Investig Magn Reson Imaging.
2016 Jun;20(2):88-94. 10.13104/imri.2016.20.2.88.
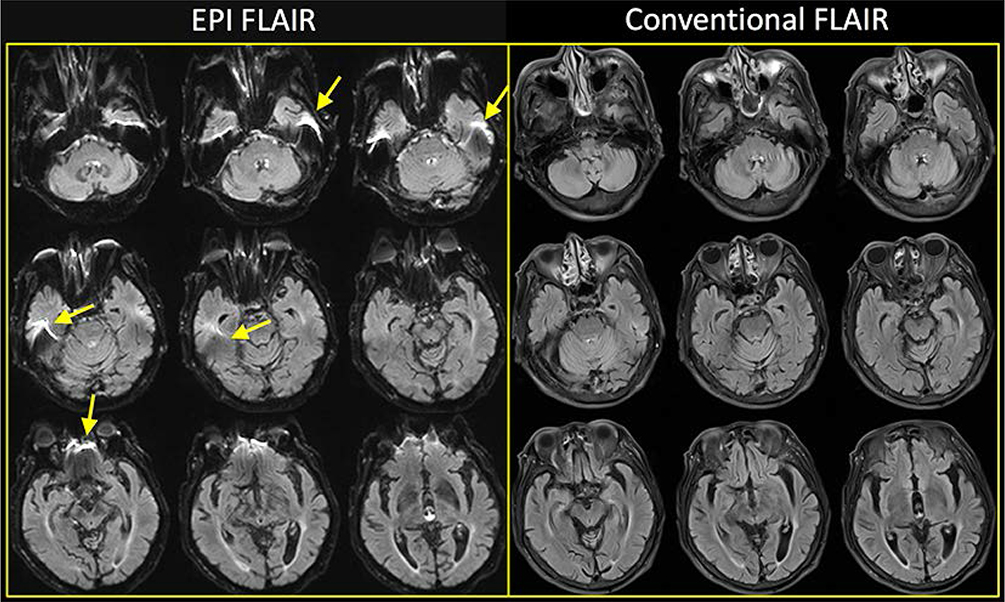
Assessment of Diffusion-Weighted Imaging-FLAIR Mismatch: Comparison between Conventional FLAIR versus Shorter-Repetition-Time FLAIR at 3T
- Affiliations
-
- 1Department of Radiology, Gachon University Gil Medical Center, Incheon, Korea. neuroradkim@gmail.com
- KMID: 2327420
- DOI: http://doi.org/10.13104/imri.2016.20.2.88
Abstract
- PURPOSE
Fluid-attenuated inversion recovery (FLAIR) imaging can be obtained faster with shorter repletion time (TR), but it gets noisier. We hypothesized that shorter-TR FLAIR obtained at 3 tesla (3T) with a 32-channel coil may be comparable to conventional FLAIR. The aim of this study was to compare the diagnostic value between conventional FLAIR (TR = 9000 ms, FLAIR9000) and shorter-TR FLAIR (TR = 6000 ms, FLAIR6000) at 3T in terms of diffusion-weighted imaging-FLAIR mismatch.
MATERIALS AND METHODS
We recruited 184 patients with acute ischemic stroke (28 patients < 4.5 hours) who had undergone 5-mm diffusion-weighted imaging (DWI) and two successive 5-mm FLAIR images (no gap; in-plane resolution, 0.9 × 0.9 mm) at 3T with a 32-channel coil. The acquisition times for FLAIR9000 and FLAIR6000 were 108 seconds (generalized autocalibrating partially parallel acquisitions [GRAPPA] = 2) and 60 seconds (GRAPPA = 3), respectively. Two radiologists independently assessed the paired imaging sets (DWI-FLAIR9000 and DWI-FLAIR6000) for the presence of matched hyperintense lesions on each FLAIR imaging. The signal intensity ratios (area of DWI lesion to contralateral normal-appearing region) on both FLAIR imaging sets were compared.
RESULTS
DWI-FLAIR9000 mismatch was present in 39 of 184 (21.2%) patients, which was perfectly the same on FLAIR6000. Three of 145 patients (2%) with DWI-matched lesions on FLAIR9000 had discrepancy on FLAIR6000, showing no significant difference (P > 0.05). Interobserver agreement was excellent for both DWI-FLAIR9000 and DWI-FLAIR6000 (k = 0.904 and 0.883, respectively). Between the two FLAIR imaging sets, there was no significant difference of signal intensity ratio (mean, standard deviation; 1.25 ± 0.20; 1.24 ± 0.20, respectively) (P > 0.05).
