J Korean Ophthalmol Soc.
2010 Oct;51(10):1409-1413.
Subretinal Fluid Collection in Patient With Non-Arteritic Anterior Ischemic Optic Neuropathy: A Case Report
- Affiliations
-
- 1Department of Ophthalmology, Soonchunhyang University College of Medicine, Seoul, Korea. ckseek@naver.com
Abstract
- PURPOSE
To report a patient with non-arteritic anterior ischemic optic neuropathy with submacular fluid and peripapillary swelling.
CASE SUMMARY
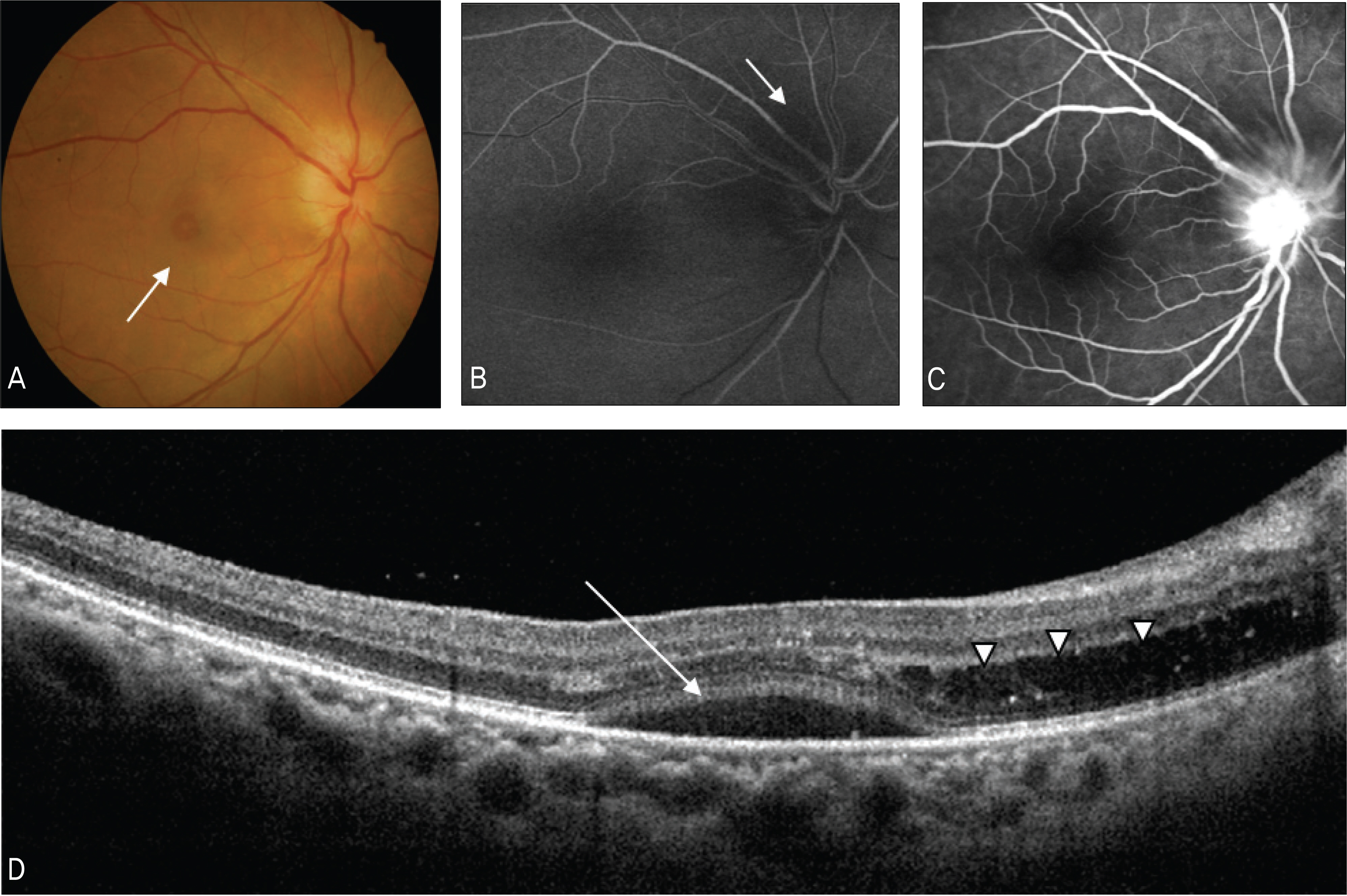
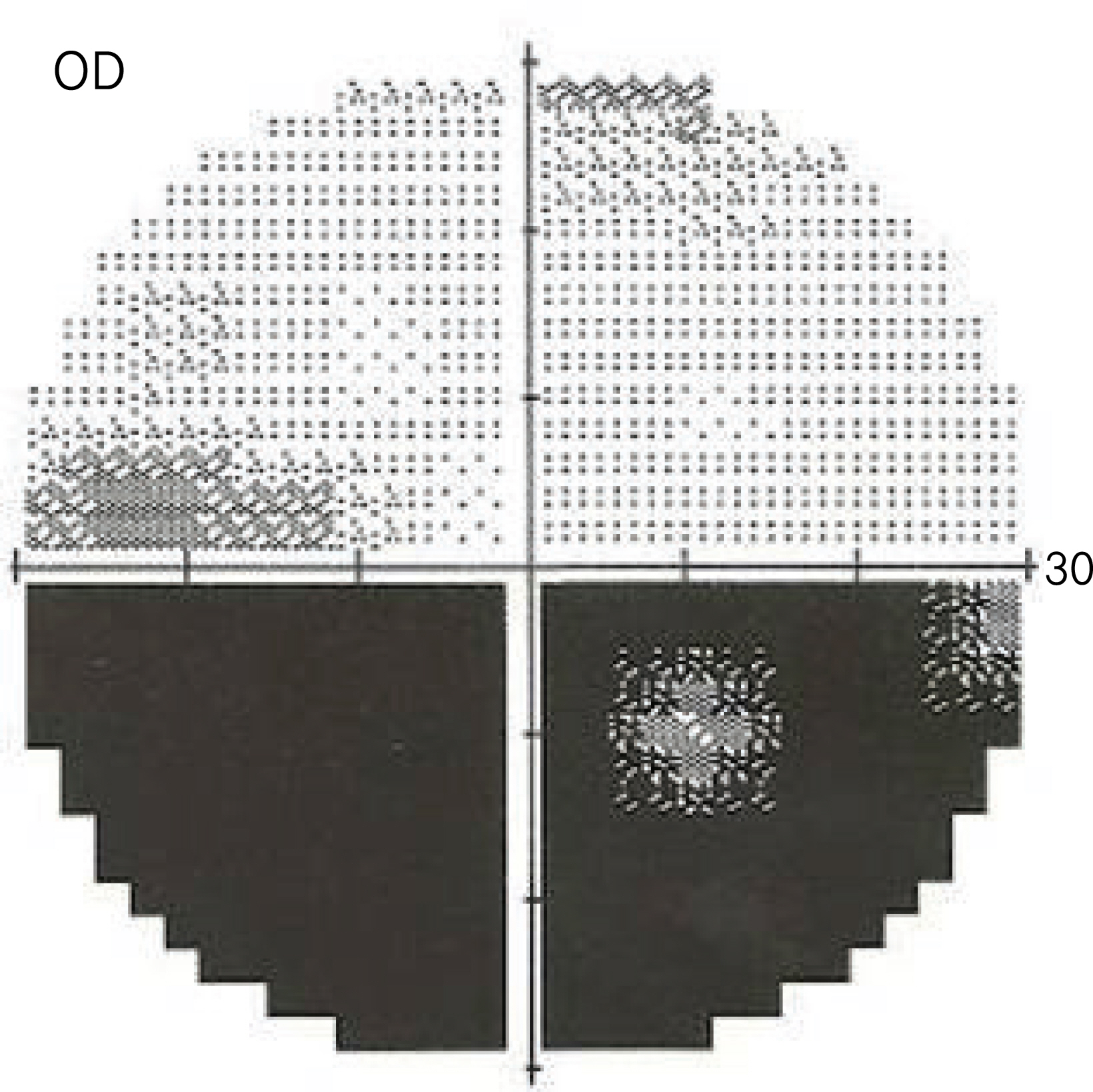
A 53-year-old patient visited our clinic complaining of acute visual loss in the right eye which began two days previously. The patient had no clinical history of ocular pain on eye movement. A relative afferent pupillary defect was observed in the right eye. Fundoscopic examination showed optic disc edema and an elevated macular lesion (1 disc diameter). Fluorescein angiography (FAG) revealed blocking by serous detachment in the peripapillary area in the early phase and peripapillary leakage in the late phase. Spectral domain optical coherence tomography (SD-OCT) showed submacular fluid and peripapillary swelling. Intravenous steroid injection was administrated. After five days of treatment, visual acuity improved to 0.2; one month later, visual acuity was 0.5. subretinal fluid absorption was observed with remaining lipid deposits.
CONCLUSIONS
