J Korean Ophthalmol Soc.
2015 Jan;56(1):86-92. 10.3341/jkos.2015.56.1.86.
Diagnostic Availability of Ocular Response Analyzer in Korean Patients with Normal Tension Glaucoma
- Affiliations
-
- 1Institute of Ophthalmology and Optometry, Department of Ophthalmology, Ewha Womans University Medical Center, Ewha Womans University School of Medicine, Seoul, Korea. ckrey02@ewha.ac.kr
- 2Department of Ophthalmology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- KMID: 2216158
- DOI: http://doi.org/10.3341/jkos.2015.56.1.86
Abstract
- PURPOSE
To compare the parameters measured with the ocular response analyzer (ORA; Reichert Inc., Depew, NY, USA) between normal control subjects and patients with normal tension glaucoma (NTG) and to investigate clinical usefulness of ORA.
METHODS
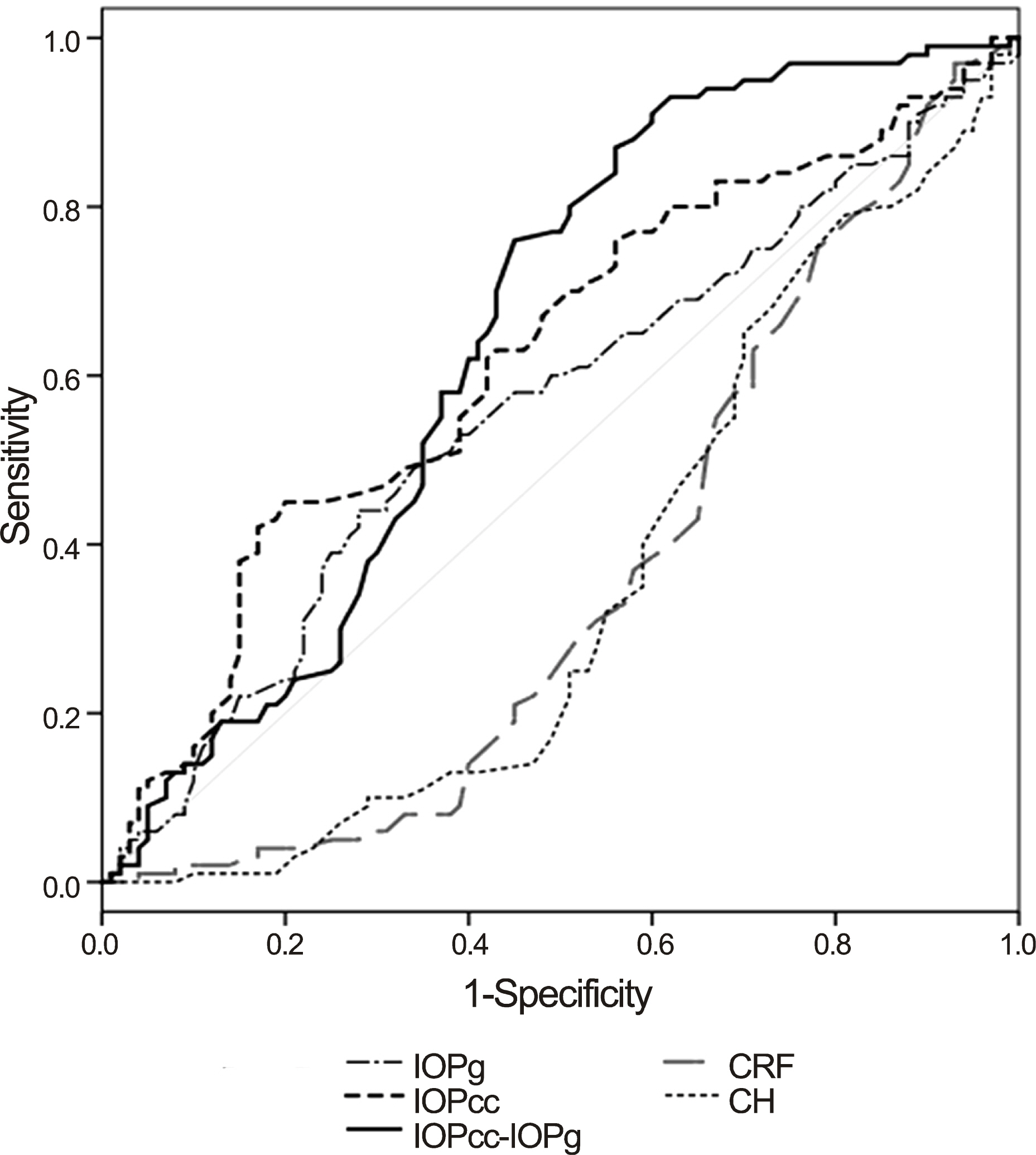
Intraocular pressure (IOP) and central corneal thickness (CCT) were measured using the Goldmann applanation tonometer (GAT) in 100 eyes of 100 normal subjects and 100 eyes of 100 NTG patients. Four types of ORA parameters, corneal hysteresis (CH), corneal resistance factor (CRF), Goldmann-correlated IOP (IOPg), and corneal-compensated IOP (IOPcc) were also measured.
