J Korean Assoc Oral Maxillofac Surg.
2014 Jun;40(3):140-146.
Pigmented villonodular synovitis of the temporomandibular joint - computed tomography and magnetic resonance findings: a case report
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Inha University College of Medicine, Incheon, Korea. kik@inha.ac.kr
Abstract
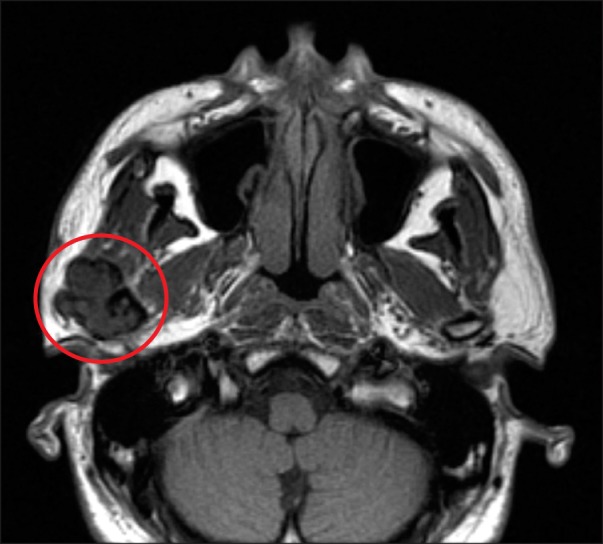
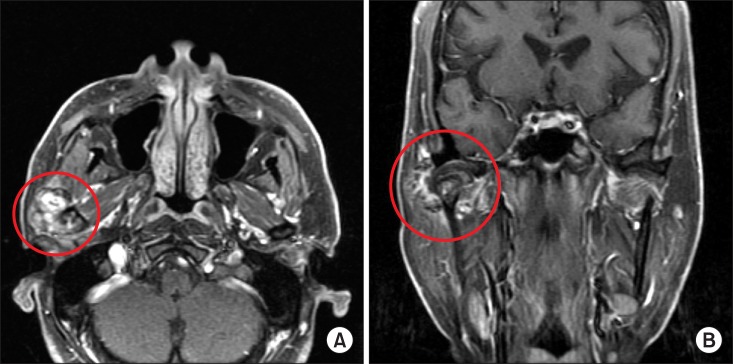
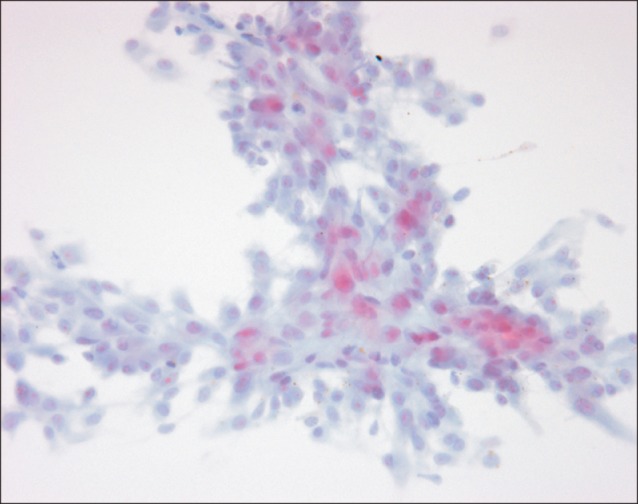
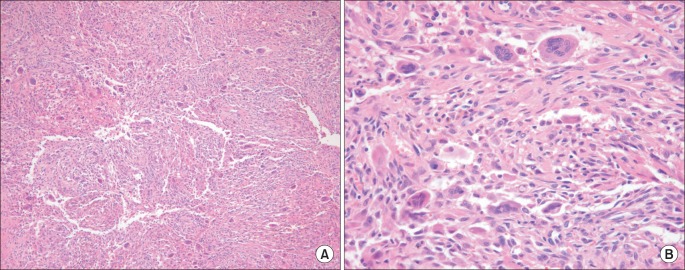
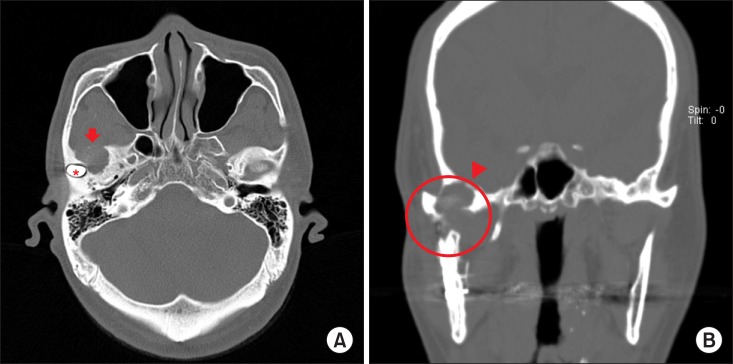
- Pigmented villonodular synovitis (PVNS) is a benign but locally aggressive and destructive disease originating in the synovial membranes. It is a proliferative disorder of unknown etiology. Involvement of the temporomandibular joint (TMJ) is very rare. Computed tomography clearly reveals areas of lytic bone erosion and sclerosis, and also clearly defines the extent of the tumor which is the focal areas of hyperdensity within the soft-tissue mass. Magnetic resonance images invariably show profound hypointensity on both T1- and T2-weighted sequences due to hemosiderin pigmentation. Additionally, high signal intensity on T2-weighted images may indicate cystic loculation of the joint fluid. This case study describes a rare case of PVNS of the TMJ with bone destruction of the mandibular condyle. Complete surgical excision of the lesion was performed through a preauricular approach with temporal extension. During the 10-year follow-up, two more operations were performed due to local recurrence and the fracture of the reconstruction plate. Total joint reconstruction with Biomet was finally performed, and the absence of disease was confirmed with a biopsy report showing fibrosis with hyalinization and mild inflammation of the excised soft tissue from the old lesion.
