J Korean Soc Radiol.
2013 Jan;68(1):49-55.
Comparison of Different 3.0 T Magnetic Resonance Sequences for Lumbosacral Plexus and Its Branches: Preliminary Study
- Affiliations
-
- 1Department of Radiology, Seoul National University Bundang Hospital, Seongnam, Korea. joonwoo2@gmail.com
Abstract
- PURPOSE
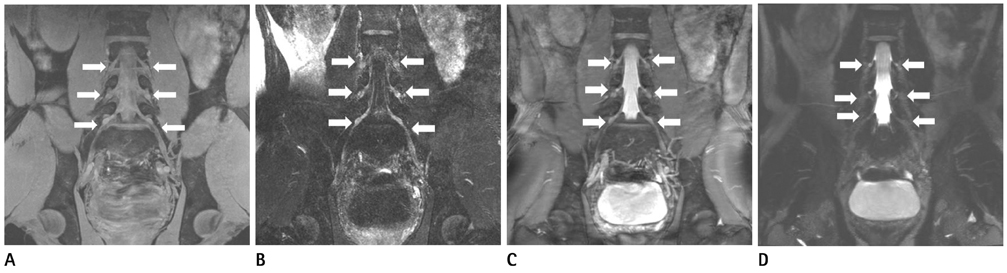
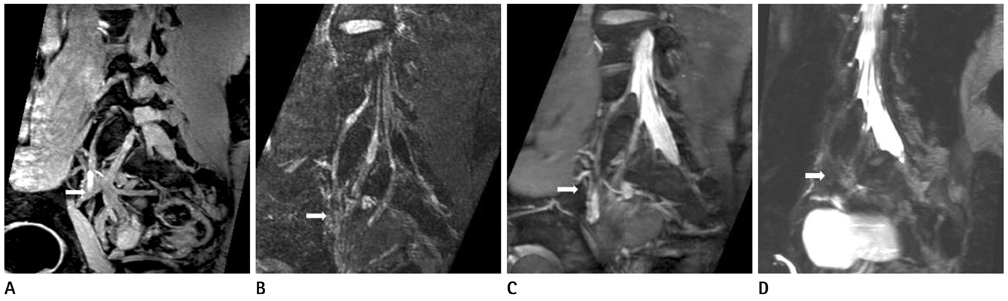
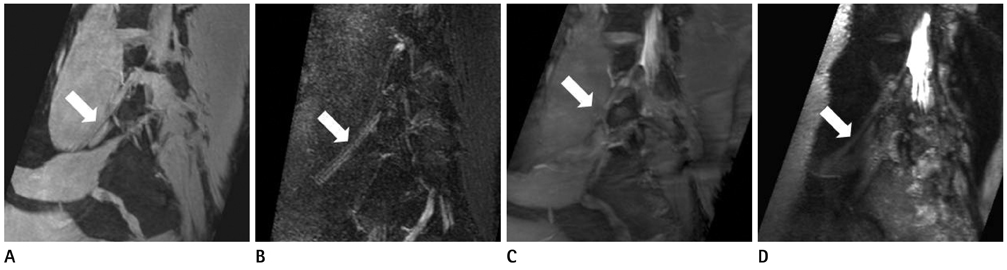
To prospectively evaluate four magnetic resonance sequences [ProSet, fluid attenuation inversion recovery (FLAIR), balanced turbo field echo (B-TFE), T2 Drive] for the lumbosacral plexus and its branches.
MATERIALS AND METHODS
Ten healthy volunteers who underwent four MRI sequences on lumbosacral area were evaluated for image quality (1 to 5; 1 = poor, 5 = excellent), the number of visualized bilateral spinal nerves from L2 to S1, the overlapping vessels obscuring the plexus (1 = many, 2 = some, 3 = few), and image quality defining spinal nerves (0 = nonvisualized, 1 = poor, 2 = moderate, 3 = good).
