J Korean Ophthalmol Soc.
2007 Aug;48(8):1028-1035.
Comparison of Changes in Higher-order Aberrations between Conventional and Wavefront-guided LASEK
- Affiliations
-
- 1Department of Ophthalmology, College of Medicine, Seoul National University, Seoul, Korea. kmk9@snu.ac.kr
- 2Artificial Eye Center of Clinical Research Institute, Seoul National University Hospital, Seoul, Korea.
Abstract
-
PURPOSE: To evaluate the postoperative higher-order aberrations (HOAs) and factors affecting postoperative changes in HOAs in eyes that underwent wavefront-guided LASEK (laser-assisted subepithelial keratectomy), compared with the eyes that underwent conventional LASEK.
METHODS
We reviewed the medical records of 221 patients who had undergone LASEK or wavefront guided LASEK with VISX WaveScan and VISX Star S4 eximer laser by a single surgeon (427 total eye operations). We matched 29 eyes of the LASEK and the wavefront LASEK groups (58 eyes total) according to the guideline: preoperative refractive power differences must be within 1 diopter and preoperative root-mean-square (RMS) of total HOAs differences must be within 0.01 micrometer. Preoperative wavefront aberrations and two-months postoperative wavefront aberrations and associated factors were compared and analyzed.
RESULTS
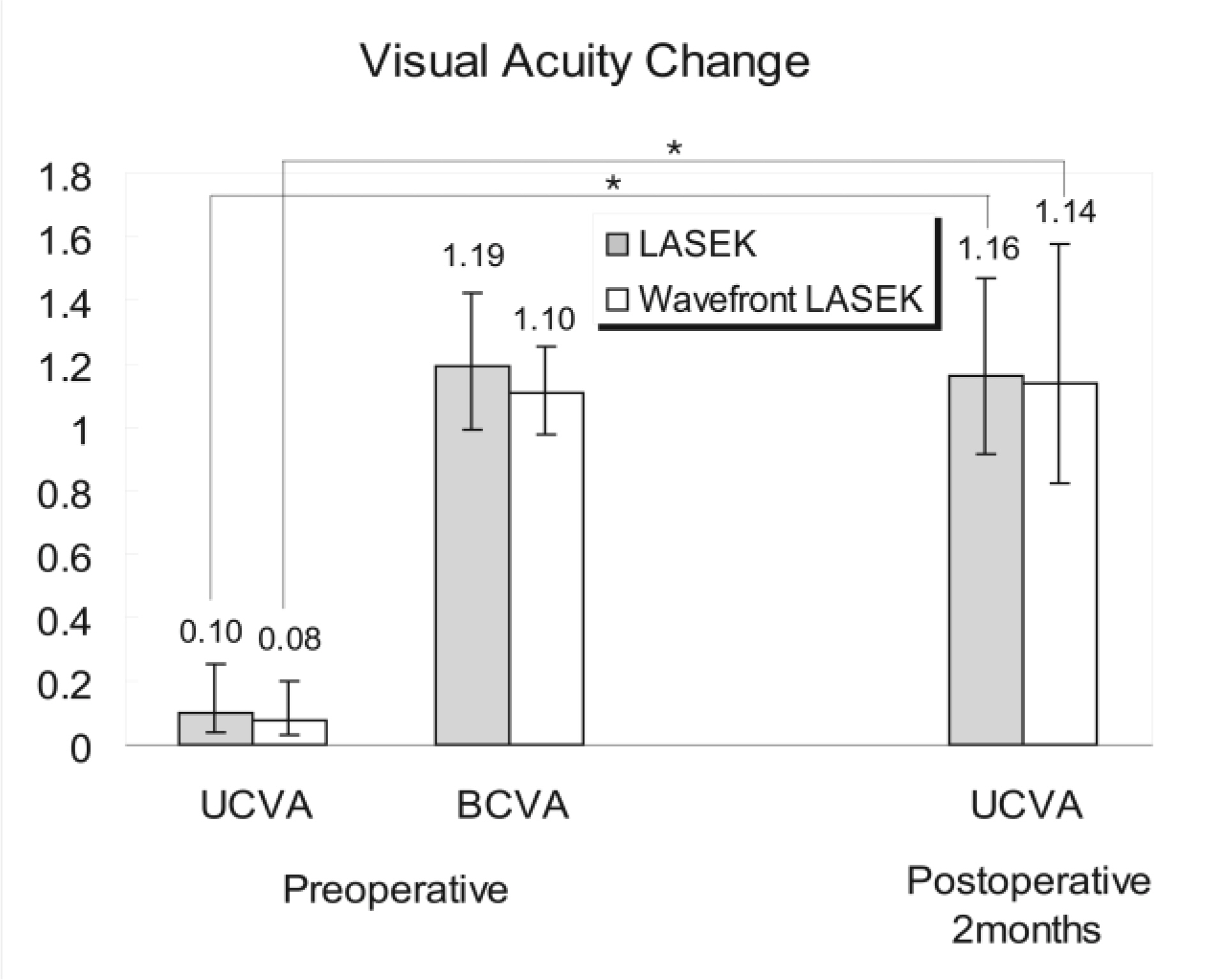
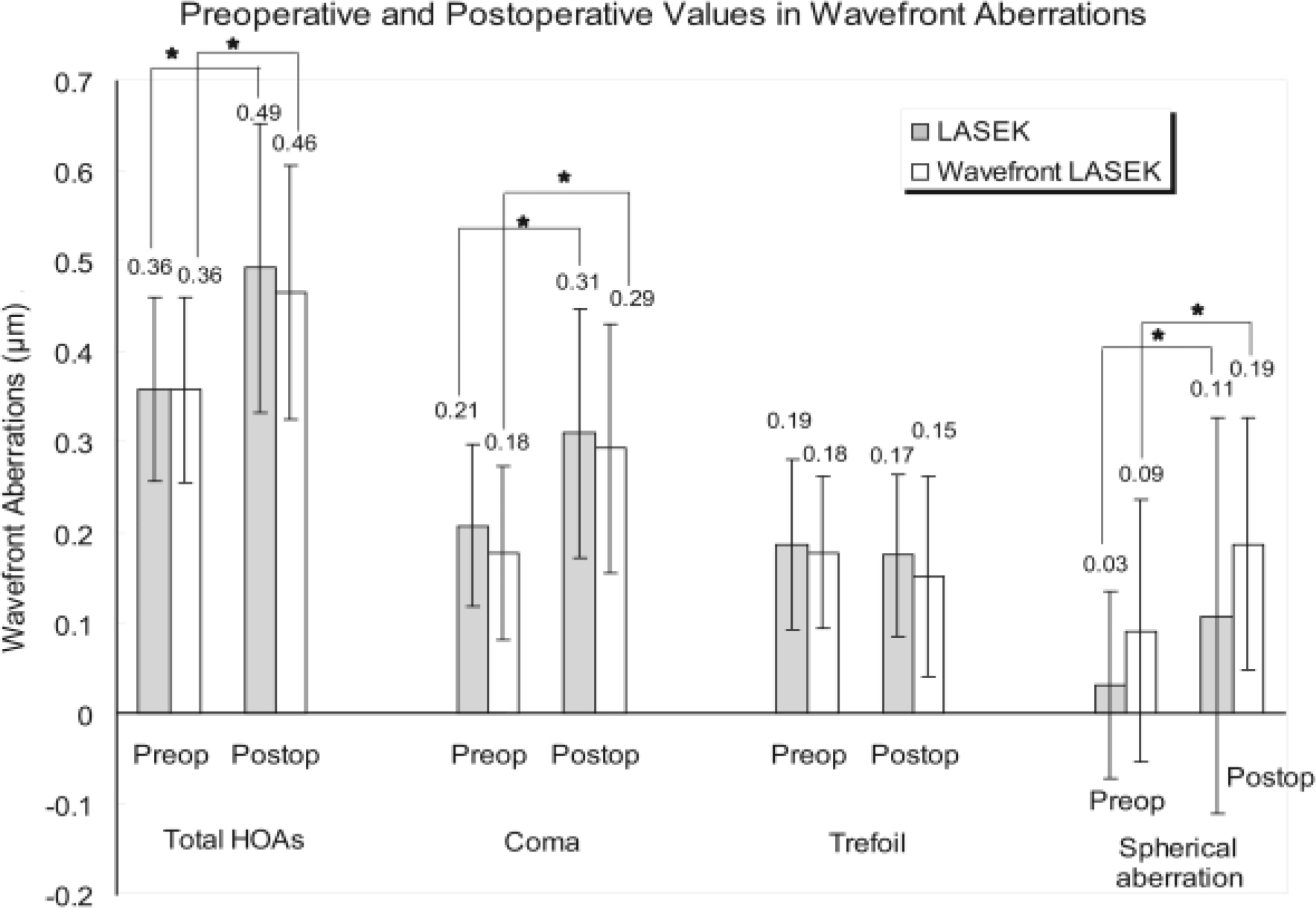
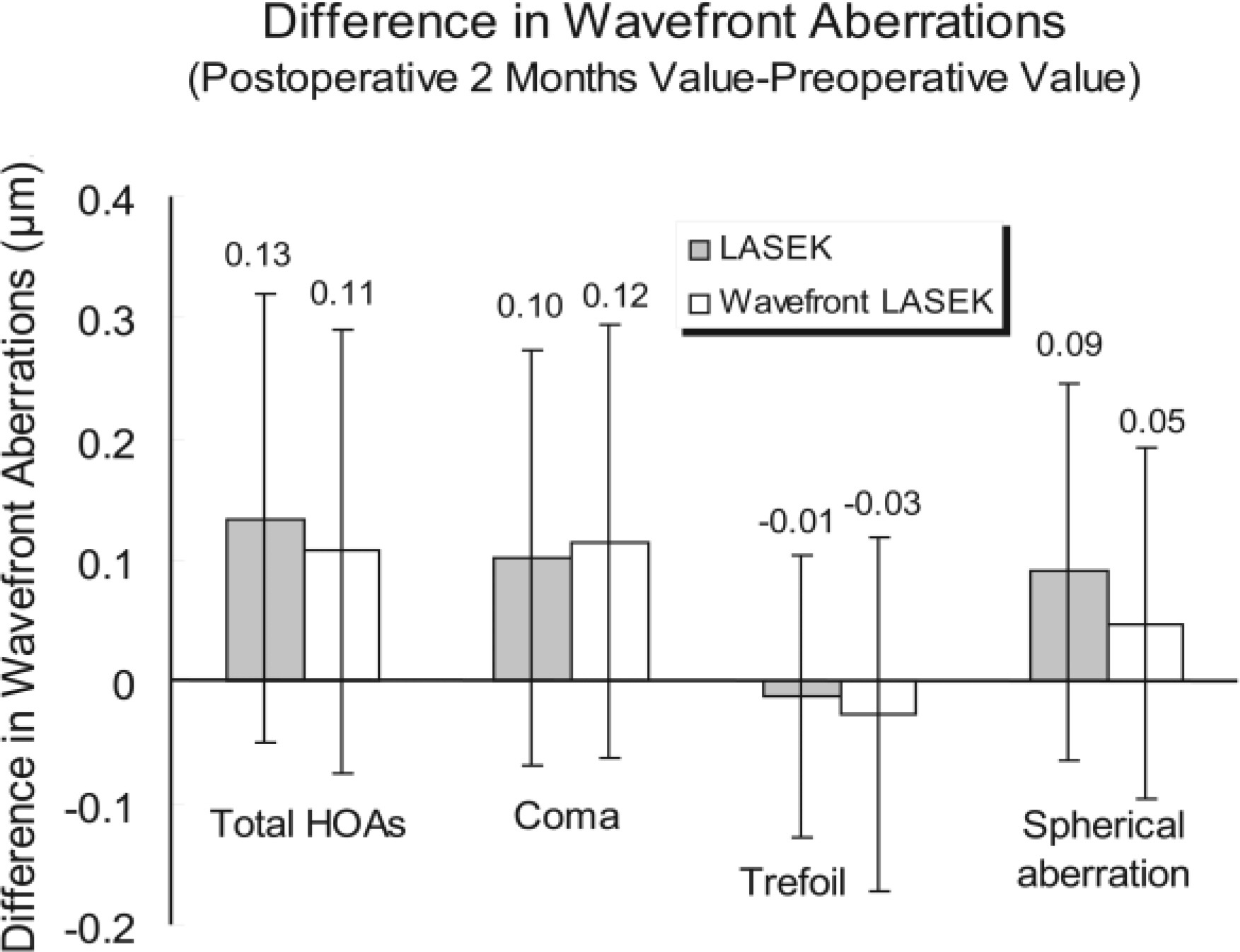
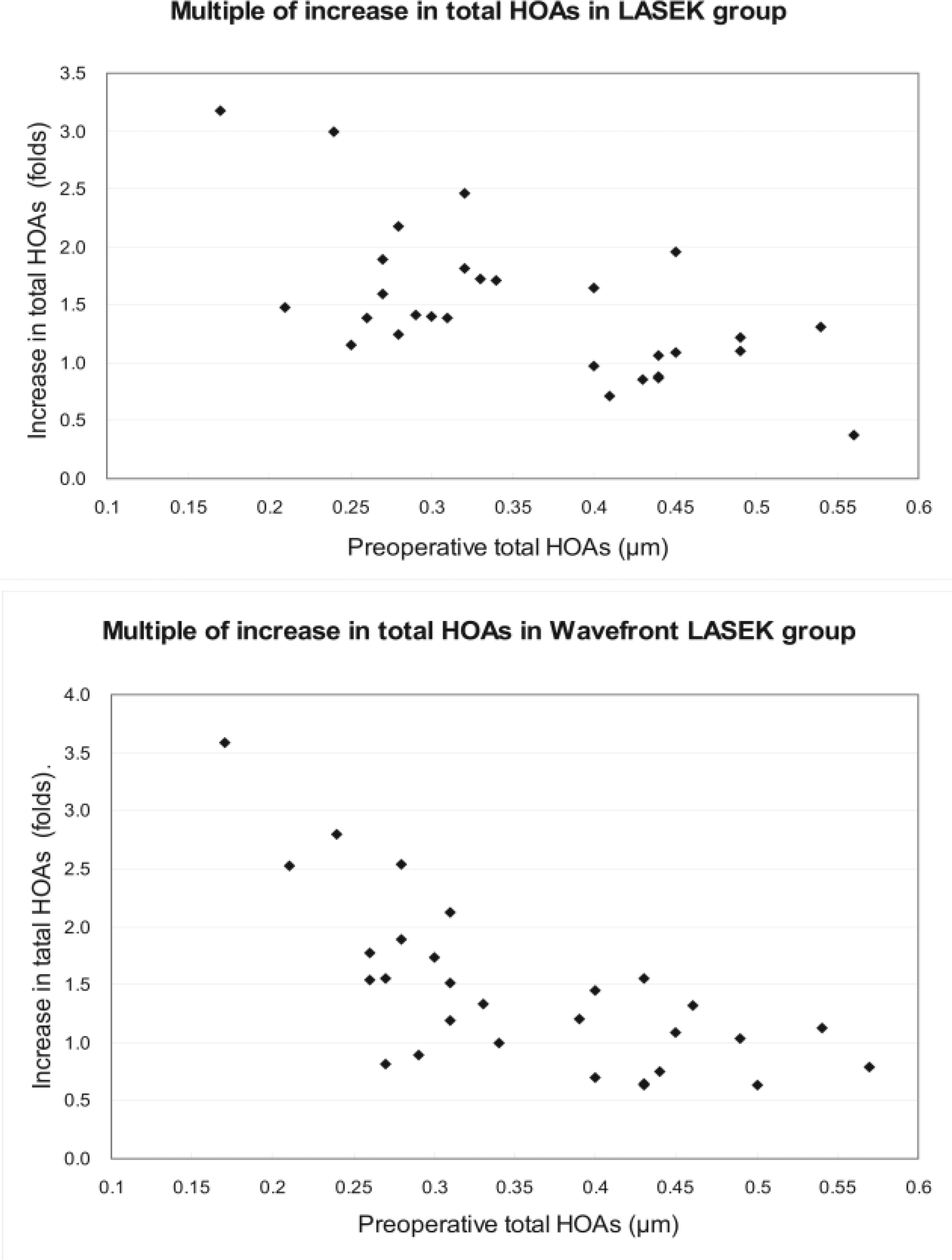
Postoperative total HOAs, comas, and spherical aberrations increased significantly from 0.36+/-0.10 micrometer to 0.49+/-0.16 micrometer (p=.001), 0.21+/-0.09 