J Korean Soc Spine Surg.
2004 Dec;11(4):223-230.
Transforaminal Lumbar Interbody Fusion for the Treatment of Nonunion after Posterolateral Lumbar Fusion
- Affiliations
-
- 1Department of Orthopaedic Surgery, Konkuk University Minjoong Hospital, Seoul, Korea.
- 2Department of Orthopaedic Surgery, Seoul Veterans Hospital, Seoul, Korea. drortho@korea.com
- 3Department of Orthopaedic Surgery, Daejeon Veterans Hospital, Seoul, Korea.
Abstract
- STUDY DESIGN: A retrospective study
OBJECTIVES
To evaluate the clinical and radiological results of a transforaminal lumbar interbody fusion for the treatment of non-union after a posterolateral spinal fusion. LITERATURE REVIEW SUMMARY: In the case of nonunion after a posterolateral spinal fusion, the anterior column should be reconstructed. However, due to epidural scarring and fibrosis, the approach to the anterior column by conventional posterior lumbar interbody fusion (PLIF) is difficult. The authors have modified the original transforaminal lumbar interbody fusion (TLIF) developed by Dr. Harms, which offers potential advantages and provides a surgical alternative to the traditional methods.
MATERIALS AND METHODS
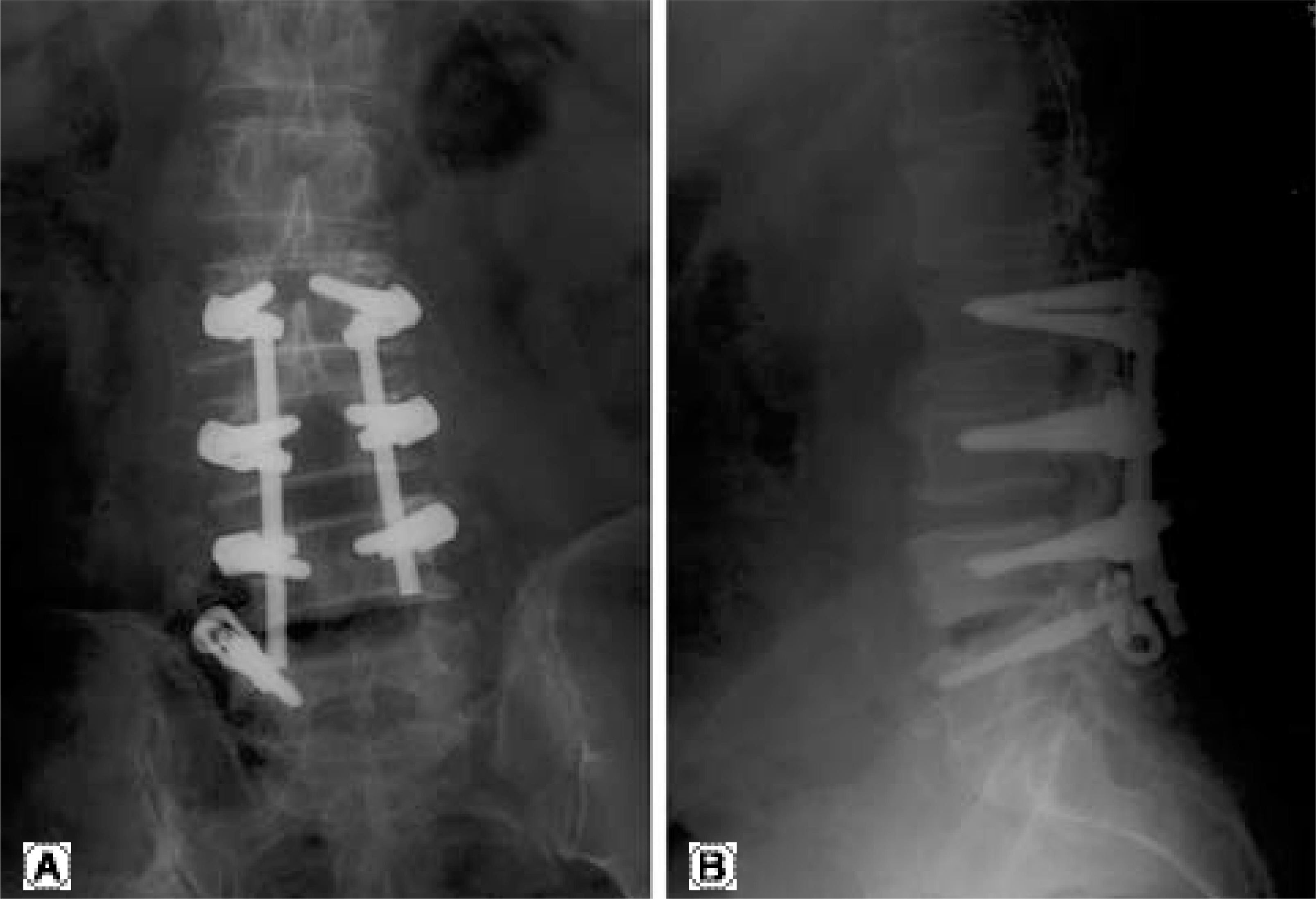
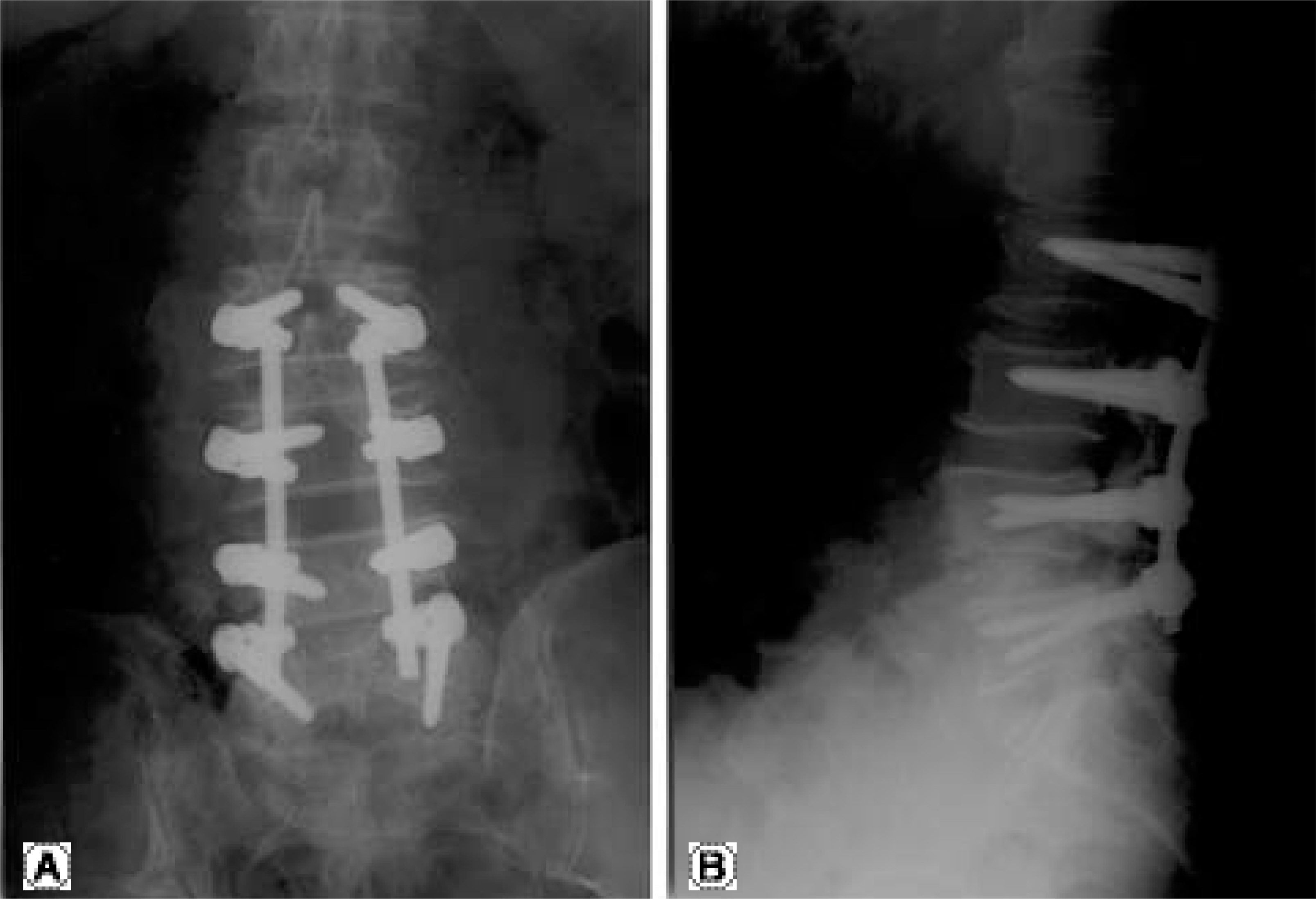