RESULTS
The mean CH values were 11.2 mm Hg and 10.3 mm Hg and the mean CRF values were 10.8 mm Hg and 9.9 mm Hg in the normal subjects group and the NTG group, respectively. Mean CH and CRF were significantly lower in NTG patients (p < 0.001) and the IOPcc were higher than normal subjects (p = 0.004). IOPg was in agreement with the GAT IOP (ICC = 0.811) and IOPcc was not correlated with CCT. The cut-off value of 'IOPcc - IOPg' as the diagnostic standard parameter was -0.05 mm Hg (sensitivity; 76%, specificity; 55%).
CONCLUSIONS
IOPg measurements were similar to GAT IOP, and other ORA parameters (CH, CRF, IOPcc) were significantly different between normal subjects and NTG patients. Consequently, the difference of IOPcc and IOPg could be a useful parameter in NTG diagnosis.
Keyword
Figure
Cited by 1 articles
-
Diurnal Variation in Intraocular Pressure Measured by Ocular Response Analyzer in Korean Patients with Normal Tension Glaucoma
Yeon Jung Choi, Kyu Ryong Choi
J Korean Ophthalmol Soc. 2015;56(12):1913-1920. doi: 10.3341/jkos.2015.56.12.1913.
Reference
-
References
1. Chihara E. Assessment of true intraocular pressure: the gap between theory and practical data. Surv Ophthalmol. 2008; 53:203–18.
Article2. Gunvant P, O'Leary DJ, Baskaran M. . Evaluation of tonometric correction factors. J Glaucoma. 2005; 14:337–43.
Article3. Elsheikh A, Gunvant P, Jones SW. . Correction factors for Goldmann Tonometry. J Glaucoma. 2013; 22:156–63.
Article4. Luce DA. Determining in vivo biomechanical properties of the cornea with an ocular response analyzer. J Cataract Refract Surg. 2005; 31:156–62.
Article5. Grise-Dulac A, Saad A, Abitbol O. . Assessment of corneal biomechanical properties in normal tension glaucoma and comparison with openangle glaucoma, ocular hypertension, and normal eyes. J Glaucoma. 2012; 21:486–9.
Article6. Morita T, Shoji N, Kamiya K. . Corneal biomechanical properties in normaltension glaucoma. Acta Ophthalmol. 2012; 90:e48–53.
Article7. Kaushik S, Pandav SS, Banger A. . Relationship between corneal biomechanical properties, central corneal thickness, and intraocular pressure across the spectrum of glaucoma. Am J Ophthalmol. 2012; 153:840–9.e2.
Article8. Nessim M, Mollan SP, Wolffsohn JS. . The relationship between measurement method and corneal structure on apparent intraocular pressure in glaucoma and ocular hypertension. Cont Lens Anterior Eye. 2013; 36:57–61.
Article9. Shah S, Laiquzzaman M, Mantry S, Cunliffe I. Ocular response analyser to assess hysteresis and corneal resistance factor in low tension, open angle glaucoma and ocular hypertension. Clin Experiment Ophthalmol. 2008; 36:508–13.
