J Korean Soc Radiol.
2013 Dec;69(6):427-431.
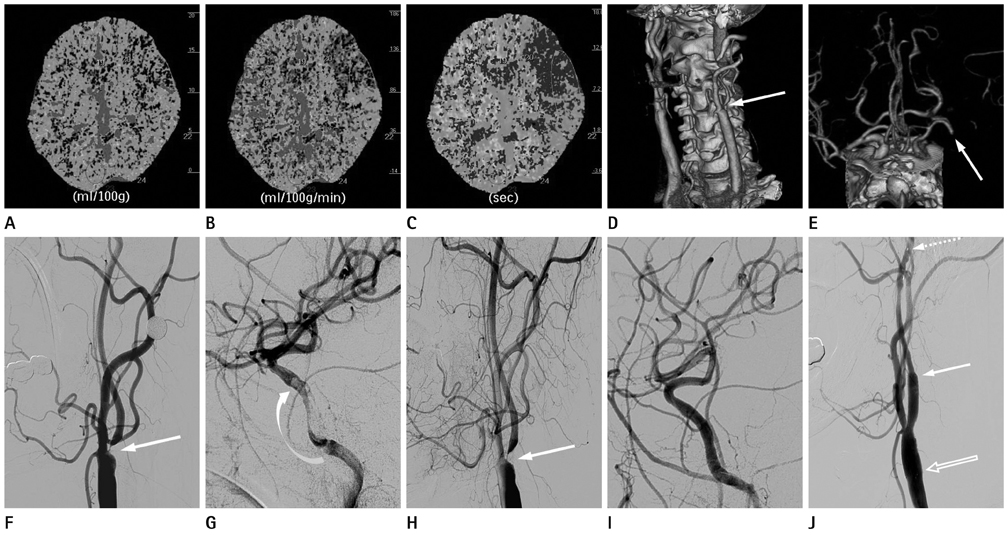
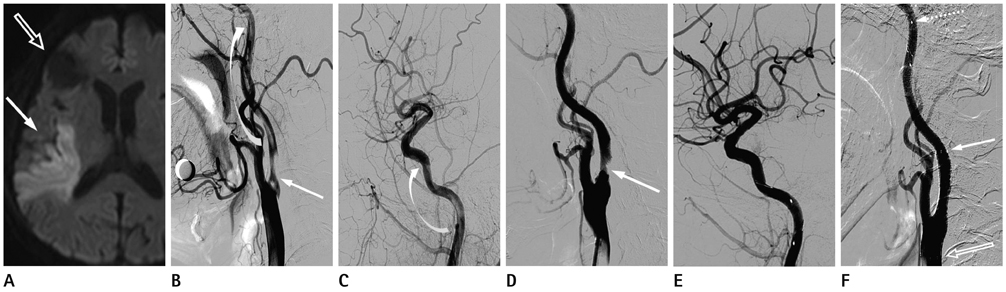
Carotid Artery Stenting in Patients with Critical Stenosis of Proximal Internal Carotid Artery and Large Distal Arterial Thrombus: 2 Case Reports
- Affiliations
-
- 1Department of Radiology, Kyung Hee University College of Medicine, Seoul, Korea.
- 2Department of Radiology, Kyung Hee University Hospital, Seoul, Korea. euijkim@hanmail.net
- 3Department of Neurology, Kyung Hee University Hospital, Seoul, Korea.
Abstract
- Determining the timing of carotid artery stenting in patients with carotid artery stenosis with a large territorial infarction is still controversial. Furthermore, it is more difficult to decide the timing of the procedure in cases with a coexisting tandem lesion, including distal arterial stenosis or thrombus. We report two cases of critical stenosis of the proximal internal carotid artery with a coexisting large distal arterial thrombus that presented as a large territorial infarction, that showed resolution of the distal arterial thrombus with stroke management after 3-4 weeks, and that were safely treated with carotid artery stenting.
MeSH Terms
Figure
Reference
-
1. Jovin TG, Gupta R, Uchino K, Jungreis CA, Wechsler LR, Hammer MD, et al. Emergent stenting of extracranial internal carotid artery occlusion in acute stroke has a high revascularization rate. Stroke. 2005; 36:2426–2430.2. Gasecki AP, Ferguson GG, Eliasziw M, Clagett GP, Fox AJ, Hachinski V, et al. Early endarterectomy for severe carotid artery stenosis after a nondisabling stroke: results from the North American Symptomatic Carotid Endarterectomy Trial. J Vasc Surg. 1994; 20:288–295.3. Paty PS, Darling RC 3rd, Feustel PJ, Bernardini GL, Mehta M, Ozsvath KJ, et al. Early carotid endarterectomy after acute stroke. J Vasc Surg. 2004; 39:148–154.4. Yadav JS, Wholey MH, Kuntz RE, Fayad P, Katzen BT, Mishkel GJ, et al. Protected carotid-artery stenting versus endarterectomy in high-risk patients. N Engl J Med. 2004; 351:1493–1501.5. Mantese VA, Timaran CH, Chiu D, Begg RJ, Brott TG. CREST Investigators. The Carotid Revascularization Endarterectomy versus Stenting Trial (CREST): stenting versus carotid endarterectomy for carotid disease. Stroke. 2010; 41:10 Suppl. S31–S34.6. Mathur A, Roubin GS, Iyer SS, Piamsonboon C, Liu MW, Gomez CR, et al. Predictors of stroke complicating carotid artery stenting. Circulation. 1998; 97:1239–1245.7. Roubin GS, Iyer S, Halkin A, Vitek J, Brennan C. Realizing the potential of carotid artery stenting: proposed paradigms for patient selection and procedural technique. Circulation. 2006; 113:2021–2030.8. Delgado MG, Vega P, Mateos V, Bogousslavsky J. Large carotid thrombus. Cerebrovasc Dis. 2009; 27:617–618.9. Yamagami H, Kitagawa K, Ohtsuki T, Matsumoto M, Hori M. Embolic cerebral infarction caused by intraluminal thrombus in the carotid siphon successfully treated with combination of anticoagulant and antiplatelet drugs. Circ J. 2005; 69:1147–1149.10. Kaushansky K, Lichtman M. Williams hematology. 8th ed. China: McGraw Hill;2011. p. 1845–1861.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Transseptal Approach to Carotid Artery Stenting in Right Internal Carotid Stenosis
- Steerable Microcatheter Facilitates Navigation through Tortuous Internal Carotid Artery Lesions in Carotid Artery Stenting
- Carotid Artery Stenting
- Carotid Artery Stenting in a Patient with Spontaneous Recanalization of a Proximal Internal Carotid Artery Occlusion: a Case Report
- Pseudo-no-Reflow Phenomenon in Carotid Artery Stenting using FilterWire EX: Successful Recovery by Aspiration Thrombectomy