Between January 2002 and August 2003, 10 cases of TLIF for the treatment of non-unions after a posterolateral spinal fusion were performed. There were 8 male and 2 female cases. The mean age of the patient was 63.3 years, ranging from 53 to 75 years. The levels of the TLIF were the L4-5 and L5-S1 in 9 and 1 cases, respectively. The mean interval between the revision and previous operations was 21.3 months, ranging 12 to 48 months. In the preoperative radiography, bony defect in posterolateral fusion mass, halos around screws and abnormal motions in the stress view were observed. Using the previous midline approach, exposure of the bilateral articular and transverse processes were performed. With a small osteotome, the superior articular process was removed along a line parallel to the superior margins of the pedicular screw head, to allow access to the neural foramen and lateral aspect of the disc space. The TLIF was performed through this space by inserting cages. The loosened screw was replaced by one that was thicker, coupled with a cancellous bone graft in the foramen.
RESULTS
The average operation time and blood loss were 224 min. and 727 cc, respectively. Using Kirkaldy-Willis categories, the results were excellent in 1 case, good in 7, fair in 1 and poor in a further 1 case, with 1 case of nonunion was observed postoperatively.
CONCLUSIONS
The transforaminal lumbar interbody fusion for the treatment of nonunion after a posterolateral spinal fusion is a reliable and safe technique, which seems to have the merit of less morbidity.
MeSH Terms
Figure
Reference
-
1). Gertzbein SD, Hollopeter MR, Hall S. Pseudoarthrosis of the lumbar spine: Outcome after circumferential fusion. Spine. 1998; 23:2352–2357.2). Moskowitz A. Transforaminal lumbar interbody fusion. Orthop Clin North Am. 2002; 33:359–366.
Article3). Stauffer RN, Coventry MB. Anterior interbody lumbar spine fusion analysis of Mayo Clinic series. J Bone Joint Surg[Am]. 1972; 54:756–768.4). Buttermann GR, Glazer PA, Hu SS, Bradford DS. Revision of failed lumbafusions. A comparison of anterior autograft and allograft. Spine. 1997; 22:2748–2755.5). Albert TJ, Pinto M, Denis F. Management of symptomatic lumbar pseudoarthrosis with anteriorposterior fusion A functional and radiographic outcome study. Spine. 2000; 25:123–130.6). Duggal N, Mendiondo I, Pares HR, et al. Anterior lumbar interbody fusion for treatment of failed back surgery syndrome: an outcome analysis. Neurosurgery. 2004; 54:636–643.
Article7). Kim KT, Suk KS, Lee SH, Kim JM. Revision arthrodesis after lumbar fusion in degenerative lumbar disease. J Kor Orthop Assoc. 2003; 38:659–664.
Article8). Lauerman WC, Bradford DS, Ogilvie JW, Transfeldt EE. Results of lumbar pseudarthrosis repair. J Spinal Disord. 1992; 5:149–157.