Article10. Ang GS, Bochmann F, Townend J, Azuara-Blanco A. Corneal biomechanical properties in primary open angle glaucoma and normal tension glaucoma. J Glaucoma. 2008; 17:259–62.
Article11. Ehrlich JR, Radcliffe NM, Shimmyo M. Goldmann applanation tonometry compared with corneal-compensated intraocular pressure in the evaluation of primary openangle Glaucoma. BMC Ophthalmol. 2012; 12:52.
Article12. Park JH, Choi KR. The association between corneal biomechanical properties and progression of visual field loss in normal tension glaucoma. J Korean Ophthalmol Soc. 2013; 54:1757–66.
Article13. Rhew JY, Choi KR. Corneal biomechanical properties of normal tension glaucoma in young patients evaluated with the ocular response analyzer. J Korean Ophthalmol Soc. 2013; 54:280–8.
Article14. Jeon HS, Lee JS. Biomechanical property of keratoconus measured by ORA. J Korean Ophthalmol Soc. 2013; 54:869–76.
Article15. Fleiss JL. The design and analysis of clinical experiments. Newyork: Wiley Inc.;1986. p. 7.16. Congdon NG, Broman AT, Bandeen-Roche K. . Central corneal thickness and corneal hysteresis associated with glaucoma damage. Am J Ophthalmol. 2006; 141:868–75.
Article17. Medeiros FA, Meira-Freitas D, Lisboa R. . Corneal hysteresis as a risk factor for glaucoma progression: a prospective longitudinal study. Ophthalmology. 2013; 120:1533–40.
Article18. De Moraes CV, Hill V, Tello C. . Lower corneal hysteresis is associated with more rapid glaucomatous visual field progression. J Glaucoma. 2012; 21:209–13.
Article19. Wells AP, Garway-Heath DF, Poostchi A. . Corneal hysteresis but not corneal thickness correlates with optic nerve surface compliance in glaucoma patients. Invest Ophthalmol Vis Sci. 2008; 49:3262–8.
Article20. Bochmann F, Ang GS, Azuara-Blanco A. Lower corneal hysteresis in glaucoma patients with acquired pit of the optic nerve (APON). Graefes Arch Clin Exp Ophthalmol. 2008; 246:735–8.
Article21. Gordon MO, Beiser JA, Brandt JD. . The Ocular Hypertension Treatment Study: baseline factors that predict the onset of primary openangle glaucoma. Arch Ophthalmol. 2002; 120:714–20. discussion 829-30.22. Sullivan-Mee M, Billingsley SC, Patel AD. . Ocular Response Analyzer in subjects with and without glaucoma. Optom Vis Sci. 2008; 85:463–70.
Article23. Medeiros FA, Weinreb RN. Evaluation of the influence of corneal biomechanical properties on intraocular pressure measurements using the ocular response analyzer. J Glaucoma. 2006; 15:364–70.
Article24. Martinez-de-la-Casa JM, Garcia-Feijoo J, Fernandez-Vidal A. . Ocular response analyzer versus Goldmann applanation tonometry for intraocular pressure measurements. Invest Ophthalmol Vis Sci. 2006; 47:4410–4.
Article25. Detry-Morel M, Jamart J, Hautenauven F, Pourjavan S. Comparison of the corneal biomechanical properties with the Ocular Response Analyzer® (ORA) in African and Caucasian normal subjects and patients with glaucoma. Acta Ophthalmol. 2012; 90:e118–24.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Corneal Biomechanical Properties of Normal Tension Glaucoma in Young Patients Evaluated with the Ocular Response Analyzer
- The Association Between Corneal Biomechanical Properties and Progression of Visual Field Loss in Normal Tension Glaucoma
- The Measurement of Ocular Blood Flow Velocity using Doppler Ultrasound in Normal Tension Glaucoma Patients
- The Short-Term Effect of Prostaglandin Analog Monotherapy on Corneal Biomechanical Properties in Normal Tension Glaucoma Patients
- The Association between Corneal Biomechanical Properties and Initial Visual Field Defect Pattern in Normal Tension Glaucoma