J Korean Ophthalmol Soc.
2010 Jan;51(1):35-41.
Primary Combined Photodynamic Therapy and Intravitreal Bevacizumab Injection for Neovascular Age-related Macular Degeneration
- Affiliations
-
- 1MyungGok Eye Research Institute, Konyang University, Kim's Eye Hospital, Seoul, Korea.
- 2Department of Ophthalmology, College of Medicine, Konyang University, Deajeon, Korea. idoc@kimeye.com
Abstract
- PURPOSE
To investigate the efficacy of the combined treatment of photodynamic therapy (PDT) with verteporfin and intravitreal bevacizumab in patients with neovascular age-related macular degeneration.
METHODS
Forty-five eyes received a single session of PDT following three intravitreal bevacizumab (1.25 mg) injections at six-week intervals (IVB+PDT group). Twenty-seven eyes received three intravitreal bevacizuamb (1.25 mg) injections only at six-week intervals (IVB group).
RESULTS
After the six months of follow up, the mean BCVA (LogMAR) changed significantly from 0.62+/-0.34 to 0.56+/-0.33 in the IVB group (p=0.03) and from 0.61+/-0.33 to 0.48+/-0.21 in the IVB+PDT group (p=0.001). The mean BCVA was more improved in the IVB+PDT group (p=0.049). The mean CMT changes were significant in both groups immediately after treatment, but there was no significant difference at six months between the two groups. Ten eyes (37.0%) in the IVB group and 12 eyes (26.7%) in the IVB+PDT group required retreatments during the six months of follow-up (p=0.02).
CONCLUSIONS
