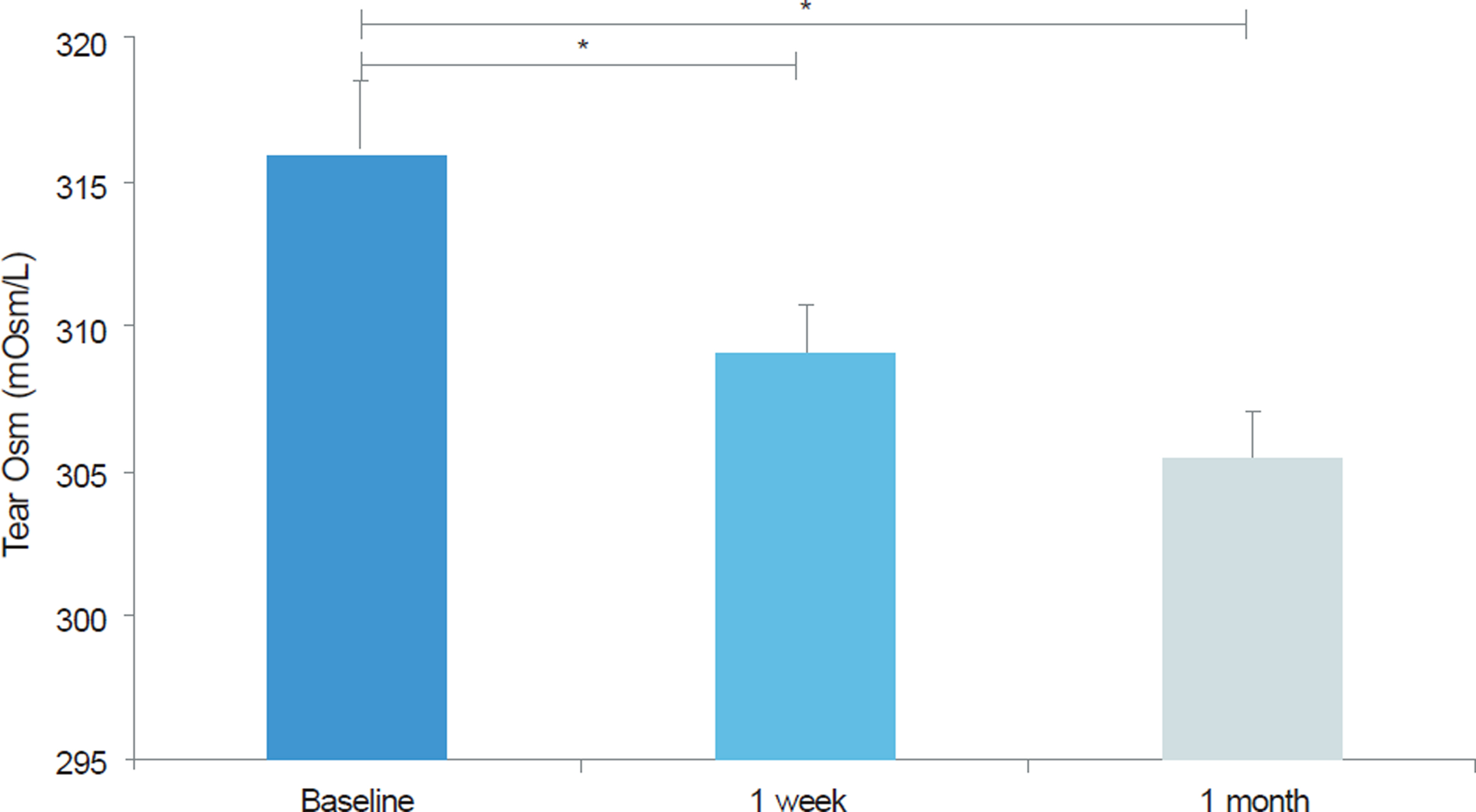
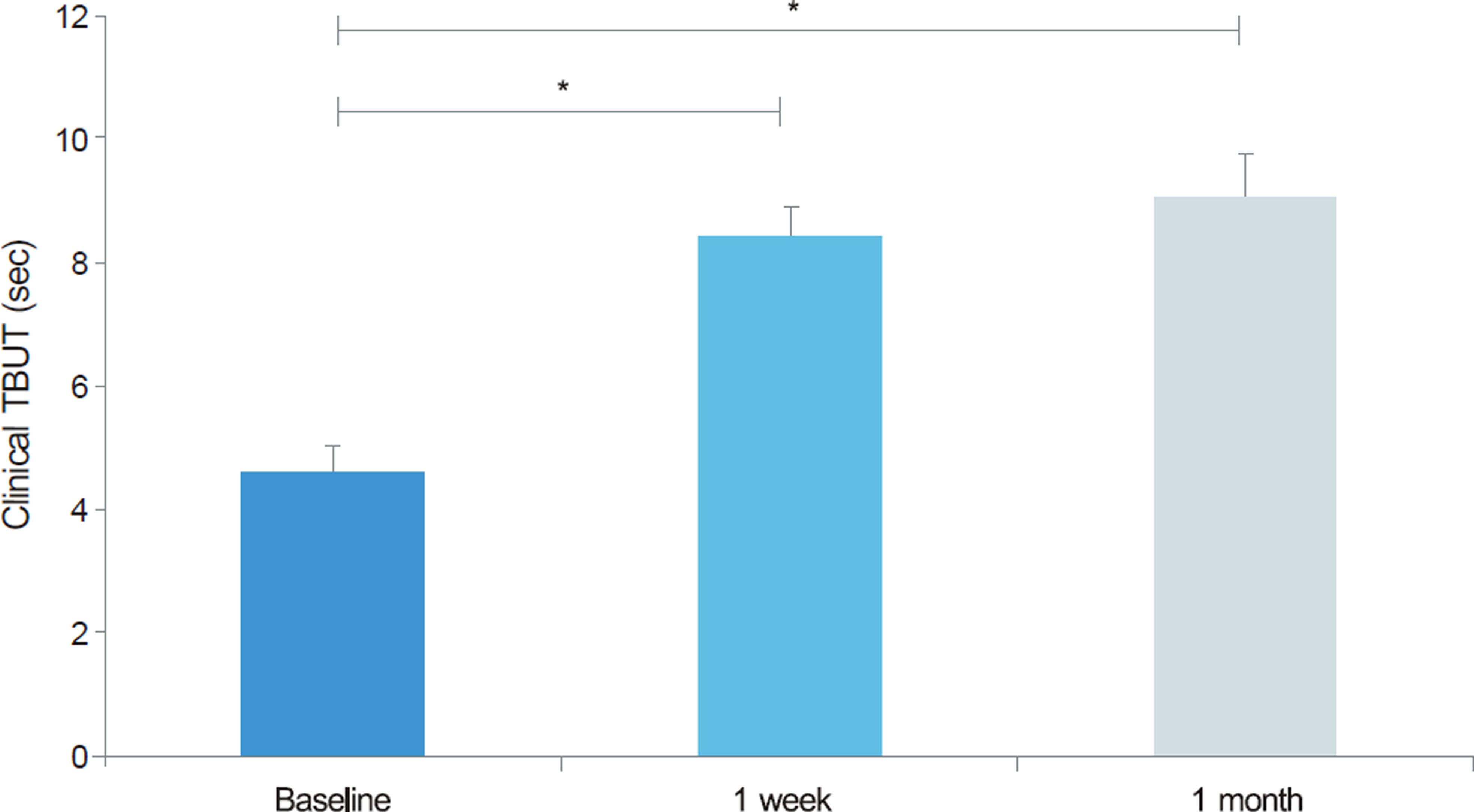
Patients (n = 54 eyes, 27 subjects) diagnosed with dry eye with MGD were recruited for a prospective, one-month clinical trial. Patients received a twice-a-day 15-minute treatment using the KCL 990(R). Effectiveness parameters included patient symptom scores using the Ocular Surface Disease Index (OSDI) questionnaires, tear osmolarity measured with TearLab(R) (TearLab Corporation, San Diego, CA, USA), classical tear break-up time (TBUT), and objective TBUT value using an Optical Quality Analysis System (OQAS(R), Visiometrics, Castelldefels, Spain). Data are presented for pre-treatment (baseline) and at 1 week and 1 month post-treatment. An objective TBUT value was estimated in each eye when the optical scattering index (OSI) started to increase consistently, and data were obtained at pretreatment (baseline) and at 1 month post-treatment.