micrometer to 0.31+/-0.14 micrometer (p=.003), and 0.03+/-0.10 micrometer to 0.10+/-0.20 micrometer (p=.043), respectively, in the conventional LASEK group. In the wavefront LASEK group, postoperative HOAs, comas, and spherical aberrations significantly increased from 0.36+/-0.10 micrometer to 0.46+/-0.14 micrometer (p=.004), 0.18+/-0.10 micrometer to 0.29+/-0.14 micrometer (p=.002), and 0.09+/-0.14 micrometer to 0.19+/-0.14 micrometer (p=.006), respectively. There were no significant differences in HOAs between the two groups. A strong negative correlation between preoperative total HOAs and a multiple of increase in total HOAs postoperatively was found, with the negative correlation being stronger in the wavefront-guided LASEK group (Pearson's correlation coefficient =-0.697, p<.001) than in the LASEK group (Pearson's correlation coefficient =-0.632, p<.001).
CONCLUSIONS
There were no significant decreases in HOAs in the eyes that underwent wavefront-guided LASEK compared with the matched control eyes of patients that underwent conventional LASEK. Analyzing the tendency of a multiple of increase in total HOAs according to the preoperative HOAs, it suggests that the wavefront-guided LASEK may be more effective in suppressing an increase in total HOAs in the eyes with higher preoperative HOAs.
Figure
Reference
-
References
1. Taneri S, Zieske JD, Azar DT. Evolution, techniques, clinical outcomes, and pathophysiology of LASEK: review of the literature. Surv Ophthalmol. 2004; 49:576–602.
Article2. Netto MV, Dupps W Jr, Wilson SE. Wavefront-guided ablation: evidence for efficacy compared to traditional ablation. Am J Ophthalmol. 2006; 141:360–8.
Article3. Thibos LN. Principles of Hartmann-Shack aberrometry. J Refract Surg. 2000; 16:S563–5.
Article4. Liang J, Grimm B, Goelz S, Bille J. Objective measurement of wave aberrations of the human eye with the use a Hartmann Shack wavefront sensor. J Opt Soc Am A Opt Image Sci Vis. 1994; 11:1949–57.5. McDonald MB. Summit-Autonomous Custom Cornea laser in situ keratomileusis outcomes. J Refract Surg. 2000; 16:S617–8.
Article6. Panagopoulou SI, Pallikaris IG. Wavefront customized ablations with the WASCA Asclepion workstation. J Refract Surg. 2001; 17:S608–12.
Article7. Kanjani N, Jacob S, Agarwal S, et al. Wavefront- and topography-guided ablation in myopic eyes using Zyoptix. J Cataract Refract Surg. 2004; 30:398–402.