Significant improvement in visual acuity and reduction in central macular thickness over a six-months period were observed in both groups. The mean visual acuity was significantly better and the rate of reinjections after the initial treatment schedule was lower in the IVB+PDT group.
Keyword
MeSH Terms
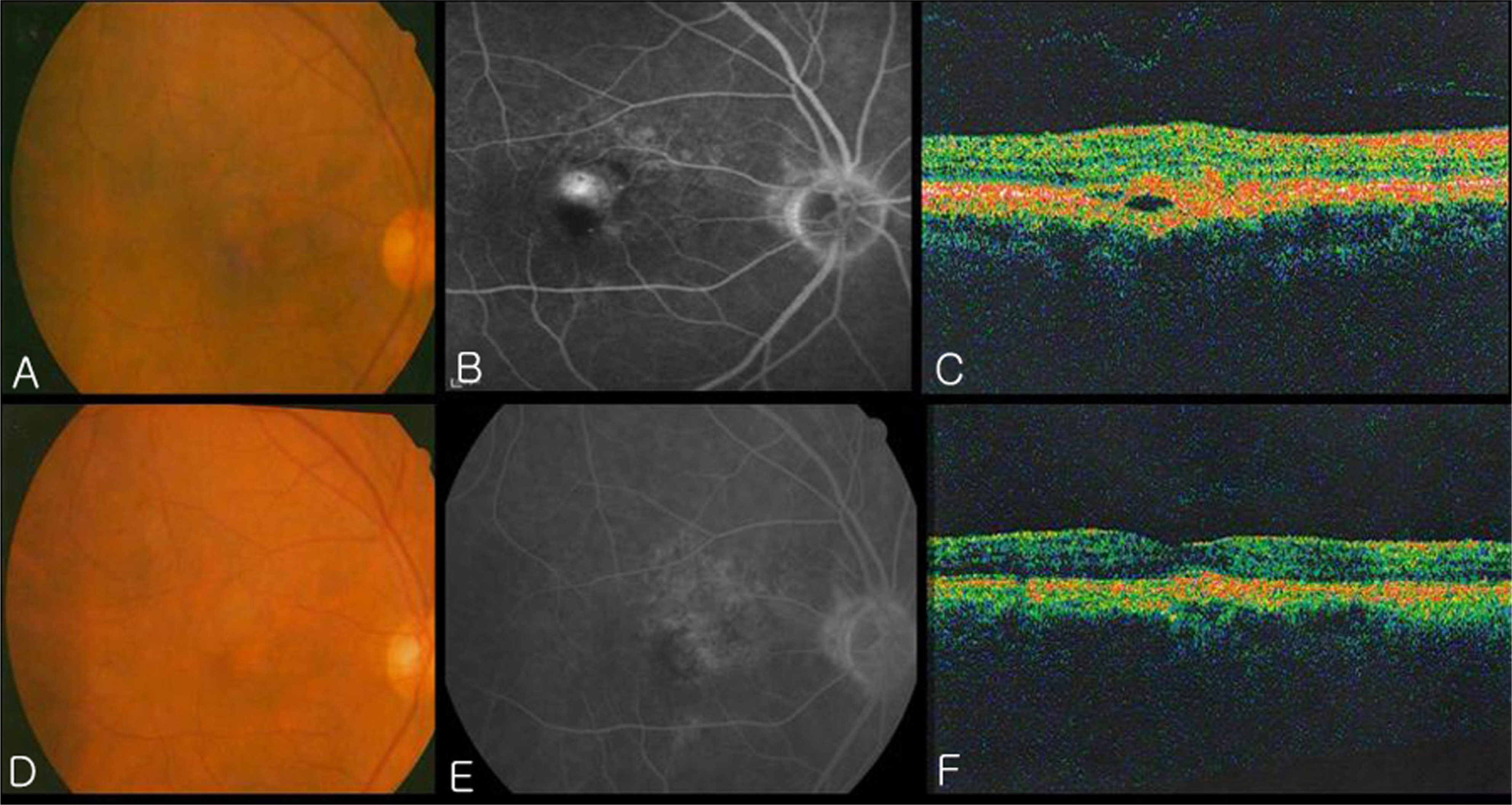
Figure
Reference
-
References
1. Polito A, Isola M, Lanzetta P, et al. The natural history of occult choroidal neovascularization associated with age-related macular degeneration: a systemic review. Ann Acad Med Singapore. 2006; 35:145–50.2. Macular Photocoagulation Study group. Subfoveal neovascular lesions in age related macular degeneration: guidelines for aberrations and treatment in the macular photocoagulation study. Arch Ophthalmol. 1991; 109:1242–57.3. Treatment of Age related macular degeneration with aberrations Therapy (TAP) Study Group. Photodynamic therapy of subfoveal choroidal neovascularization in age related macular degeneration with verteporfin: two-year results of 2 randomized clinical trials-TAP report 2. Arch Ophthalmol. 2001; 119:198–207.4. Emerson MV, Lauder AK, Flaxel CJ, et al. Intravitreal aberrations(Avastin) treatment of neovascular age-related macular aberrations. Retina. 2007; 27:439–44.5. Bashshur ZF, Schakal A, Hamam RN, et al. Intravitreal aberrations vs. verteporfin photodynamic therapy for neovascular age-related macular degeneration. Arch Ophthalmol. 2007; 125:1357–61.6. Ferrara N. Vascular endothelial growth factor: basic science and clinical progress. Endocr Rev. 2004; 25:581–611.
Article7. Adamis AP, Shima DT. The role of vascular endothelial growth factor in ocular health and disease. Retina. 2005; 25:111–8.