RESULTS
The symptom scores on OSDI questionnaires, tear osmolarity, and tear break-up time improved significantly from baseline to one week (p < 0.05). This improvement was maintained with no significant regression at 1 month (p < 0.05). The objective TBUT value decreased significantly at 1 month (p < 0.05).
CONCLUSIONS
KCL 990(R) contributed to improve not only signs and symptoms of dry eye with MGD, but also the function of the tear film and ocular surface.
MeSH Terms
Figure
Reference
-
References
1. Tiffany JM. The lipid secretion of the meibomian glands. Adv Lipid Res. 1987; 22:1–62.
Article2. Lemp MA. Report of the National Eye Institute/Industry workshop on clinical trials in dry eyes. CLAO J. 1995; 21:221–32.3. Lee SH, Tseng SC. Rose bengal staining and cytologic character-istics associated with lipid tear deficiency. Am J Ophthalmol. 1997; 124:736–50.
Article4. Korb DR, Greiner JV. Increase in tear film lipid layer thickness fol-lowing treatment of meibomian gland dysfunction. Adv Exp Med Biol. 1994; 350:293–8.
Article5. Key JE. A comparative study of eyelid cleaning regimens in chron-ic blepharitis. CLAO J. 1996; 22:209–12.6. Smith RE, Flowers CW Jr. Chronic blepharitis: a review. CLAO J. 1995; 21:200–7.7. Driver PJ, Lemp MA. Meibomian gland dysfunction. Surv Ophthalmol. 1996; 40:343–67.
Article8. Shine WE, McCulley JP. Meibomianitis: polar lipid abnormalities. Cornea. 2004; 23:781–3.9. Goto E, Monden Y, Takano Y. . Treatment of noninflamed ob-structive meibomian gland dysfunction by an infrared warm com-pression device. Br J Ophthalmol. 2002; 86:1403–7.
Article10. Freedman HL, Preston KL. Heat retention in varieties of warm compresses: A comparison between warm soaks, hard-boiled eggs and the re-heater. Ophthalmic Surg. 1989; 20:846–8.
Article11. Blackie CA, Solomon JD, Greiner JV. . Inner eyelid surface temperature as a function of warm compress methodology. Optom Vis Sci. 2008; 85:675–83.
Article12. Nelson JD, Shimazaki J, Benitez-del-Castillo JM. . The inter-national workshop on meibomian gland dysfunction: report of the definition and classification subcommittee. Invest Ophthalmol Vis Sci. 2011; 52:1930–7.
Article13. Schiffman RM, Christianson MD, Jacobsen G. . Reliability and validity of the Ocular Surface Disease Index. Arch Ophthalmol. 2000; 118:615–21.
Article14. Szalai E, Berta A, Szekanecz Z. . Evaluation of tear osmolarity in non-Sjögren and Sjögren syndrome dry eye patients with the TearLab system. Cornea. 2012; 31:867–71.
Article15. Benito A, Pérez GM, Mirabet S. . Objective optical assessment of tear-film quality dynamics in normal and mildly symptomatic dry eyes. J Cataract Refract Surg. 2011; 37:1481–7.
Article16. Mori A, Shimazaki J, Shimmura S. . Disposable eyelid-warming device for the treatment of meibomian gland dysfunction. Jpn J Ophthalmol. 2003; 47:578–86.
