J Korean Ophthalmol Soc.
2009 Nov;50(11):1605-1610.
Factors Affecting the Ocular Response Analyzer Parameters in Normal Korean
- Affiliations
-
- 1Department of Ophthalmology, Inje university, Pusan Paik Hospital, Busan, Korea. seossg@hanmail.net
- 2Crystal Eye Hospital, Busan, Korea.
Abstract
- PURPOSE
To identify the normal range of factors which can be measured with Ocular Response Analyzer (ORA, Reichert Inc., Depew, NY, USA) in normal Korean, and to analyze factors affecting ORA by measuring intraocular pressure (IOP) of noncontact tonometer (NCT) and central corneal thickness (CCT).
METHODS
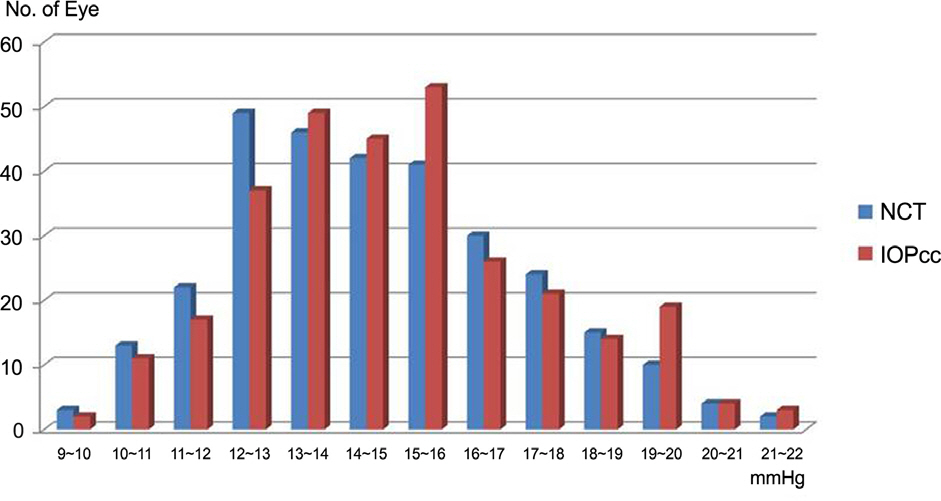
Three hundred and one normal Korean subjects who did not have specific ophthalmological diseases and surgeries in the past were recruited for this study. Corneal hysteresis (CH), corneal response factor (CRF), corneal-compensated IOP (IOPcc), and Goldmann correlated IOP (IOPg) were measured using ORA. In addition, IOP of NCT and CCT were measured and the results and factors analyzed.
RESULTS
The mean CH measured among normal Korean subjects in this study was 10.70 mmHg. The mean CRF was 10.40 mmHg. CH and CRF were significantly higher in the juvenile group. IOPcc and IOPg as measures of IOP using the ORA had significant correlation with IOP of NCT. In particular, IOPcc appeared to be independent of CCT.
CONCLUSIONS
CH and CRF were different according to age, indicating a difference in biomechanical properties of the cornea. In particular, IOPcc is more important as it is independent of corneal thickness and should be compensated in general measurements of IOP reflecting biomechanical properties.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Dupps WJ Jr. Hysteresis: new mechanospeak for the ophthalmologist. J Cataract Refract Surg. 2007; 33:1499–501.
Article2. Luce DA. Determining in vivo biomechanical properties of the cornea with an ocular response analyzer. J Cataract Refract Surg. 2005; 31:156–62.
Article3. Touboul D, Roberts C, Kérautret J, et al. Correlations between corneal hysteresis, intraocular pressure, and corneal central pachy-metry. J Cataract Refract Surg. 2008; 34:616–22.
Article4. Hager A, Schroeder B, Sadeghi M, et al. The influence of corneal hysteresis and corneal resistance factor on the measurement of intraocular pressure. Ophthalmologe. 2007; 104:484–9.5. Broman AT, Congdon NG, Bandeen-Roche K, Quigley HA. Influence of corneal structure, corneal responsiveness, and other ocular parameters on tonometric measurement of intraocular pressure. J Glaucoma. 2007; 16:581–8.
Article6. Lam A, Chen D, Chiu R, Chui WS. Comparison of IOP measure-ments between ORA and GAT in normal Chinese. Optom Vis Sci. 2007; 84:909–14.
Article7. Kirwan C, O'Keefe M, Lanigan B. Corneal hysteresis and intraocular pressure measurement in children using the Reichert ocular response analyzer. Am J Ophthalmol. 2006; 142:990–2.
Article8. Moreno-Montañés J, Maldonado MJ, García N, et al. Reproducibility and clinical relevance of the ocular response analyzer in nono-perated eyes: corneal biomechanical and tonometric implications. Invest Ophthalmol Vis Sci. 2008; 49:968–74.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Corneal Biomechanical Properties of Normal Tension Glaucoma in Young Patients Evaluated with the Ocular Response Analyzer
- Diagnostic Availability of Ocular Response Analyzer in Korean Patients with Normal Tension Glaucoma
- Detection of Early Visual Field Change in Ocular Hypertension Using STATPAC
- Biomechanical Property of Keratoconus Measured by ORA
- The Effect of Corneal Biomechanical Factors on Ocular Pulse Amplitude in Normal Subjects