J Korean Ophthalmol Soc.
2010 Aug;51(8):1047-1053.
Clinical Effects of Combination Therapy Using Heparin and Phospholipid in Severe Dry Eye Syndrome
- Affiliations
-
- 1Department of Ophthalmology, Chung-Ang University College of Medicine, Seoul, Korea. JCK50ey@kornet.net
Abstract
- PURPOSE
To evaluate the therapeutic effects of topical heparin (Hylo-Parin(R), Ursapharm Saarbr cken, Germany) and spray type phospholipids (Tears Again(R), Optima Pharmazeutische GmbH. Freising, Germany) in severe dry eye syndrome resistant to conventional therapy.
METHODS
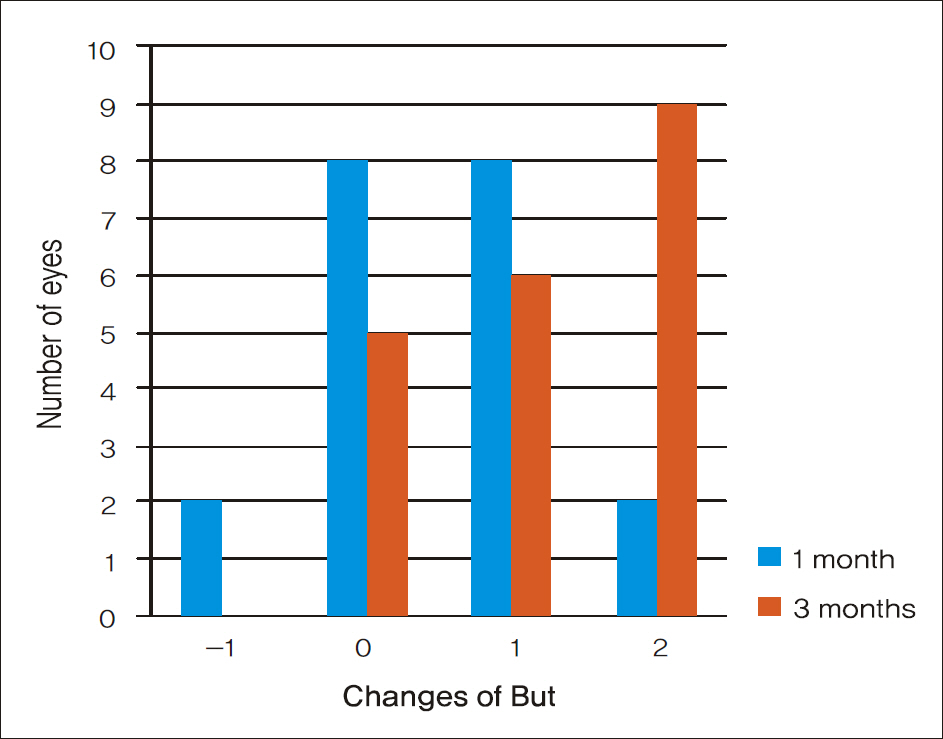
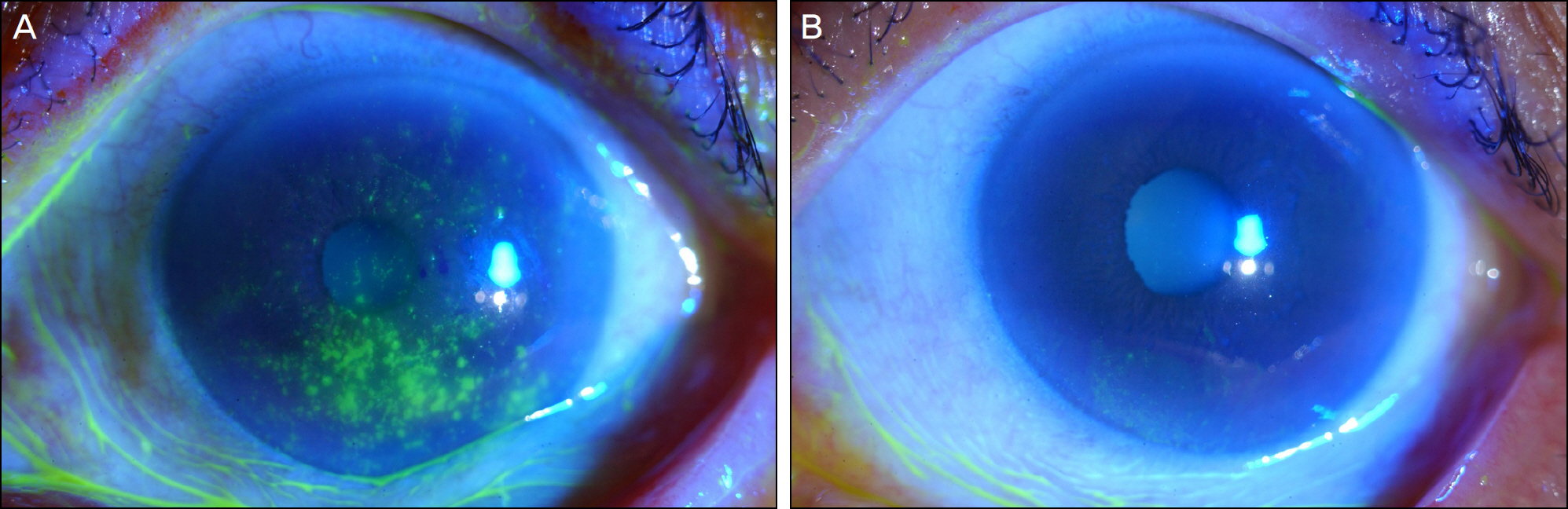
Twenty eyes of ten patients with refractory severe dry eye were treated with Hylo-Parin(R) (two times a day) and Tears Again(R) (three times a day) for three months. Before and one and three months after treatment, a symptom questionnaire was administered to the patients. The ocular surface disease index (OSDI), tear film break-up time, Schirmer test, conjunctival fluorescein staining examinations and filamentary keratitis were evaluated.