Article17. Matsumoto Y, Dogru M, Goto E. . Efficacy of a new warm moist air device on tear functions of patients with simple meibo-mian gland dysfunction. Cornea. 2006; 25:644–50.
Article18. Driver PJ, Lemp MA. Meibomian gland dysfunction. Surv Ophthalmol. 1996; 40:343–67.
Article19. Paranjpe DR, Foulks GN. Therapy for meibomian gland disease. Ophthalmol Clin North Am. 2003; 16:37–42.
Article20. Shine WE, McCulley JP, Pandya AG. Minocycline effect on mei-bomian gland lipids in meibomianitis patients. Exp Eye Res. 2003; 76:417–20.
Article21. Olson MC, Korb DR, Greiner JV. Increase in tear film lipid layer thickness following treatment with warm compresses in patients with meibomian gland dysfunction. Eye Contact Lens. 2003; 29:96–9.
Article22. Goto E, Monden Y, Takano Y. . Treatment of non-inflamed ob-structive meibomian gland dysfunction by an infrared warm com-pression device. Br J Ophthalmol. 2002; 86:1403–7.
Article23. Methodologies to diagnose and monitor dry eye disease: report of the Diagnostic Methodology Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007; 5:108–52.24. Behrens A, Doyle JJ, Stern L. . Dysfunctional tear syndrome. a Delphi approach to treatment recommendations. Cornea. 2006; 25:900–7.
Article25. Lane SS, DuBiner HB, Epstein RJ. . A new system, the LipiFlow, for the treatment of meibomian gland dysfunction. Cornea. 2012; 31:396–404.
Article26. Benelli U, Nardi M, Posarelli C, Albert TG. Tear osmolarity meas-urement using the TearLab Osmolarity System in the assessment of dry eye treatment effectiveness. Cont Lens Anterior Eye. 2010; 33:61–7.
Article27. Utine CA, Bıçakçı gil M, Yavuz S, Çiftçi F. Tear osmolarity meas-urements in dry eye related to primary Sjögren’s syndrome. Curr Eye Res. 2011; 36:683–90.
Article28. Jacobi C, Jacobi A, Kruse FE, Cursiefen C. Tear film osmolarity measurements in dry eye disease using electrical impedance technology. Cornea. 2011; 30:1289–92.
Article29. Benito A, Pérez GM. . Objective optical assessment of tear-film quality dynamics in normal and mildly symptomatic dry eyes. J Cataract Refract Surg. 2011; 37:1481–7.
Article30. Pult H, Riede-Pult BH. Non-contact meibography in diagnosis and treatment of non-obvious meibomian gland dysfunction. J Optom. 2012; 5:2–5.
Article31. Geerling G, Tauber J, Baudouin C. . The international work-shop on meibomian gland dysfunction: Report of the sub-committee on management and treatment of meibomian gland dysfunction. Invest Ophthalmol Vis Sci. 2011; 52:2050–64.
Article32. Dogru M, Tsubota K. Pharmacotherapy of dry eye. Expert Opin Pharmacother. 2011; 12:325–34.
Article33. Greiner JV. A single LipiFlow® Thermal Pulsation System treat-ment improves meibomian gland function and reduces dry eye symptoms for 9 months. Curr Eye Res. 2012; 37:272–8.34. McMonnies CW, Korb DR, Blackie CA. The role of heat in rub-bing and massage-related corneal deformation. Cont Lens Anterior Eye. 2012; 35:148–54.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Therapeutic Effect of Intense Pulsed Light of Dry Eye with Meibomian Gland Dysfunction
- Assessment of Meibomian Gland Dysfunction and Comparison of The Results of BUT and Schirmer Test According to Meibomian Gland State
- Effects and Prognostic Factors of Automated Thermodynamic System Treatment for Meibomian Gland Dysfunction
- Risk Factors of Meibomian Gland Loss in Dry Eye Disease
- CCL4 Concentration in Tears of Dry Eye Patients and Its Correlation With Tear Surface Parameters