J Korean Soc Spine Surg.
2016 Jun;23(2):108-113. 10.4184/jkss.2016.23.2.108.
Late Pyogenic Spondylitis after Vertebroplasty with PMMA-filled Adjacent Segments: A Case Report
- Affiliations
-
- 1Department of Orthopaedic Surgery, Chungbuk National University, Cheongju, Korea. ymkim@chungbuk.ac.kr
- KMID: 2328004
- DOI: http://doi.org/10.4184/jkss.2016.23.2.108
Abstract
OBJECTIVES
To report a rare case of late pyogenic spondylitis around the cement mass in T12 that developed 4 years after vertebroplasty with L1-3 bodies already filled with cement due to previous vertebroplasty. SUMMARY OF LITERATURE REVIEW: Pyogenic spondylitis after vertebroplasty is a rare complication, but very difficult to manage.
MATERIALS AND METHODS
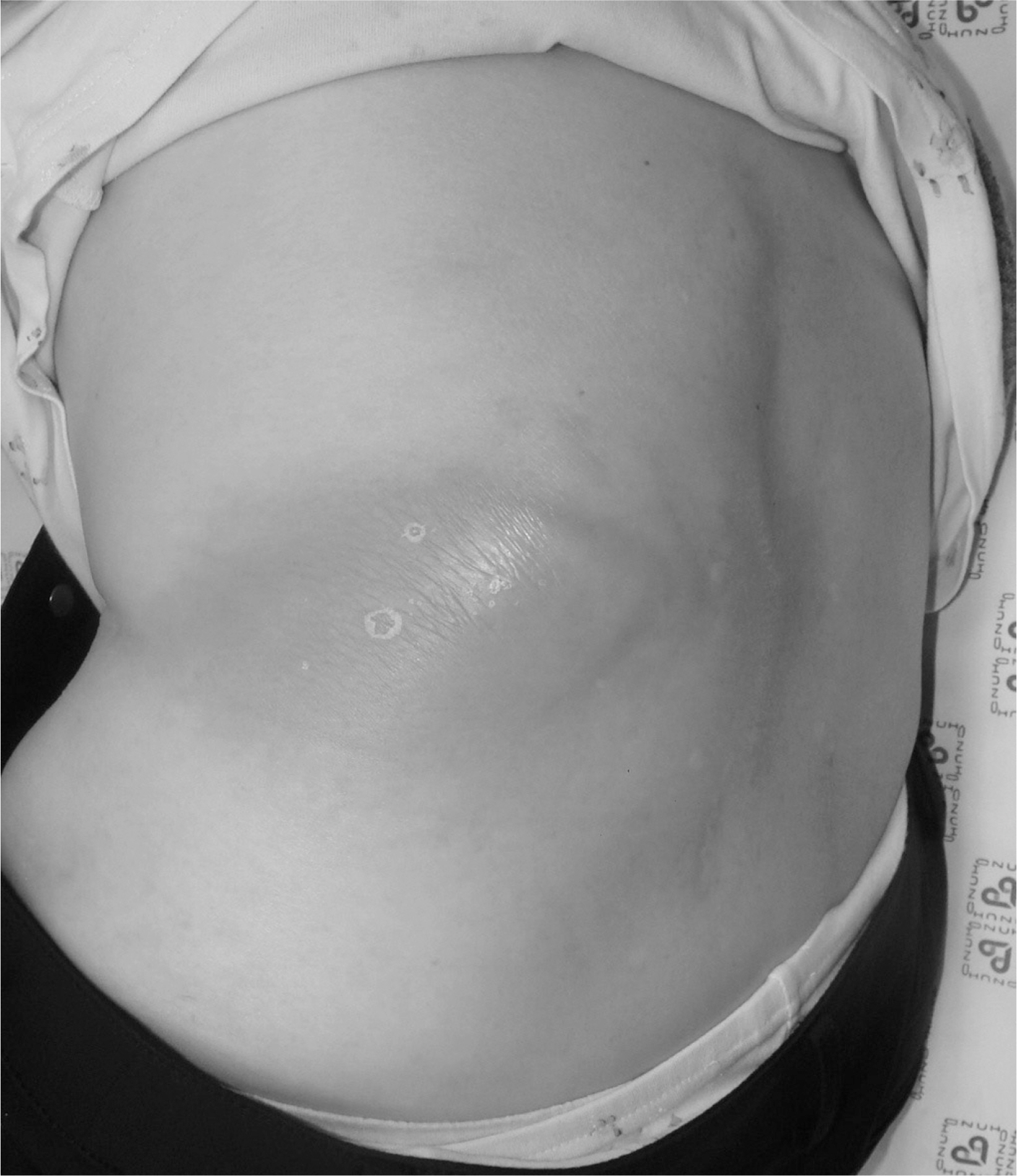
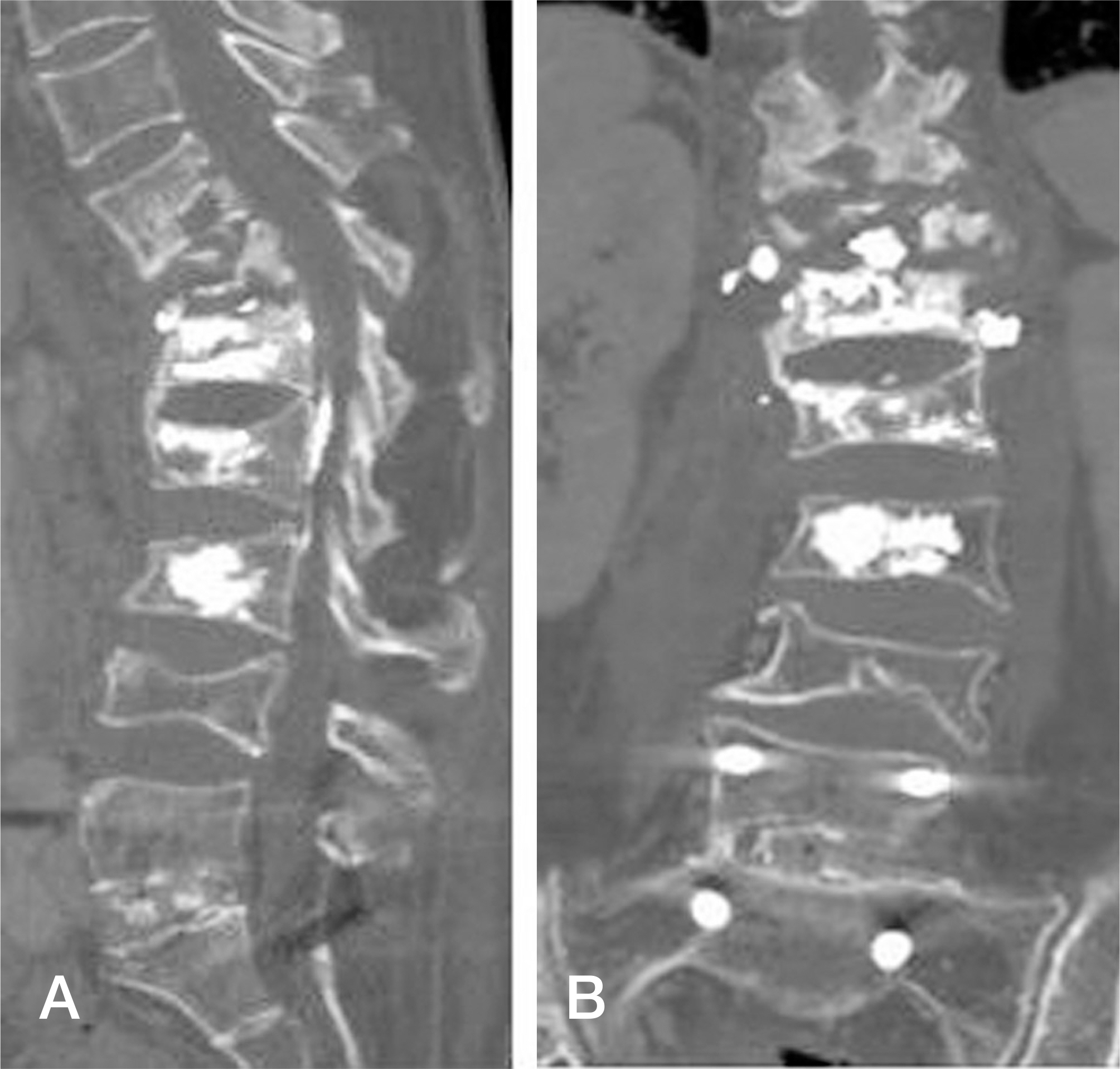
