Pediatr Gastroenterol Hepatol Nutr.
2016 Jun;19(2):104-109. 10.5223/pghn.2016.19.2.104.
Efficacy and Tolerance of a New Anti-Regurgitation Formula
- Affiliations
-
- 1Department of Paediatric Gastroenterology Hepatology and Nutrition, Hôpital Necker Enfants Malades, Paris, France.
- 2Department of Paediatrics, UZ Brussel, Vrije Universiteit Brussel, Brussels, Belgium. yvan.vandenplas@uzbrussel.be
- KMID: 2328170
- DOI: http://doi.org/10.5223/pghn.2016.19.2.104
Abstract
- PURPOSE
Regurgitation is a common physiological phenomenon in infants. The aim of the present study was to evaluate the efficacy of a new anti-regurgitation (AR) formula (Novalac), thickened with an innovative complex including fibres, on the daily number of regurgitations and to assess its impact on stool consistency and frequency.
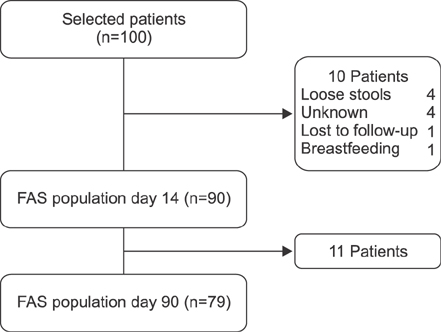
METHODS
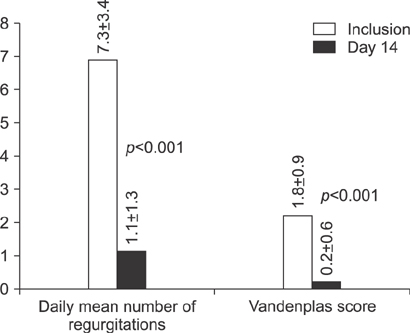
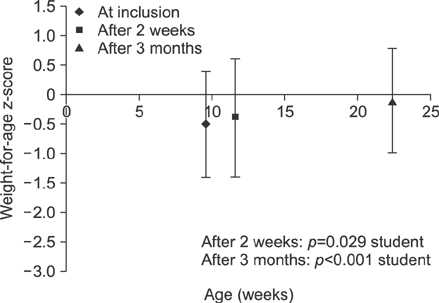
Infants younger than five months, presenting at least 5 regurgitations per day were recruited in this trial. The efficacy of the new formula on regurgitation (daily number and Vandenplas score), stool frequency and consistency were assessed at day 14 and 90. Growth data were recorded at each study visit.
RESULTS
Ninety babies (mean age 9.6±5.8 weeks) were included in the full analysis data set. The mean number of regurgitation episodes at inclusion was 7.3±3.4. In all infants, regurgitations improved after 2 weeks. The daily number of regurgitations decreased significantly (-6.3±3.3, p<0.001) including in those previously fed a thickened formula (-6.2±3.0, p<0.001). There was no significant change in stool consistency at day 14. After 3 months, 97.5% of infants had formed or soft stools. Growth was appropriate with a slight increase of weight-for-age z-score (from -0.5±1.0 to -0.1±0.9) and no change of weight-for length z-score (-0.1±1.1 to -0.1±-1.1).
CONCLUSION
The new AR formula thickened with an innovative complex is very effective in reducing the daily number of regurgitations without having a negative impact on stools consistency.
Keyword
Figure
Reference
-
1. Vandenplas Y, Rudolph CD, Di Lorenzo C, Hassall E, Liptak G, Mazur L, et al. Pediatric gastroesophageal reflux clinical practice guidelines: joint recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN). J Pediatr Gastroenterol Nutr. 2009; 49:498–547.
Article2. Martin AJ, Pratt N, Kennedy JD, Ryan P, Ruffin RE, Miles H, et al. Natural history and familial relationships of infant spilling to 9 years of age. Pediatrics. 2002; 109:1061–1067.
Article3. Nelson SP, Chen EH, Syniar GM, Christoffel KK. Prevalence of symptoms of gastroesophageal reflux during infancy. A pediatric practice-based survey. Pediatric Practice Research Group. Arch Pediatr Adolesc Med. 1997; 151:569–572.
Article4. Vandenplas Y, Abkari A, Bellaiche M, Benninga M, Chouraqui JP, Çokura F, et al. Prevalence and health outcomes of functional gastrointestinal symptoms in infants from birth to 12 months of age. J Pediatr Gastroenterol Nutr. 2015; 61:531–537.
Article5. Vandenplas Y, Lifshitz JZ, Orenstein S, Lifschitz CH, Shepherd RW, Casaubón PR, et al. Nutritional management of regurgitation in infants. J Am Coll Nutr. 1998; 17:308–316.
Article6. Vandenplas Y, Gutierrez-Castrellon P, Velasco-Benitez C, Palacios J, Jaen D, Ribeiro H, et al. Practical algorithms for managing common gastrointestinal symptoms in infants. Nutrition. 2013; 29:184–194.
Article7. Wenzl TG, Schneider S, Scheele F, Silny J, Heimann G, Skopnik H. Effects of thickened feeding on gastroesophageal reflux in infants: a placebo-controlled crossover study using intraluminal impedance. Pediatrics. 2003; 111:e355–e359.
Article8. Vandenplas Y, Hachimi-Idrissi S, Casteels A, Mahler T, Loeb H. A clinical trial with an "anti-regurgitation" formula. Eur J Pediatr. 1994; 153:419–423.
Article9. Iacono G, Vetrano S, Cataldo F, Ziino O, Russo A, Lorello D, et al. Clinical trial with thickened feeding for treatment of regurgitation in infants. Dig Liver Dis. 2002; 34:532–533.
Article10. Lewis SJ, Heaton KW. Stool form scale as a useful guide to intestinal transit time. Scand J Gastroenterol. 1997; 32:920–924.
Article11. World Health Organization. WHO Multicentre Growth Reference Study Group: WHO Child Growth Standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development. Geneva: World Health Organization;2006. Available from: http://www.who.int/childgrowth/standards/en/.12. Horvath A, Dziechciarz P, Szajewska H. The effect of thickened-feed interventions on gastroesophageal reflux in infants: systematic review and meta-analysis of randomized, controlled trials. Pediatrics. 2008; 122:e1268–e1277.
Article13. Vandenplas Y, De Greef E, Hauser B. Paradice Study Group. Safety and tolerance of a new extensively hydrolyzed rice protein-based formula in the management of infants with cow's milk protein allergy. Eur J Pediatr. 2014; 173:1209–1216.
Article14. Dupont C, Kalach N, Soulaines P, Bradatan E, Lachaux A, Payot F, et al. Safety of a new amino acid formula in infants allergic to cow's milk and intolerant to hydrolysates. J Pediatr Gastroenterol Nutr. 2015; 61:456–463.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Digestive Tolerance and Safety of an Anti-Regurgitation Formula Containing Locust Bean Gum, Prebiotics and Postbiotics: A RealWorld Study
- Effectiveness and Tolerance of a Locust Bean Gum-Thickened Formula: A Real-Life Study
- Types of Special Infant Formulas Marketed in Korea and Their Indications
- Middle East Consensus Statement on the Diagnosis and Management of Functional Gastrointestinal Disorders in <12 Months Old Infants
- Safety of a New Synbiotic Starter Formula