J Korean Soc Spine Surg.
2011 Sep;18(3):117-122.
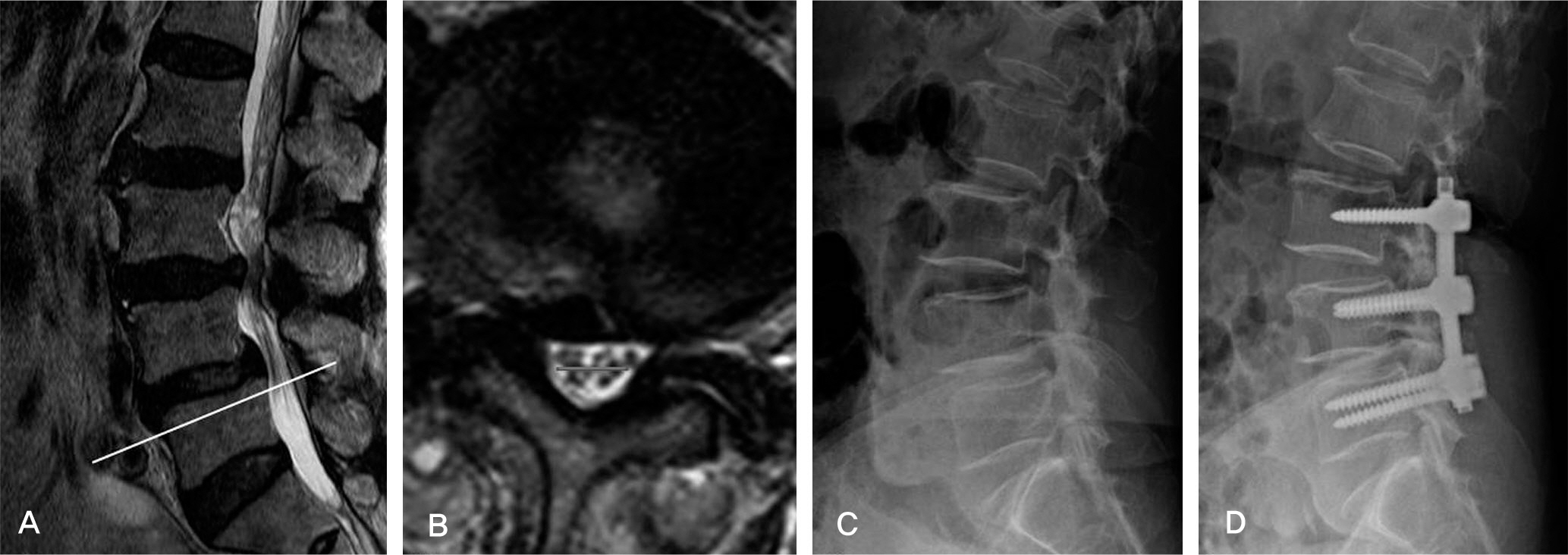
Clinical Value of Nerve Root Sedimentation Sign in Lumbar Spinal Stenosis
- Affiliations
-
- 1Department of Orthopedic Surgery, College of Medicine, Dong-A University, Korea. gylee@dau.ac.kr
Abstract
- STUDY DESIGN: A retrospective study.
OBJECTIVES
To assess the diagnostic value of the sedimentation sign seen on MRI with lumbar spinal stenosis and to compare postoperative clinical results. SUMMARY OF LITERATURE REVIEW: Nerve root sedimentation sign is an additional tool to diagnose lumbar spinal stenosis.
MATERIALS AND METHODS
There were 302 patients enrolled that had been diagnosed with lumbar spinal stenosis by MRI, which were reviewed to identify a sedimentation sign and all underwent the operative treatment. There were 142 patients who could not have their spinal stenosis diagnosis confirmed by MRI, and thus were selected as the control group to estimate the diagnostic value of nerve root sedimentation sign. Correlation with the duration of preoperative symptoms and the number of involved segments were compared and analyzed between sedimentation sign positive (Group I) and negative (Group II). We estimated Million Visual Analogue Score (MVAS) and Korean Oswestry Disability Index (KODI) for the assessment of the pain and the functional disability.
RESULTS
A positive sedimentation sign was found in 265 patients (87.7%) and diagnostic value was statistically significant (P<0.001). The involvement of 2 or more segments was significantly correlated with the sedimentation sign in the positive group (P<0.001). MVAS presented the improvement of 64.5+/-4.6%, KODI, 62.9+/-3.9% after surgical treatment in Group I. In Group II, each score showed improvement of 34.6+/-2.3% (MVAS), 37.1+/-1.8% (KODI). The improvement of these scores in Group I was better than in Group II.
CONCLUSIONS
The nerve root sedimentation sign is an additional tool to diagnose lumbar spinal stenosis and the considerable factor to decide the operation.