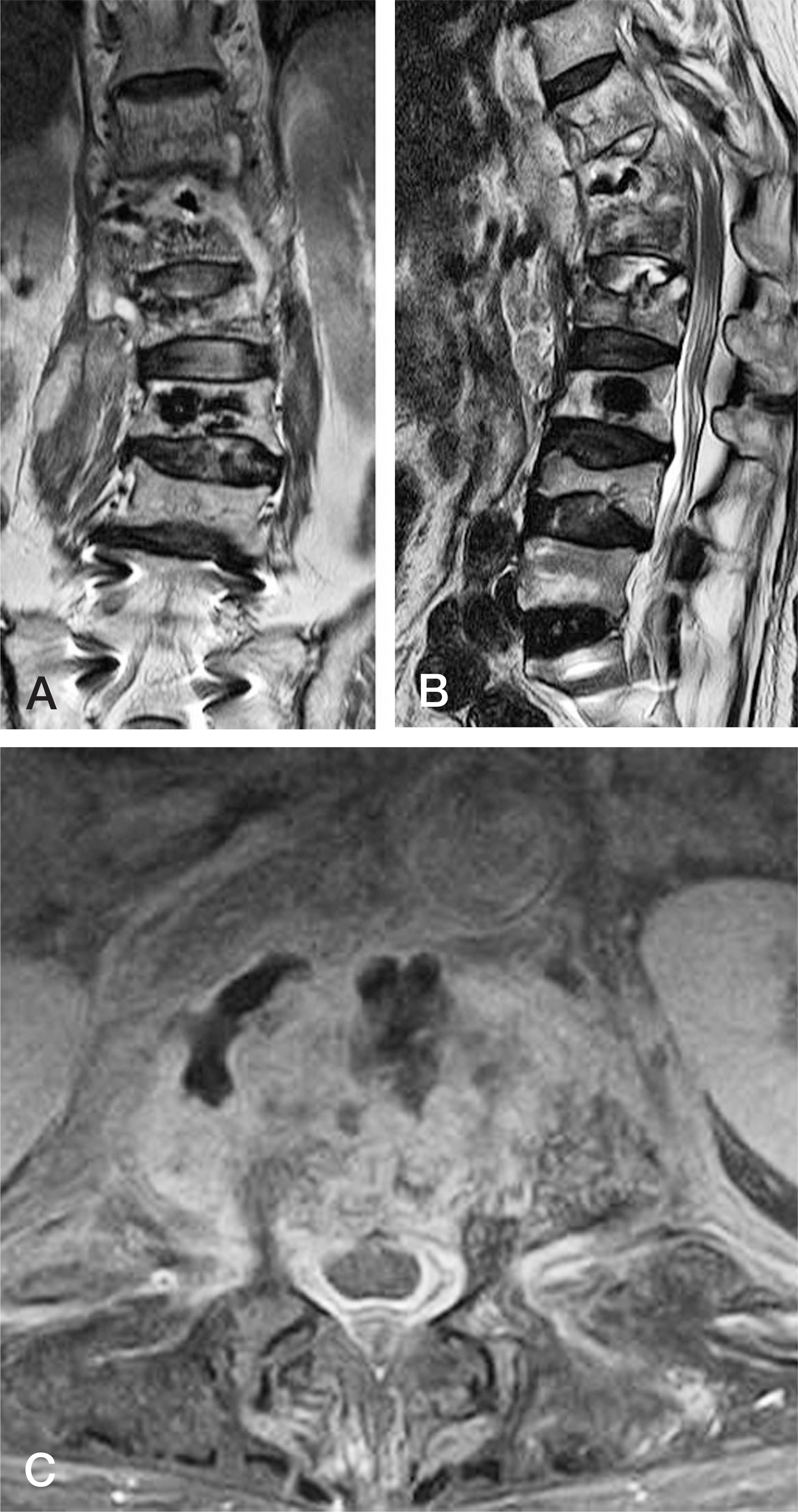
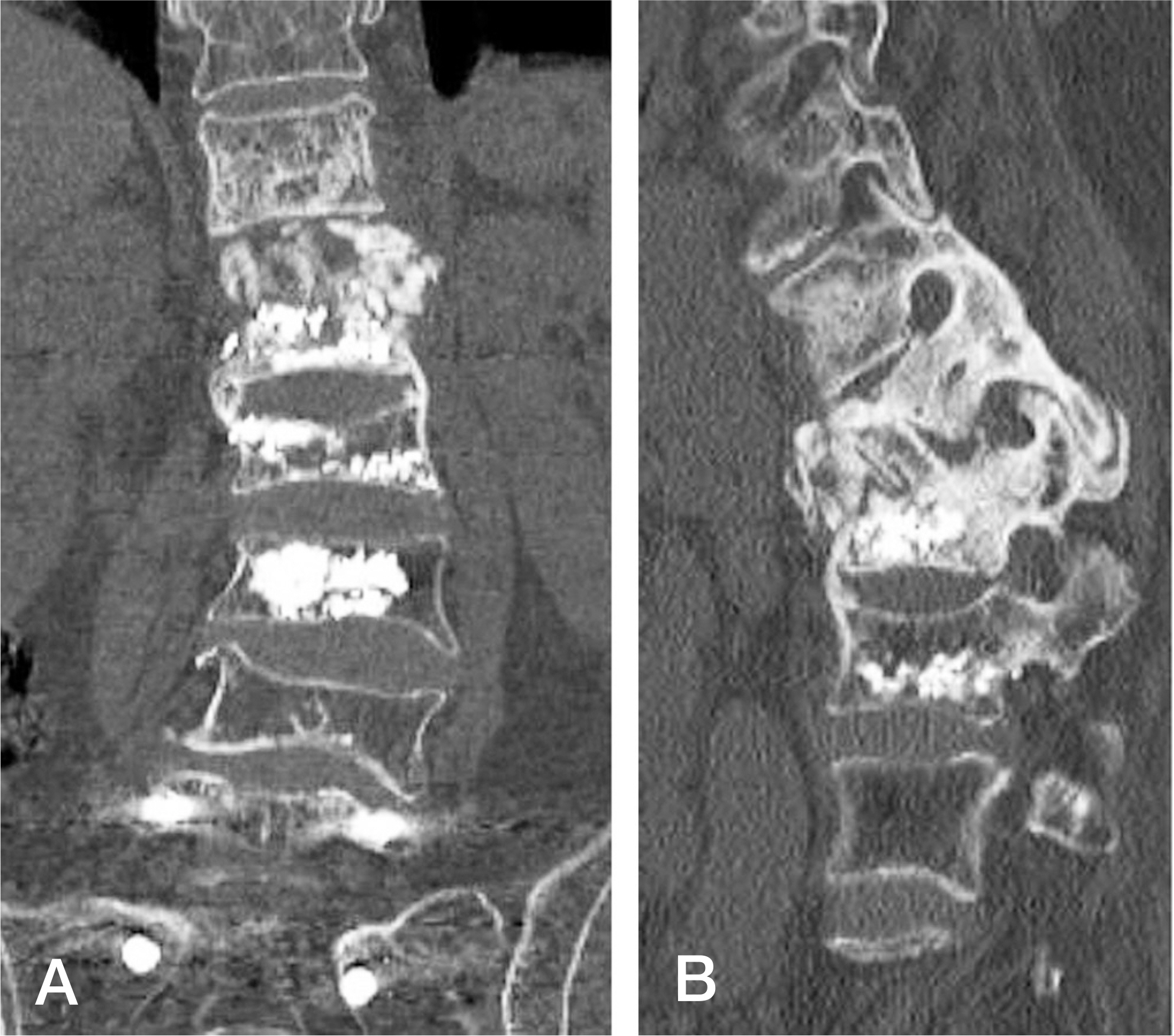
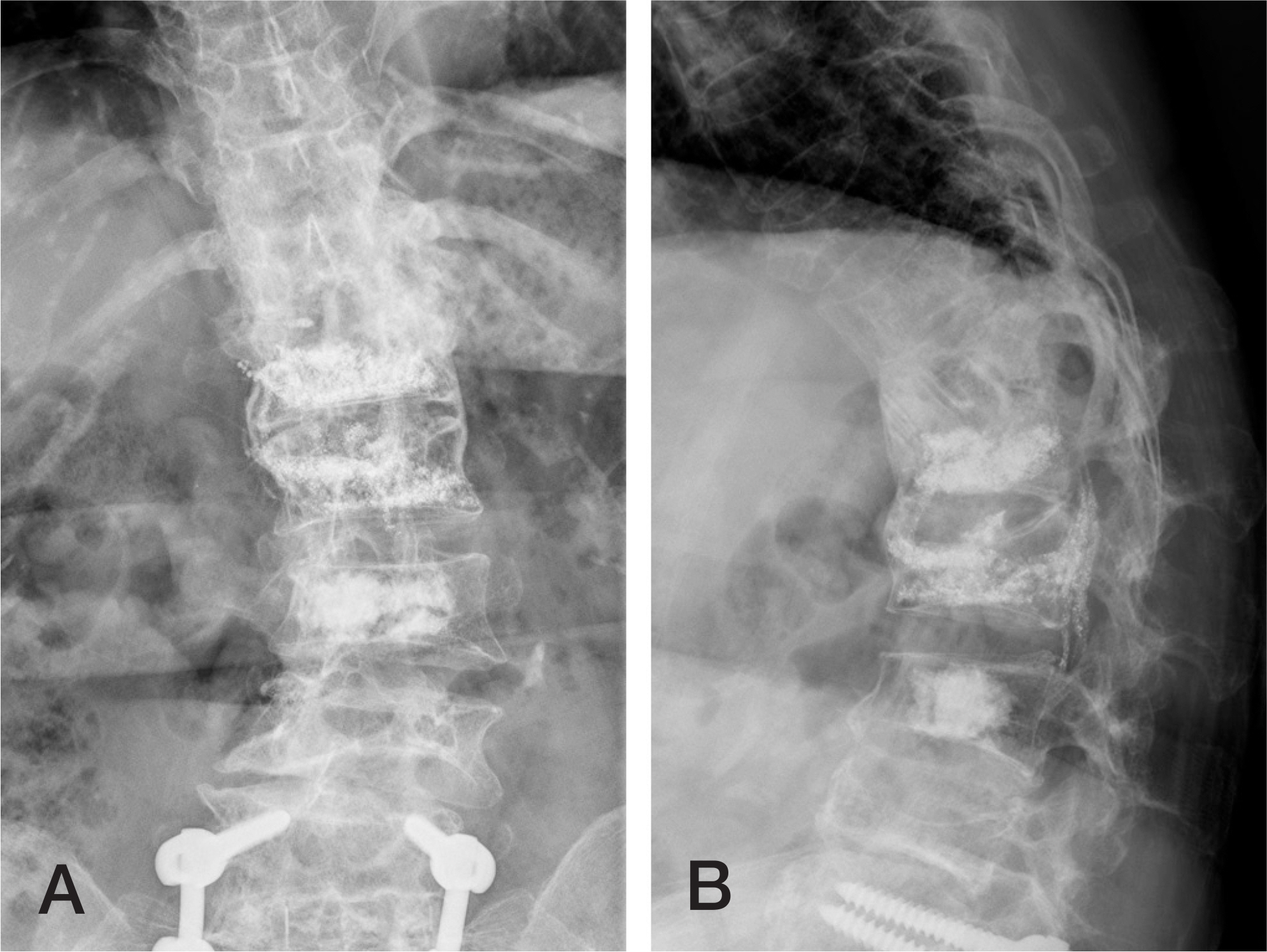
A 56-year old female visited us with pyogenic spondylitis around the T12 body. The bodies of L1-L3 had been filled with cement eight years previously, followed by another vertebroplasty for T12 four years previously in a local clinic. At first, conservative management with intravenous antibiotics was attempted for 8 weeks, without clinical improvement. Therefore, anterior surgery for T12 corpectomy, removal of the cement, and fusion was performed.