Article8. Oh JR, Kim JS, Lee DH. The change of ocular aberration after LASIK Surgery. J Korean Ophthalmol Soc. 2003; 44:278–83.9. Chalita MR, Chavala S, Xu M, Krueger RR. Wavefront analysis in post-LASIK eyes and its correlation with visual symptoms, refraction, and topography. Ophthalmology. 2004; 111:447–53.
Article10. Yamane N, Miyata K, Samejima T, et al. Ocular higher-order aberrations and contrast sensitivity after conventional laser in situ keratomileusis. Invest Ophthalmol Vis Sci. 2004; 45:3986–90.
Article11. Seiler T, Kaemmerer M, Mierdel P, Krinke HE. Ocular optical aberrations after photorefractive keratectomy for myopia and myopic astigmatism. Arch Ophthalmol. 2000; 118:17–21.
Article12. Kim TW, Wee WR, Lee JH, Kim MK. The changes of contrast sensitivity and glare in laser keratomileusis and laser epithelial keratomileusis with VISX S4. J Cataract Refract Surg. 2007; 23:355–61.13. Lee SW, Choi TH, Lee HB. Comparison of wavefront guided ablation vs. conventional ablation. J Korean Ophthalmol Soc. 2003; 44:2607–14.14. Kim TI, Yang SJ, Tchah H. Bilateral comparison of wavefront-guided versus conventional laser in situ keratomileusis with Bausch and Lomb Zyoptix. J Refract Surg. 2004; 20:432–8.
Article15. Cho SH, Kim HJ, Kim MJ, Joo CK. Clinical outcomes of wavefront-guided LASIK: 6-months follow-up. J Korean Ophthalmol Soc. 2005; 46:610–5.16. Lee YH, Kim GH, Roh GH. Comparison of conventional versus wavefront-guided LASIK. J Korean Ophthalmol Soc. 2005; 46:2050–8.17. Kim MJ, Kim HJ, Joo CK. Clinical outcomes of wavefront-guided LASIK using the Fourier algorithm: 6-months follow-up. J Korean Ophthalmol Soc. 2006; 47:806–11.18. Kim YT, Chung ES. Clinical result of wavefront-guided corneal ablation: LASIK vs. LASEK. J Korean Ophthalmol Soc. 2005; 46:1114–20.19. Chung SH, Lee IS, Lee YG, et al. Comparison of higher-order aberrations after wavefront-guided laser in situ keratomileusis and laser-assisted subepithelial keratectomy. J Cataract Refract Surg. 2006; 32:779–84.
Article20. Buzzonetti L, Iarossi G, Valente P, et al. Comparison of wavefront aberration changes in the anterior corneal surface after laser-assisted subepithelial keratectomy and laser in situ keratomileusis: preliminary study. J Cataract Refract Surg. 2004; 30:1929–33.
Article21. Seo KY, Lee JB, Kang JJ, et al. Comparison of higher-order aberrations after LASEK with a 6.0 mm ablation zone and a 6.5 mm ablation zone with blend zone. J Cataract Refract Surg. 2004; 30:653–7.
Article22. Lee SB, Choi BH. Analysis of higher-order wavefront aberrations in standard PRK. J Korean Ophthalmol Soc. 2005; 46:1454–63.23. Oh SJ, Lee IS, Lee YG, et al. Comparison of higher-order aberrations (HOAs) between wavefront-guided laser in situ keratomileusis and laser epithelial keratomileusis. J Korean Ophthalmol Soc. 2004; 45:1652–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Higher-order Aberrations (HOAs) between Wavefront-guided Laser in Situ Keratomileusis and Laser Epithelial Keratomileusis
- The Changes of Posterior Corneal Surface and High-Order Aberrations after Refractive Surgery in Moderate Myopia
- Change of High-order Aberration after Wavefront-guided LASIK and LASEK
- Clinical Result of Wavefront-guided Corneal Ablation: LASIK vs. LASEK
- Higher-Order Aberrations and Visual Acuity with Wavefront-Guided and Wavefront-Optimized Ablation in Laser Keratorefractive Surgery