RESULTS
The ProSet (mean = 4.2, range 3-5) and B-TFE (mean = 3.7, range 3-5) showed better image quality than others. The number of visualized spinal nerves was the largest on ProSet image (mean = 9.2, range 8-10). FLAIR (mean = 2.1, range 1-3) and T2 Drive sequences (mean = 2.1, range 1-3) discriminated the nerves well from the vessels. The main branches of the lumbosacral plexus were well visualized on both ProSet (mean = 2.9, range 2-3) and FLAIR images (mean = 2.6, range 1-3). All of these were statistically significant.
CONCLUSION
ProSet is the best sequence in the evaluation of the lumbosacral plexus and its major branches while FLAIR can be a complementary sequence for the evaluation of nerves overlapping vascular structures.
MeSH Terms
Figure
Reference
-
1. Gierada DS, Erickson SJ. MR imaging of the sacral plexus: abnormal findings. AJR Am J Roentgenol. 1993. 160:1067–1071.2. Sasaka KK, Phisitkul P, Boyd JL, Marsh JL, El-Khoury GY. Lumbosacral nerve root avulsions: MR imaging demonstration of acute abnormalities. AJNR Am J Neuroradiol. 2006. 27:1944–1946.3. Blake LC, Robertson WD, Hayes CE. Sacral plexus: optimal imaging planes for MR assessment. Radiology. 1996. 199:767–772.4. Gierada DS, Erickson SJ, Haughton VM, Estkowski LD, Nowicki BH. MR imaging of the sacral plexus: normal findings. AJR Am J Roentgenol. 1993. 160:1059–1065.5. Aagaard BD, Maravilla KR, Kliot M. MR neurography. MR imaging of peripheral nerves. Magn Reson Imaging Clin N Am. 1998. 6:179–194.6. Filler AG, Howe FA, Hayes CE, Kliot M, Winn HR, Bell BA, et al. Magnetic resonance neurography. Lancet. 1993. 341:659–661.7. Filler AG, Maravilla KR, Tsuruda JS. MR neurography and muscle MR imaging for image diagnosis of disorders affecting the peripheral nerves and musculature. Neurol Clin. 2004. 22:643–682. vi–vii.8. Zhang ZW, Song LJ, Meng QF, Li ZP, Luo BN, Yang YH, et al. High-resolution diffusion-weighted MR imaging of the human lumbosacral plexus and its branches based on a steady-state free precession imaging technique at 3T. AJNR Am J Neuroradiol. 2008. 29:1092–1094.9. Lewis AM, Layzer R, Engstrom JW, Barbaro NM, Chin CT. Magnetic resonance neurography in extraspinal sciatica. Arch Neurol. 2006. 63:1469–1472.10. Freund W, Brinkmann A, Wagner F, Dinse A, Aschoff AJ, Stuber G, et al. MR neurography with multiplanar reconstruction of 3D MRI datasets: an anatomical study and clinical applications. Neuroradiology. 2007. 49:335–341.11. Chhabra A, Thawait GK, Soldatos T, Thakkar R, Del Grande F, Chalian M, et al. High-resolution 3T MR neurography of the brachial plexus and its branches, with emphasis on 3D imaging. AJNR Am J Neuroradiol. 2012. [Epub ahead of print].12. Chhabra A, Chalian M, Soldatos T, Andreisek G, Faridian-Aragh N, Williams E, et al. 3-T high-resolution MR neurography of sciatic neuropathy. AJR Am J Roentgenol. 2012. 198:W357–W364.13. Chhabra A, Andreisek G, Soldatos T, Wang KC, Flammang AJ, Belzberg AJ, et al. MR neurography: past, present, and future. AJR Am J Roentgenol. 2011. 197:583–591.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An Updated Review of Magnetic Resonance Neurography for Plexus Imaging
- MR Imaging of Lumbar Root Avulsion: Report of Two Case Studies
- Lumbosacral Plexus Conduction Study by Magnetic Stimulation
- MR Imaging of Radiation-Induced Lumbosacral Plexopathy, as a Rare Complication of Concomitant Chemo-Radiation for Cervical Cancer
- Role of MR Neurography for Evaluation of the Lumbosacral Plexus: A Scoping Review