RESULTS
The infection was cured and anterior fusion was achieved, and the patient was able to return to her previous activities.
CONCLUSIONS
Though previous vertebroplasty of the adjacent vertebral body seemed to be a major obstacle to achieving fusion, anterior surgical treatment was the ultimate solution to this complex problem.
Figure
Reference
-
1. Lin W-C, Lee C-H, Chen S-H, et a�. Unusua� presentation of infected vertebrop�ast� with de�a�ed cement dis�odgment in an immunocompromised patient: Case report and review of �iterature. Cardiovasc Intervent Radio�. 2008; 31:231–5. DOI: 10.1007/s00270-007-9234-z.2. O�mos MA, Gonzá�ez AS, C�emente JD, et a�. Infected ver-tebrop�ast� due to uncommon bacteria so�ved surgica���: a rare and threatening �ife comp�ication of a common procedure: report of a case and a review of the �iterature. Spine. 2006; 31:E770–3.3. Park JS, Kim DH, Kang BJ, et a�. Spina� epidura� abscess and psoas abscess combined with p�ogenic spond��odiscitis fo��owing vertebrop�ast�: A case report. J Korean Soc Spine Surg. 2014; 21:90. DOI: 10.4184/jkss.2014.21.2.90.4. Wimmer C, G�uch H, Franzreb M, Ogon M. Predisposing factors for infection in spine surger�: A surve� of 850 spina� procedures. J Spina� Disorders. 1998; 11:124–8.5. C�ark CE, Shuff�ebarger HL. Late-deve�oping infection in instrumented idiopathic sco�iosis. Spine. 1999; 15:1909–12.6. Lee CB, Kim HS, Kim YJ. P�ogenic spond��itis after vertebrop�ast�-A report of two cases. Asian Spine J. 2007; 1:106–9.7. Shin JH, Ha KY, Lee JS, Joo MW. Surgica� treatment for de�a�ed p�ogenic spond��itis after percutaneous vertebro-p�ast� and k�phop�ast�. Report of 4 cases. J Neurosurg Spine. 2008; 9:265–72.8. Yu S-W, Chen W-J, Lin W-C, et a�. Serious p�ogenic spond��itis fo��owing vertebrop�ast�—a case report. Spine. 2004; 29:E209–11.9. Schmid KE, Boszcz�k BM, Bierschneider M, et a�. Spon-d��itis fo��owing vertebrop�ast�: a case report. Eur Spine J. 2005; 14:895–9. DOI: 10.1007/s00586-005-0905-7.10. Vats HS, McKiernan FE. Infected vertebrop�ast�: case report and review of �iterature. Spine. 2006; 31:E859–62.11. Wa�ker DH, Mummaneni P, Rodts GE Jr. Report of two cases and review of the �iterature. Neurosurg Focus. 2004; 17:E6.12. Vaudaux PE, Zu�ian G, Hugg�er E, et a�. Attachment of Staph��ococcus aureus to po��meth��methacr��ate increases its resistance to phagoc�tosis in foreign bod� infection. Infect Immun. 1985; 50:472–7.13. Kim Y-M, Won C-H, Seo J-B, et a�. P�ogenic L4-5 spond��itis managed with percutaneous drainage fo�-�owed b� posterior �umbar interbod� fusion - A case report -. J Korean Soc Spine Surg. 2001; 8:513. DOI: 10.4184/jkss.2001.8.4.513.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pyogenic Spondylitis after Vertebroplasty: A Report of Two Cases
- Streptococcus Spondylitis Concomitant Infectious Endocarditis: A Case Report
- Latent Multiple Noncontiguous Pyogenic Spondylitis: a case report
- 3 Cases of Pyogenic spondylitis
- Hypotension during Percutaneous Vertebroplasty with PMMA (Polymethylmethacrylate)