J Korean Ophthalmol Soc.
2012 Oct;53(10):1505-1511.
Characteristics and Prognostic Factors of Open-Globe Injuries in Korea
- Affiliations
-
- 1Department of Ophthalmology, Yonsei University College of Medicine, Seoul, Korea. sklee219@yuhs.ac
Abstract
- PURPOSE
To characterize epidemiologically open-globe injuries and to identify prognostic factors for visual outcomes after open-globe injuries in Korea.
METHODS
The medical records of 138 patients with open-globe injuries presenting to the Severance Hospital between January 2005 and June 2011 were retrospectively reviewed.
RESULTS
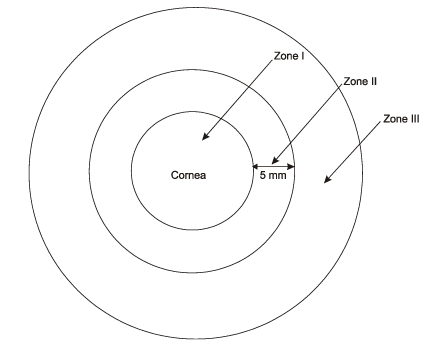
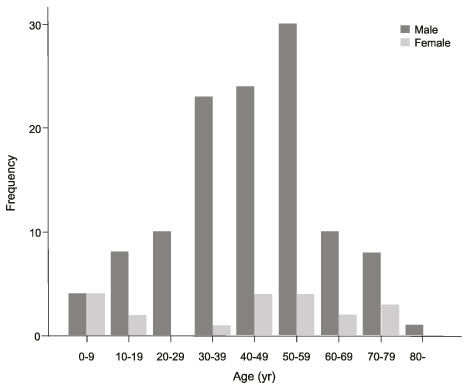
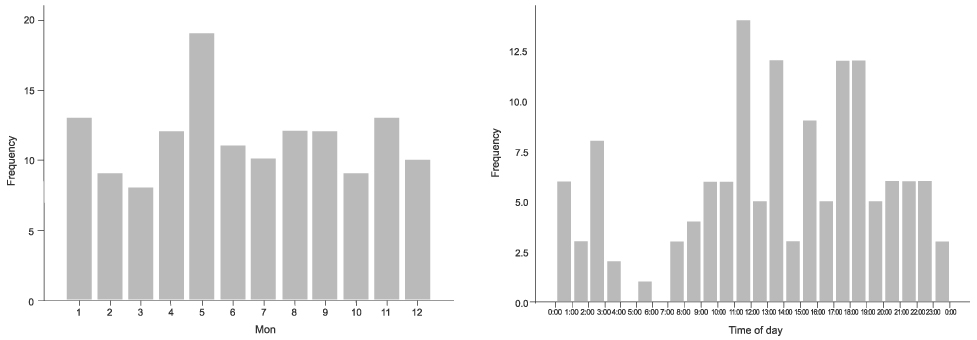
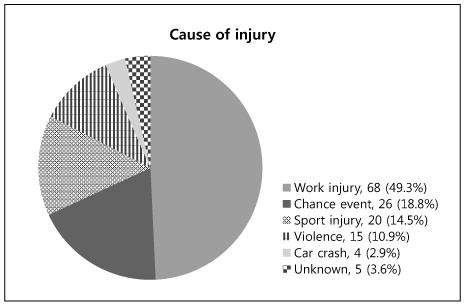
Out of 138 patients, 85.5% were men. The types of injury included penetrating injury (44.2%), intraocular foreign body (15.9%), blunt injury (35.5%), and perforating injury (3.6%). The most common cause of injury was accidents at work (49.3%) and 60.9% of these injuries were a penetrating wound in zone I limited to the cornea. Predictors of poor visual outcome using univariate analysis included wound extended to posterior sclera, wound length of 10 mm or more, poor initial visual acuity of hand motion or less, and presence of associated ocular injuries at presentation including hyphema, lens injury, vitreous hemorrhage, and retinal detachment. Initial visual acuity and wound size were independent prognostic factors of visual outcome.
