J Korean Ophthalmol Soc.
2011 Feb;52(2):136-140.
Correction of Lower Lid Retraction Using Autologous Ear Cartilage Graft
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University College of Medicine, Seoul, Korea. resourceful@hanmail.net
- 2Seoul Artificial Eye Center, Seoul National University Hospital Clinical Research Institute, Seoul, Korea.
- 3Department of Ophthalmology, Seoul National University Hospital, Seoul, Korea.
- 4Department of Ophthalmology, Seoul National University Bundang Hospital, Seongnam, Korea.
- 5Department of Ophthalmology, SMG-SNU Boramae Medical Center, Seoul, Korea.
Abstract
- PURPOSE
To evaluate the surgical results of lower eyelid retraction using autologous ear cartilage graft.
METHODS
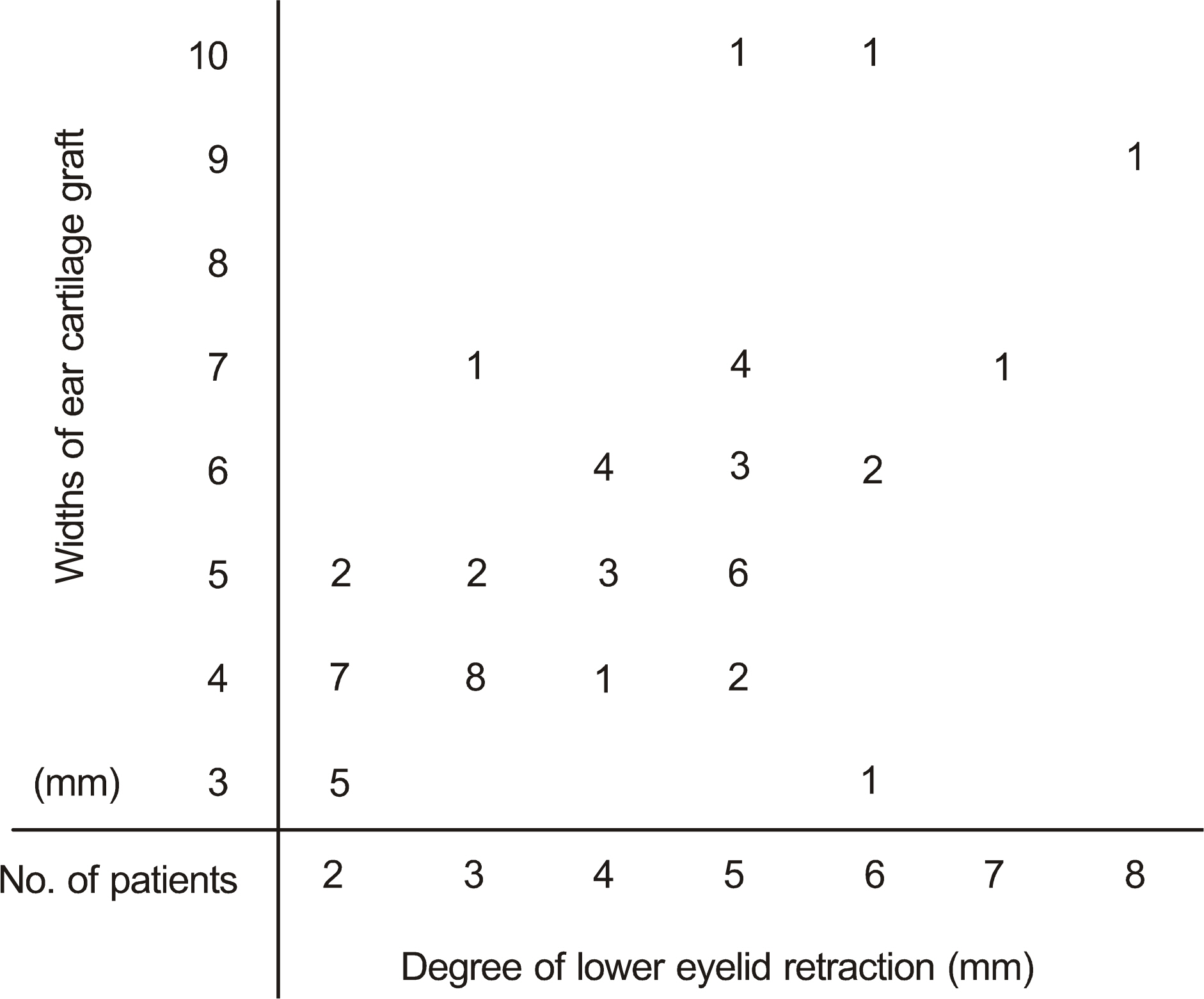
Fifty patients (54 eyes) who received surgical correction of lower eyelid retraction by lower eyelid retractors and conjunctiva recession from the tarsal plate with autologous ear cartilage grafts from March 2002 to July 2010 were evaluated. Medical records were reviewed and clinical characteristics, surgical outcomes, and postoperative complications were analyzed retrospectively.