CONCLUSION
For the determination of mismatch or match between DWI and FLAIR imaging, there is no significant difference between FLAIR9000 and FLAIR6000 at 3T with a 32-channel coil.
Keyword
MeSH Terms
Figure
Reference
-
1. Hacke W, Donnan G, Fieschi C, et al. Association of outcome with early stroke treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet. 2004; 363:768–774.2. Del Zoppo GJ, Saver JL, Jauch EC, Adams HP Jr. American Heart Association Stroke Council. Expansion of the time window for treatment of acute ischemic stroke with intravenous tissue plasminogen activator: a science advisory from the American Heart Association/American Stroke Association. Stroke. 2009; 40:2945–2948.3. Balami JS, Hadley G, Sutherland BA, Karbalai H, Buchan AM. The exact science of stroke thrombolysis and the quiet art of patient selection. Brain. 2013; 136:3528–3553.4. European Stroke Organisation (ESO) Executive Committee. ESO Writing Committee. Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovasc Dis. 2008; 25:457–507.5. Adams HP Jr, del Zoppo G, Alberts MJ, et al. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: The American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Circulation. 2007; 115:e478–e534.6. Barber PA, Zhang J, Demchuk AM, Hill MD, Buchan AM. Why are stroke patients excluded from TPA therapy? An analysis of patient eligibility. Neurology. 2001; 56:1015–1020.7. Thomalla G, Rossbach P, Rosenkranz M, et al. Negative fluid-attenuated inversion recovery imaging identifies acute ischemic stroke at 3 hours or less. Ann Neurol. 2009; 65:724–732.8. Thomalla G, Cheng B, Ebinger M, et al. DWI-FLAIR mismatch for the identification of patients with acute ischaemic stroke within 4.5 h of symptom onset (PREFLAIR): a multicentre observational study. Lancet Neurol. 2011; 10:978–986.9. Petkova M, Rodrigo S, Lamy C, et al. MR imaging helps predict time from symptom onset in patients with acute stroke: implications for patients with unknown onset time. Radiology. 2010; 257:782–792.10. Koga M, Toyoda K, Kimura K, et al. THrombolysis for Acute Wake-up and unclear-onset Strokes with alteplase at 0.6 mg/kg (THAWS) Trial. Int J Stroke. 2014; 9:1117–1124.11. Thomalla G, Fiebach JB, Ostergaard L, et al. A multicenter, randomized, double-blind, placebo-controlled trial to test efficacy and safety of magnetic resonance imaging-based thrombolysis in wake-up stroke (WAKE-UP). Int J Stroke. 2014; 9:829–836.12. Nael K, Khan R, Choudhary G, et al. Six-minute magnetic resonance imaging protocol for evaluation of acute ischemic stroke: pushing the boundaries. Stroke. 2014; 45:1985–1991.13. Griswold MA, Jakob PM, Heidemann RM, et al. Generalized autocalibrating partially parallel acquisitions (GRAPPA). Magn Reson Med. 2002; 47:1202–1210.14. Wiesinger F, Van de Moortele PF, Adriany G, De Zanche N, Ugurbil K, Pruessmann KP. Potential and feasibility of parallel MRI at high field. NMR Biomed. 2006; 19:368–378.15. Meshksar A, Villablanca JP, Khan R, Carmody R, Coull B, Nael K. Role of EPI-FLAIR in patients with acute stroke: a comparative analysis with FLAIR. AJNR Am J Neuroradiol. 2014; 35:878–883.16. Galinovic I, Puig J, Neeb L, et al. Visual and region of interest-based inter-rater agreement in the assessment of the diffusion-weighted imaging- fluid-attenuated inversion recovery mismatch. Stroke. 2014; 45:1170–1172.17. Saver JL. Time is brain--quantified. Stroke. 2006; 37:263–266.18. Gagoski BA, Bilgic B, Eichner C, et al. RARE/turbo spin echo imaging with simultaneous multislice wave-CAIPI. Magn Reson Med. 2015; 73:929–938.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Comparison of Lesion Detection and Conspicuity on T2-weighted Images (T2 FFE), FLAIR and Diffusion-weighted Images in Patients with Traumatic Brain Injury
- Detection of Acute Intraventricular Hemorrhage: Comparison of FLAIR MR Imaging with Unenhanced CT
- Contrast-enhanced Fast Fluid-attenuated Inversion Recovery MR Imaging in Patients with Brain Tumors
- MR Imaging with FLAIR Pulse Sequence in Various Cerebral Lesions: Comparison with T2-Weighted Imaging
- Fast FLAIR MR Imaging Finidngs of Cerebral Infarction: Comparison with T2-Weighted Spin Echo Imaging