CONCLUSIONS
Accidents at work are the most important cause of open-globe injuries in Korea. Accordingly, protective measures such as appropriate eyewear and safety education at work are warranted. Initial visual acuity and wound size predicted favorable visual outcome.
MeSH Terms
Figure
Reference
-
1. Négrel AD, Thylefors B. The global impact of eye injuries. Ophthalmic Epidemiol. 1998. 5:143–169.2. Koo L, Kapadia MK, Singh RP, et al. Gender differences in etiology and outcome of open globe injuries. J Trauma. 2005. 59:175–178.3. Entezari M, Rabei HM, Badalabadi MM, Mohebbi M. Visual outcome and ocular survival in open-globe injuries. Injury. 2006. 37:633–637.4. Wong TY, Klein BE, Klein R. The prevalence and 5-year incidence of ocular trauma. The Beaver Dam Eye Study. Ophthalmology. 2000. 107:2196–2202.5. May DR, Kuhn FP, Morris RE, et al. The epidemiology of serious eye injuries from the United States Eye Injury Registry. Graefes Arch Clin Exp Ophthalmol. 2000. 238:153–157.6. Schmidt GW, Broman AT, Hindman HB, Grant MP. Vision survival after open globe injury predicted by classification and regression tree analysis. Ophthalmology. 2008. 115:202–209.7. Man CY, Steel D. Visual outcome after open globe injury: a comparison of two prognostic models--the Ocular Trauma Score and the Classification and Regression Tree. Eye (Lond). 2010. 24:84–89.8. Kuhn F, Morris R, Witherspoon CD. Birmingham Eye Trauma Terminology (BETT): terminology and classification of mechanical eye injuries. Ophthalmol Clin North Am. 2002. 15:139–143. v9. Kuhn F, Maisiak R, Mann L, et al. The Ocular Trauma Score (OTS). Ophthalmol Clin North Am. 2002. 15:163–165. vi10. Pieramici DJ, Sternberg P Jr, Aaberg TM Sr, et al. A system for classifying mechanical injuries of the eye (globe). The Ocular Trauma Classification Group. Am J Ophthalmol. 1997. 123:820–831.11. Esmaeli B, Elner SG, Schork MA, Elner VM. Visual outcome and ocular survival after penetrating trauma. A clinicopathologic study. Ophthalmology. 1995. 102:393–400.12. Rahman I, Maino A, Devadason D, Leatherbarrow B. Open globe injuries: factors predictive of poor outcome. Eye (Lond). 2006. 20:1336–1341.13. Han SB, Yu HG. Visual outcome after open globe injury and its predictive factors in Korea. J Trauma. 2010. 69:E66–E72.14. Hyun Lee S, Ahn JK. Emergent risk factors associated with eyeball loss and ambulatory vision loss after globe injuries. J Trauma. 2010. 69:195–198.15. Rofail M, Lee GA, O'Rourke P. Prognostic indicators for open globe injury. Clin Experiment Ophthalmol. 2006. 34:783–786.16. Andreoli MT, Andreoli CM. Geriatric traumatic open globe injuries. Ophthalmology. 2011. 118:156–159.17. Han SB, Yang HK, Woo SJ, et al. Association of alcohol consumption with the risk of ocular trauma. J Korean Med Sci. 2011. 26:675–678.18. Nashed A, Saikia P, Herrmann WA, et al. The outcome of early surgical repair with vitrectomy and silicone oil in open-globe injuries with retinal detachment. Am J Ophthalmol. 2011. 151:522–528.19. Sandinha MT, Newman W, Wong D, Stappler T. Outcomes of delayed vitrectomy in open-globe injuries in young patients. Retina. 2011. 31:1541–1544.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Predictability of Ocular Trauma Score and Prognostic Factors of Open Globe Injury
- The Relationship between Visual Outcome and Ocular Trauma Score after Open Globe Injuries in Children
- The Availability of Modified Ocular Trauma Score in Korean Patients with Open Globe Injury
- The Role of Orbital Computed Tomography as a Prognostic Indicator for Open Globe Injury
- Changes in the Clinical Manifestations of Ocular Injuries Induced by Power Lawn Mowers