RESULTS
The use of prosthesis due to anophthalmos or microphthalmos (22 eyes) was the most common cause of lower eyelid retraction. The mean postoperative follow-up period was 16.6 months (1-98 months). Lower eyelid retraction was successfully corrected in 52 of 54 eyes. Postoperatively, 2 cases of corneal erosions, 1 case of conjunctival erosion, and 2 pyogenic granulomas developed. Corneal and conjunctival erosions resolved with conservative management and granulation tissues were removed by excision.
CONCLUSIONS
Correction of lower eyelid retraction using autologous ear cartilage graft is an excellent surgical procedure with low complication rates for eyelid retraction of various etiologies.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Baylis HI, Perman KI, Fett DR, Sutcliffe RT. Autogenous auricular cartilage grafting for lower eyelid retraction. Ophthal Plast Reconstr Surg. 1985; 1:23–7.
Article2. Mann F, Roussat B. Surgical treatment of lower eyelid retraction occurring after inferior rectus recession: a case report of a patient with congenital fibrosis of the extraocular muscles. J Fr Ophtalmol. 2008; 31:605–8.3. Kim YK, Kim JW. Evaluation of subciliary incision used in blowout fracture treatment: pretarsal flattening after lower eyelid surgery. Plast Reconstr Surg. 2010; 125:1479–84.
Article4. Olver JM, Rose GE, Khaw PT, Collin JR. Correction of lower eyelid retraction in thyroid eye disease: a randomised controlled trial of retractor tenotomy with adjuvant antimetabolite versus scleral graft. Br J Ophthalmol. 1998; 82:174–80.
Article5. Wearne MJ, Sandy C, Rose GE, et al. Autogenous hard palate mucosa: the ideal lower eyelid spacer? Br J Ophthalmol. 2001; 85:1183–7.
Article6. Li TG, Shorr N, Goldberg RA. Comparison of the efficacy of hard palate grafts with acellular human dermis grafts in lower eyelid surgery. Plast Reconstr Surg. 2005; 116:873–8.7. Marks MW, Argenta LC, Friedman RJ, Hall JD. Conchal cartilage and composite grafts for correction of lower lid retraction. Plast Reconstr Surg. 1989; 83:629–35.8. Smith RJ, Malet T. Auricular cartilage grafting to correct lower conjunctival fornix retraction and eyelid malposition in anophthalmic patients. Ophthal Plast Reconstr Surg. 2008; 24:13–8.9. Baylis HI, Rosen N, Neuhaus RW. Obtaining auricular cartilage for reconstructive surgery. Am J Ophthalmol. 1982; 93:709–12.
Article10. Moon JW, Choung HK, Khwarg SI. Correction of lower lid retraction combined with entropion using an ear cartilage graft in the anophthalmic socket. Korean J Ophthalmol. 2005; 19:161–7.
Article11. Aldave AJ, Maus M, Rubin PA. Advances in the management of lower eyelid retraction. Facial Plast Surg. 1999; 15:213–24.
Article12. Kim JW, Kikkawa DO, Lemke BN. Donor site complications of hard palate mucosal grafting. Ophthal Plast Reconstr Surg. 1997; 13:36–9.
Article13. Gardner TA, Kennerdell JS, Buerger GF. Treatment of dysthyroid lower lid retraction with autogenous tarsus transplants. Ophthal Plast Reconstr Surg. 1992; 8:26–31.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Correction of Lower Lid Retraction Combined with Entropion using an Ear Cartilage Graft in the Anophthalmic Socket
- Hard Palate Mucosa Grafts for Lower Lid Retraction
- Surgical Correction of Lower Lid Retraction Using The Scleral Spacer
- Correction of Lower Eyelid Retraction with Autogenous Hard Palate Mucosa : 2 Case Report
- Two Cases of Tragal Cartilage Graft in Rhinoplasty