Article9). Waddell G, Kummel EG, Lotto WN, Graham JD, Hall H, McCulloch JA. Failed lumbar disc surgery and repeat surgery following industrial injuries. J Bone Joint Surg[Am]. 1979; 61:201–207.
Article10). Suk SI, Lee CK, Kim WJ, Lee JH, Cho KJ, Kim HG. Adding posterior lumbar interbody fusion to pedicle screw fixation and posterolateral fusion after decompression in spondylolytic spondylolisthesis. Spine. 1997; 22:210–220.
Article11). Humphreys SC, hodges SD, Patwardhan AG, et al. Comparison of posterior and transforaminal approaches to lumbar interbody fusion. Spine. 2001; 26:567–571.
Article12). Salehi SA. Tawk R, Ganju A, LaMarca F, Liu JC, Ondra SL. Transforaminal lumbar interbody fusion: Surgical technique and results in 24 patients. Neurosurgery. 2004; 54:368–372.13). Whitecloud III TS, Roesch WW, Ricciardi JE. Transforaminal interbody fusion versus anteriorposterior interbody fusion of the lumbar spine: a financial analysis. J Spinal Disord. 2001; 14:100–103.14). Kirkaldy-Willis WH, Paine KWE, Cauchoix J, McIvor G. Lumbar spinal stenosis. Clin Orthop. 1974; 99:30–50.15). Fischgrund JS, Mackay M, Herkowitz HN, Brower R, Montgomery DM, Kurz LT. Degenerative lumbar spondylolisthesis with spinal stenosis: A prospective, randomized study comparing decompressive laminectomy and arthrodesis with and without spinal instrumentation. Spine. 1997; 22:2807–2812.16). Cohen DB, Chotivichit A, Fujita T, et al. Pseudoarthrosis repair. Clin Orthop. 2000; 371:46–55.17). Larsen JM, Rimold RL, Capen DA, Nelson RW, Nagel-berg S, Thomas Jr JC. Assessment of pseudarthrosis in pedicle screw fusion: A prospective study comparing plain radiographs, flexion/extension radiographs, CT scanning, and bone scintigraphy with operative findings. J Spinal Disord. 1996; 9:117–120.18). Harms JG, Jeszenszky D. The unilateral, transforaminal approach for posterior lumbar interbody fusion. Orthop Traumatol. 1998; 6:88–99.19). Kwon BK, Berta S, Daffner SD, et al. Ra dio gra phi c analysis of transforaminal lumbar interbody fusion for the treatment of adult isthmic spondylolisthesis. J of spinal disorders and techniques. 2003; 5:469–476.20). Lee SH, Shim JI, Kim TS, Kim YB, Ko DC. Reconstruction of lumbar kyphosis with circumferential fusion by posterior-anteriorposterior approach. J of Kor Spine Surg. 2001; 8:541–547.
Article21). Lowe TG, Tahernia AD, O’ Brien MF, Smith DAB. Unilateral transforaminal posterior interbody fsion(TLIF): Indications, techniques, and 2-year results. J of Spinal Disorders & Techniques. 2002; 15:31–38.22). West JL, Bradford DS, Ogilvie JW. Result of spinal arthrodesis with pedicle screw-plate fixation. J Bone Joint Surg[Am]. 1991; 73:1179–84.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Uniportal Endoscopic Lumbar Interbody Fusion
- A Comparison of Posterolateral and Posterior Interbody Fusion in the Surgical Treatment of Lumbar Spondylolisthesis
- Comparison between Posterior Lumbar Interbody Fusion with Pedicle Screw Fixation and Posterolateral Fusion with Pedicle Screw Fixation in Spondylolytic Spondylolisthesis in Adults
- Comparison of Outcomes of Multi-Level Anterior, Oblique, Transforaminal Lumbar Interbody Fusion Surgery : Impact on Global Sagittal Alignment
- Comparison between Posterolateral Fusion with Pedicle Screw Fixation and Anterior Interbody Fusion with Pedicle Screw Fixation in Spondylolytic Spondylolisthesis of the Lumbar Spine