J Korean Rheum Assoc.
2010 Sep;17(3):289-294.
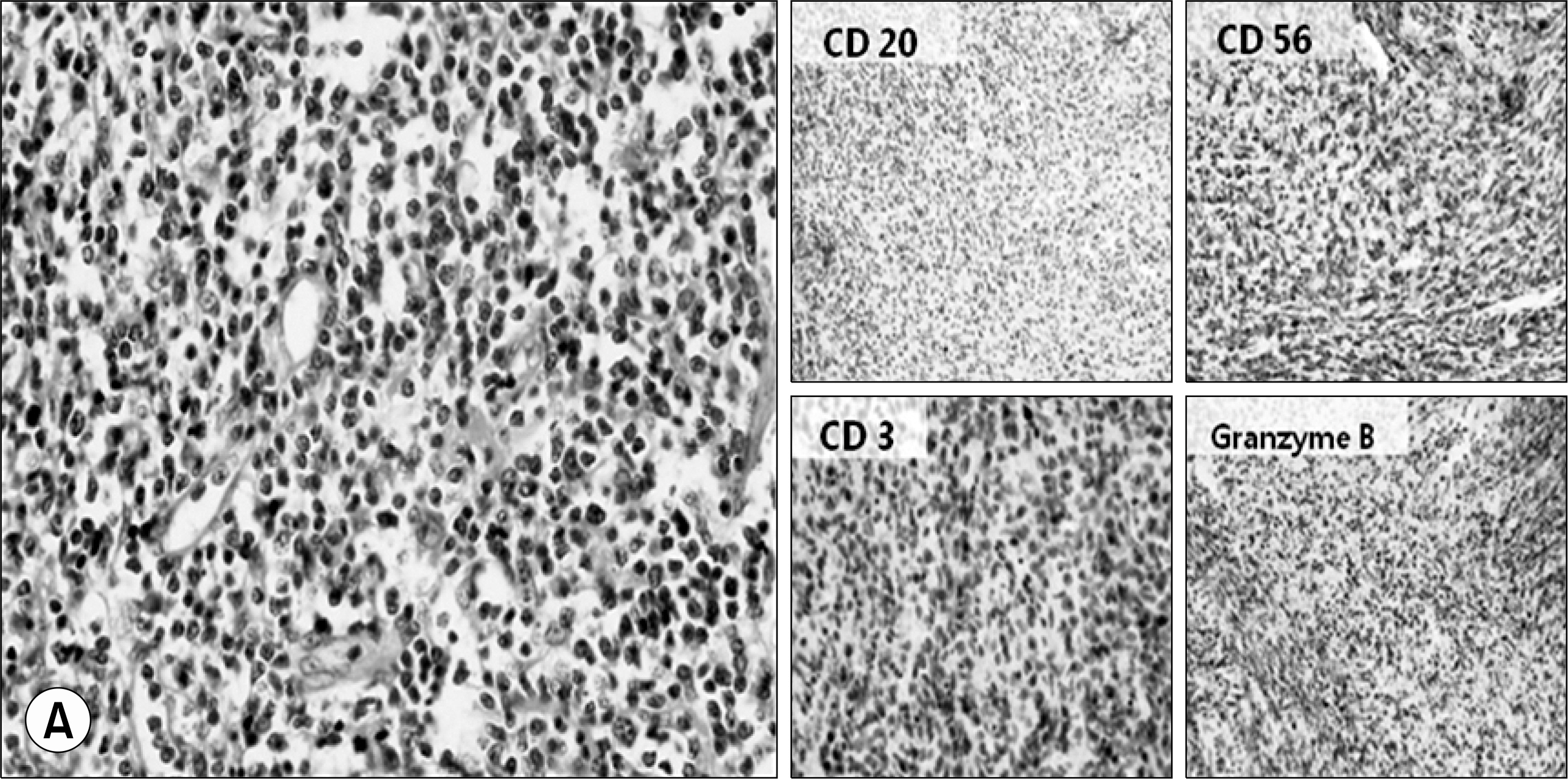
A Case of NK/T Cell Lymphoma Mimicking Limited Form of Wegener's Granulomatosis
- Affiliations
-
- 1Division of Rheumatology, Department of Internal Medicine, The Catholic University of Korea, Seoul, Korea. chocs@catholic.ac.kr
Abstract
- It is occasionally difficult to distinguish Wegener's granulomatosis (WG) from other diseases including malignancy, tuberculosis, and various types of vasculitis because of the overlapping symptoms and signs. We report on a patient with NK/T cell lymphoma who was treated with a limited form of WG. At his first visit, he presented with left foot drop and recurrent nasal swelling. Necrosis and massive infiltration of inflammatory cells were identified on a nasal tissue biopsy. Sural nerve biopsy findings also showed infiltration of inflammatory cells in both the endoneurium and perivascular area; thus, a diagnosis of a limited form of WG was made. After combination therapy with a glucocorticoid and oral cyclophosphamide was initiated, his condition completely recovered without recurrence for the next 2 years. However, he visited the hospital again for recurrence of nasal swelling. Repeated biopsy of nasal tissues, combined with an immunophenotypic analysis revealed NK/T cell lymphoma. The possibility of NK/T lymphoma should be considered when evaluating a limited type of WG, which shows atypical findings on biopsy as well as recurrent deterioration, as a suboptimal dose of immunosuppressive therapy may mask its expression and lead to a poor prognosis.
MeSH Terms
Figure
Reference
-
1). Thajeb P., Tsai JJ. Cerebral and oculorhinal manifestations of a limited form of Wegener's granulomatosis with c-ANCA-associated vasculitis. J Neuroimaging. 2001. 11:59–63.
Article2). Cassan SM., Coles DT., Harrison EG Jr. The concept of limited forms of Wegener's granulomatosis. Am J Med. 1970. 49:366–79.
Article3). Hoffman GS., Kerr GS., Leavitt RY., Hallahan CW., Lebovics RS., Travis WD, et al. Wegener granulomatosis: an analysis of 158 patients. Ann Intern Med. 1992. 116:488–98.
Article4). Knight A., Askling J., Ekbom A. Cancer incidence in a population-based cohort of patients with Wegener's granulomatosis. Int J Cancer. 2002. 100:82–5.
Article5). Fain O., Hamidou M., Cacoub P., Godeau B., Wechsler B., Paries J, et al. Vasculitides associated with malignancies: analysis of sixty patients. Arthritis Rheum. 2007. 57:1473–80.
Article6). Manske CL., Glick AD., Stone WJ. Sinusitis and glomerulonephritis in a middle-aged man. Am J Kidney Dis. 1987. 10:320–2.
Article7). Borress RS., Maccabee P., Har-El G. Foot drop in head and neck cancer. Am J Otolaryngol. 2007. 28:321–4.
Article8). VaAroAczy L., Gergely L., Zeher M., Szegedi G., IlleAs A. Malignant lymphoma-associated autoimmune diseases- a descriptive epidemiological study. Rheumatol Int. 2002. 22:233–7.9). Bobba RK., Arsura EL., Sawh AK., Naseem M. Diagnostic challenge posed by the clinical presentation of foot drop in a patient with Hodgkin's lymphoma. Eur J Intern Med. 2006. 17:572–4.
Article10). Cohen Y., Amir G., Schibi G., Amariglio N., Polliack A. Rapidly progressive diffuse large B-cell lymphoma with initial clinical presentation mimicking seronegative Wegener's granulomatosis. Eur J Haematol. 2004. 73:134–8.
Article