RESULTS
After using Tears Again(R) and Hylo-Parin(R), the OSDI score improved from 64.13 +/- 15.12 to 43.80 +/- 15.87 (p<0.01). Tear film break-up time significantly increased from 1.0 +/- 0.65 to 2.3 +/- 0.73 seconds (p<0.01) and conjunctival staining score (Oxford scale) significantly decreased from 3.85 +/- 0.75 to 3.25 +/- 0.97 (p<0.01). Filamentary keratitis in the slit-lamp examination showed significant improvement (p<0.01).
CONCLUSIONS
Tears Again(R) and Hylo-Parin(R) are considered as new treatment modalities for severe dry eye syndrome and filamentary keratitis in patients with chronic ocular surface disease resistant to conventional therapy. These treatments require additional research.
Keyword
MeSH Terms
Figure
Reference
-
References
1. The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop (2007). The Ocul Surf. 2007; 5:75–92.2. Management and therapy of dry eye disease: report of the Management and Therapy Subcommittee of the International Dry Eye WorkShop (2007). The Ocular Surface. 2007; 5:163–78.3. Bron AJ, Tiffany JM, Gouveia SM, et al. Functional aspects of the tear film lipid layer. Exp Eye Res. 2004; 78:347–60.
Article4. Albietz J, Sanfilippo P, Troutbeck R, Lenton LM. Management of filamentary keratitis associated with aqueous-deficient dry eye. Optom Vis Sci. 2003; 80:420–30.
Article5. Ubels JL, Edelhauser HF, Austin KH. Healing of experimental corneal wounds treated with topically applied retinoids. Am J Ophalmol. 1983; 95:353–8.
Article6. Hunt TK. Vitamin A and wound healing. J Am Acad Dermatol. 1986; 15:817–21.
Article7. Fujikawa A, Gong H, Amemiya T. Vitamin E prevents changes in the cornea and conjunctiva due to vitamin A deficiency. Graefes Arch Clin Exp Ophthalmol. 2003; 241:287–97.
Article8. Young E. The anti-inflammatory effects of heparin and related compounds. Thromb Res. 2008; 122:743–52.
Article9. Rabenstein DL. Heparin and heparin sulfate: structure and function. Nat Prod Rep. 2002; 19:312–31.10. Upchurch GR, Valeri CR, Khuri SF, et al. Effect of heparin on fibrinolytic activity and platelet function in vivo. Am J Physiol. 1996; 271:528–34.11. Bron AJ, Evans VE, Smith JA. Grading of corneal and conjunctival staining in the context of other dry eye tests. Cornea. 2003; 22:640–50.
Article12. Schiffman RM, Christianson MD, Jacobsen G, et al. Reliability and validity of the ocular surface disease index. Arch Ophthalmol. 2000; 118:615–21.
Article13. Her J, Yu SI, Seo SG. Clinical effects of various antiinflammatory therapies in dry eye syndrome. J Korean Ophthalmol Soc. 2006; 47:1901–10.14. Fareed J, Walenga JM, Hoppensteadt , Messmore HL. Studies on the profibrinolytic actions of heparin and its function. Semin Thromb Hemost. 1985; 11:199–207.15. Mousa S, Fareed J, Iqbal O, Kaiser B. Tissue factor pathway inhibitor in thrombosis and beyond. Methods Mol Med. 2004; 93:133–55.
Article16. Kumar R, Katare OP. Lecithin organogels as a potential phospholi-pid-structured system for topical drug delivery. AAPS Pharm Sci Tech. 2005; 6:298–310.17. Filion MC, Phillips NC. Anti-inflammatory activity of cationic lipids. Br J Pharmacol. 1997; 122:551–7.
Article18. Alving CR. Immunologic aspects of liposomes: presentation and processing of liposomal protein and phospholipid antigens. Biochim. Biophy. Acta. 1992; 1113:307–22.19. Ramos CG, Fernandes D, Charão CT, et al. Apoptotic mimicry: phosphatidylserine liposomes reduce inflammation through activation of peroxisome proliferator-activated receptors (PPARs) in vivo. Br Pharmacol. 2007; 151:844–50.
Article20. Yamada M, Mochizuki H, Kawashima M, Hata S. Phospholipids and their degrading enzyme in the tears of soft contact lens wearers. Cornea. 2006; 25:68–72.
Article21. Nakamura S, Shibuya M, Nakashima H. Involvement of oxidative stress on corneal epithelial alterations in a blink-suppressed dry eye. Invest Ophthal Vis Sci. 2007; 48:1552–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recent treatment of dry eye
- Prevalence and Clinical Aspects of Sjogren Syndrome in Dry Eye Patients
- Clinical Effects of Various Antiinflammatory Therapies in Dry Eye Syndrome
- Effects of Carbomer Eye Gels on the Ocular Surface in Dry Eye Patients
- Assessment of the Compliance with 0.1% Cyclosporine A in Dry-Eye Patients with Sjögren's Syndrome