Article8. Lazic R, Gabric N. Verteporfin therapy and intravitreal aberrations combined and alone in choroidal neovascularization due to age-related macular degeneration. Ophthalmology. 2007; 114:1179–85.9. Ladas ID, Kotsolis AI, Papakostas TD, et al. Intravitreal aberrations combined with photodynamic therapy for the treatment of occult choroidal neovascularization associated with serous aberrations epithelium detachment in age-related macular degeneration. Retina. 2007; 27:891–6.10. Bressler SB, Bressler NM, Fine SL, et al. Natural course of aberrations neovascular membranes within the foveal avascular zone in senile macular degeneration. Am J Ophthalmol. 1982; 93:157–63.11. Guyer DR, Fine SL, Maguine MG, et al. Subfoveal choroidal aberrations membranes in age-related macular degeneration. Visual prognosis in eyes with relatively good visual acuity. Arch aberrations. 1986; 104:702–5.12. Emerson MV, Lauder AK, Flaxel CJ, et al. Intravitreal aberrations(Avastin) treatment of neovascular age-related macular aberrations. Retina. 2007; 27:439–44.13. Lynch SS, Cheng CM. Bevacizumab for neovascular ocular aberrations. Ann Pharmacother. 2007; 41:614–25.14. Bressler NM, Chang TS, Fine JT, et al. Improved vision-related function after ranibizumab vs. photodynamic therapy: a aberrations clinical trial. Arch Ophthalmol. 2009; 127:13–21.15. Fintak DR, Shah GK, Blinder KJ, et al. Incidence of aberrations related to intravitreal injection of bevacizumab and aberrations. Retina. 2008; 28:1395–9.16. Mason JO 3rd, White MF, Feist RM, et al. Incidence of acute onset endophthalmitis following intravitreal bevacizumab (Avastin) injection. Retina. 2008; 28:564–7.
Article17. Yenerel NM, Dinc UA, Gorgun E. A case of sterile aberrations after repeated intravitreal bevacizumab injection. J Ocul Pharmacol Ther. 2008; 24:362–3.18. Heier JS, Boyer DS, Ciulla TA, et al. Ranibizumab combined with verteporfin photodynamic therapy in neovascular agerelated aberrations degeneration. Arch Ophthalmol. 2006; 124:1532–42.19. Augustin AJ, Puls S, Offermann I. Triple therapy for choroidal neovascularization due to age-related macular degeneration: aberrations PDT, Bevacizumab and Dexamethasone. Retina. 2007; 27:133–40.20. Ladewig MS, Karl SE, Hamelmann V, et al. Combined intravitreal bevacizumab and photodynamic therapy for neovascular age-related macular degeneration. Graefes Arch Clin Exp aberrations. 2008; 246:17–25.
Article21. Brown DM, Kaiser PK, MIchels M, et al. ANCHOR study group. Ranibizumab versus verteporfin for neovascular age-related aberrations degeneration. N Eng J Med. 2006; 335:1432–44.22. Fung AE, Lalwani GA, Rosenfeld PJ, et al. An optical coherence tomography-guided, variable dosing regimen with intravitreal ranibizumab (Lucentis) for neovascular age-related macular aberrations. Am J Ophthalmol. 2007; 143:566–83.23. Oh SB, Cho WB, Moon JW, Kim HC. Effect and prognostic factors of intravitreal bevacizumab on choroidal neovascularization from age-related macular degeneration. J Korean Ophthalmol Soc. 2009; 50:202–10.24. Kaiser PK, Blodi BA, Shapiro H, et al. Angiographic and optical coherence tomographic results of the MARINA study of aberrations in neovascular age-related macular degeneration. aberrationsmology. 2007; 114:1868–75.25. Kim YH, Kim ES, Yu SY, Kwak HW. Long-term effect of aberrations bevacizumab for CNV secondary to age-related macular degeneration. J Korean Ophthalmol Soc. 2008; 49:1935–40.26. Treatment of age-related macular degeneration with aberrations therapy and Verteporfin in photodynamic therapy study groups. Effect of lesion size, visual acuity. and lesion composition on visual acuity change with and without Verteporfin therapy for choroidal neovascularization secondary to age-related macular degeneration: TAP and VIP Report No.1 Am J Ophthalmol. 2003; 136:407–18.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Combined Photodynamic Therapy and Intravitreal Bevacizumab Injection for Exudative Age-Related Macular Degeneration and Polypoidal Choroidal Vasculopathy
- Treatment of Exudative Age-Related Macular Degeneration
- Multifocal Electroretinogram Findings after Intravitreal Bevacizumab Injection in Choroidal Neovascularization of Age-Related Macular Degeneration
- Retinal Detachment with Macular Hole Following Combined Photodynamic Therapy and Intravitreal Bevacizumab Injection
- Effect of Photodynamic Therapy and Intravitreal Triamcinolone Acetonide on Choroidal Neovascularization in Age-related Macular Degeneration