In non-arteritic anterior ischemic optic neuropathy, submacular fluid accumulation can occur due to destruction of retinal glial cells. Accumulation of submacular fluid can induce sudden visual loss and may predict visual prognosis. The macular area requires careful evaluation in non-arteritic anterior ischemic optic neuropathy patients.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Beri M, Klugman MR, Kohler JA, Hayreh SS. Anterior ischemic optic neuropathy. VII. Incidence of bilaterality and various influencing factors. Ophthalmology. 1987; 94:1020–8.2. Hayreh SS. Ischemic optic neuropathy. Prog Retin Eye Res. 2009; 28:34–62.
Article3. Hedges TR 3rd, Vuong LN, Gonzalez-Garcia AO. Subretinal fluid from anterior ischemic optic neuropathy demonstrated by optical coherence tomography. Arch Ophthalmol. 2008; 126:812–5.
Article4. Hoye VJ 3rd, Berrocal AM, Hedges TR 3rd, et al. Optical coherence tomography demonstrates subretinal macular edema from papilledema. Arch Ophthalmol. 2001; 119:1287–90.
Article5. Hayreh SS. Fluids in the anterior part of the optic nerve in health and disease. Surv Ophthalmol. 1978; 23:1–25.
Article6. Bolz M, Schmidt-Erfurth U, Deak G, et al. Optical coherence tomographic hyperreflective foci: a morphologic sign of lipid ex-travasation in diabetic macular edema. Ophthalmology. 2009; 116:914–20.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Anterior Ischemic Optic Neuropethy
- A Case of Non-Arteritic Anterior Ischemic Optic Neuropathy after Bilateral Selective Neck Dissection
- A Case of Subtype Giant Cell Arteritis Without Symptoms of Arteritic Anterior Ischemic Optic Neuropathy
- Temporal Arteritis with Diagnostic Brain Magnetic Resonance Imaging
- A Case of Acute Nonarteritic Anterior Ischemic Optic Neuropathy in Patient on Hemodialysis