MeSH Terms
Figure
Reference
-
1. Hanley EN, Phillips ED, Kostuik JP. Who should be fused? Frymoyer JW, editor. (ed):. The Adult Spine. New York: Raven Press;1991. p. 1893–917.2. Katz JN, Dalgas M, Stucki G, et al. Degenerative lumbar spinal stenosis. Diagnostic value of the history and physical examination. Arthritis Rheum. 1995; 38:1236–41.
Article3. Boswell MV, Trescot AM, Datta S, et al. Interventional techniques: evidence-based practice guidelines in the management of chronic spinal pain. Pain Physician. 2007; 10:7–111.4. Kang YH. Anatomic Consideration of Lumbar Spinal Stenosis. J Korean Soc Spine Surg. 2000; 7:94–9.5. Amundsen T, Weber H, Lilleå s F, Nordal HJ, Abdelnoor M, Magnaes B. Lumbar spinal stenosis. Clinical and radiologic features. Spine (Phila Pa 1976). 1995; 20:1178–86.6. Kraft GH. Dermatomal somatosensory-evoked potentials in the evaluation of lumbosacral spinal stenosis. Phys Med Rehabil Clin N Am. 2003; 14:71–5.
Article7. Wang YC, Jeng CM, Wu CY, et al. Dynamic effects of axial loading on the lumbar spine during magnetic resonance imaging in patients with suspected spinal stenosis. J Formos Med Assoc. 2008; 107:334–9.
Article8. Cook C, Brown C, Michael K, et al. The clinical value of a cluster of patient history and observational findings as a diagnostic support tool for lumbar spine stenosis. Physiother Res Int. 2010; 11.
Article9. Cho KJ, Moon KH, Kim MK, et al. Changes of Clinical Outcomes after Decompression and Fusion for Spinal Stenosis during 2-Year Followup Periods. J Korean Soc Spine Surg. 2003; 10:113–8.
Article10. Ono A, Suetsuna F, Irie T, et al. Clinical significance of the redundant nerve roots of the cauda equina documented on magnetic resonance imaging. J Neurosurg Spine. 2007; 7:27–32.
Article11. Jackson A, Isherwood I. Does degenerative disease of the lumbar spine cause arachnoiditis? A magnetic resonance study and review of the literature. Br J Radiol. 1994; 67:840–7.
Article12. Laitt R, Jackson A, Isherwood I. Patterns of chronic adhesive arachnoiditis following Myodil myelography: the significance of spinal canal stenosis and previous surgery. Br J Radiol. 1996; 69:693–8.
Article13. Barz T, Melloh M, Staub LP, et al. Nerve root sedimentation sign: evaluation of a new radiological sign in lumbar spinal stenosis. Spine (Phila Pa 1976). 2010; 35:892–7.14. Chiodo A, Haig AJ, Yamakawa KS, Quint D, Tong H, Choksi VR. Magnetic resonance imaging vs. electrodiagnostic root compromise in lumbar spinal stenosis: a masked controlled study. Am J Phys Med Rehabil. 2008; 87:789–97.15. Herno A, Saari T, Suomalainen O, Airaksinen O. The degree of decompressive relief and its relation to clinical outcome in patients undergoing surgery for lumbar spinal stenosis. Spine (Phila Pa 1976). 1999; 24:1010–4.
Article16. Chung SS, Lee CS, Lee SG, Choi HJ, Park BJ. Correlation between Clinical Features and MRI Findings in One Level Lumbar Spinal Stenosis. J Korean Orthop Assoc. 1999; 34:541–6.
Article17. Olmarker K, Rydevik B. Single- versus double-level nerve root compression. An experimental study on the porcine cauda equina with analyses of nerve impulse conduction properties. orthop. 1992; 279:35–9.18. Javid MJ, Hadar EJ. Longterm followup review of patients who underwent laminectomy for lumbar stenosis: a prospective study. J Neurosurg. 1998; 89:1–7.
Article19. Fairbanks JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976). 2000; 25:2940–52.20. Sirvanci M, Bhatia M, Ganiyusufoglu KA, et al. Degenerative lumbar spinal stenosis: correlation with Oswestry Disability Index and MR imaging. Eur Spine J. 2008; 17:679–85.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Selective Spinal Nerve Root Block as Predictors of Outcome of Operative Treatment in the Lumbar Spine
- Can MRI Findings Help to Predict Neurological Recovery in Paraplegics With Thoracolumbar Fracture?
- Short-Term Effects of Selective Nerve Root Block in Spinal Stenosis Patients According to Spinal Canal Dimensions
- Rt S1 Root Block During Rt L5 Root Block in the Lumbar Radiculopathy
- L2 Root Block in Failed Back Surgery Syndrome