MeSH Terms
Figure
Reference
-
1. Jaffe HL, Lichtenstein L, Sutro CJ. Pigmented villonodular synovitis, bursitis and tenosynovitis. Arch Pathol. 1941; 31:731–765.2. Kim KW, Han MH, Park SW, Kim SH, Lee HJ, Jae HJ, et al. Pigmented villonodular synovitis of the temporomandibular joint: MR findings in four cases. Eur J Radiol. 2004; 49:229–234. PMID: 14962652.
Article3. Aoyama S, Iwaki H, Amagasa T, Kino K, Okada N, Kishimoto S. Pigmented villonodular synovitis of the temporomandibular joint: differential diagnosis and case report. Br J Oral Maxillofac Surg. 2004; 42:51–54. PMID: 14706302.
Article4. Kişnişci RS, Tüz HH, Günhan O, Onder E. Villonodular synovitis of the temporomandibular joint: case report. J Oral Maxillofac Surg. 2001; 59:1482–1484. PMID: 11732040.
Article5. Lapayowker MS, Miller WT, Levy WM, Harwick RD. Pigmented villonodular synovitis of the temperomandibular joint. Radiology. 1973; 108:313–316. PMID: 4719033.
Article6. Liu YK, Chan JY, Chang CJ, Huang JS. Pigmented villonodular synovitis of the temporomandibular joint presenting as a middle cranial fossa tumor. J Oral Maxillofac Surg. 2012; 70:367–372. PMID: 21741744.
Article7. Bemporad JA, Chaloupka JC, Putman CM, Roth TC, Tarro J, Mitra S, et al. Pigmented villonodular synovitis of the temporomandibular joint: diagnostic imaging and endovascular therapeutic embolization of a rare head and neck tumor. AJNR Am J Neuroradiol. 1999; 20:159–162. PMID: 9974074.8. Cai J, Cai Z, Gao Y. Pigmented villonodular synovitis of the temporomandibular joint: a case report and the literature review. Int J Oral Maxillofac Surg. 2011; 40:1314–1322. PMID: 21474285.
Article9. Cascone P, Rinna C, Ungari C, Poladas G, Filiaci F. Pigmented villonodular synovitis of the temporomandibular joint. J Craniofac Surg. 2005; 16:712–716. PMID: 16077324.
Article10. Safaee M, Oh T, Sun MZ, Parsa AT, McDermott MW, El-Sayed IH, et al. Pigmented villonodular synovitis of the temporomandibular joint with intracranial extension: a case series and systematic review. Head Neck. 2014; doi: 10.1002/hed.23717.
Article11. Church CA, Rowe M, Llaurado R, Liwnicz BH, Martin PA. Pigmented villonodular synovitis of the temporomandibular joint: a report of two cases. Ear Nose Throat J. 2003; 82:692–695. PMID: 14569704.
Article12. Le WJ, Li MH, Yu Q, Shi HM. Pigmented villonodular synovitis of the temporomandibular joint: CT imaging findings. Clin Imaging. 2014; 38:6–10. PMID: 24100118.
Article13. Stryjakowska KK, Martel M, Sasaki CT. Pigmented villonodular synovitis of the temporomandibular joint: differential diagnosis of the parotid mass. Auris Nasus Larynx. 2005; 32:309–314. PMID: 15941640.
Article14. Wong JJ, Phal PM, Wiesenfeld D. Pigmented villonodular synovitis of the temporomandibular joint: a radiologic diagnosis and case report. J Oral Maxillofac Surg. 2012; 70:126–134. PMID: 21783297.
Article15. O'Sullivan TJ, Alport EC, Whiston HG. Pigmented villonodular synovitis of the temporomandibular joint. J Otolaryngol. 1984; 13:123–126. PMID: 6726846.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Villonodular Synovitis of the Temporomandibular Joint: A Case Report
- A Case of Pedunculated Localized Nodular Synovitis of the Knee: MR Imaging Findings
- Nodular Pigmented Villonodular Synovitis of the Right Shoulder Joint: One Case Report
- Localized Pigmented Villonodular Synovitis with Recurrent Subluxation of the Patella: A Case Report
- Localized Pigmented Villonodular Synovitis of the Posterior Compartment of the Knee: A Case Report