World J Mens Health.
2015 Apr;33(1):14-19. 10.5534/wjmh.2015.33.1.14.
The Effect of Two Weeks of Treatment with Dutasteride on Bleeding after Transurethral Resection of the Prostate
- Affiliations
-
- 1Department of Urology, Hanyang University College of Medicine, Seoul, Korea. moonuro@hanyang.ac.kr
- KMID: 2320735
- DOI: http://doi.org/10.5534/wjmh.2015.33.1.14
Abstract
- PURPOSE
Dutasteride affects the prostate by reducing intraprostatic dihydrotestosterone and prostate tissue vascularity. We evaluated the effect of pretreatment with dutasteride for two weeks on perioperative and postoperative bleeding during transurethral resection of the prostate (TURP).
MATERIALS AND METHODS
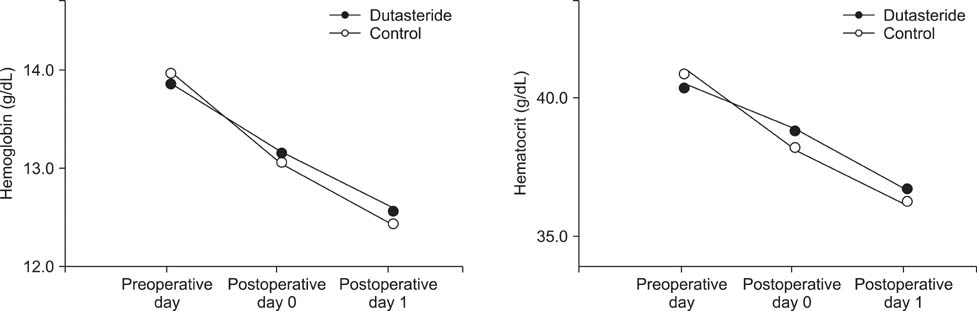
Eighty-three patients who had benign prostatic hyperplasia together with the criteria for eligibility for TURP were included. The dutasteride group consisted of 40 patients who were treated with dutasteride (0.5 mg/d) for two weeks before surgery, and the control group consisted of 43 patients who did not receive dutasteride. Blood loss was evaluated in terms of reduction in serum hemoglobin (Hb) and hematocrit (Hct) levels, which were measured before, immediately after, and 24 hours after surgery. We also measured the durations of indwelling urethral catheter use, continuous saline bladder irrigation, and hospitalization.
RESULTS
Lower mean blood loss was observed in the dutasteride group than the control group immediately after and 24 hours after surgery (DeltaHb=0.65+/-1.27 g/dL vs. 1.16+/-0.73 g/dL, 1.30+/-1.00 g/dL vs. 1.86+/-1.05 g/dL respectively, p=0.019, p=0.011; DeltaHct=1.89%+/-3.83% vs. 3.47%+/-2.09%, 3.69%+/-2.95% vs. 5.39%+/-3.23% respectively, p=0.016, p=0.011). In addition, there were fewer days of indwelling urethral catheter use (2.95+/-1.02 d vs. 3.92+/-1.14 d, p=0.000), continuous saline bladder irrigation (1.81+/-1.08 d vs. 2.36+/-1.06 d, p=0.016), and hospitalization after TURP (3.95+/-1.09 d vs. 4.76+/-1.19 d, p=0.001) in the dutasteride group.
CONCLUSIONS
Preoperative treatment with dutasteride for two weeks before TURP reduces surgical bleeding and length of hospitalization after TURP. This pretreatment can be used to decrease surgical bleeding associated with TURP.
MeSH Terms
Figure
Reference
-
1. Rassweiler J, Teber D, Kuntz R, Hofmann R. Complications of transurethral resection of the prostate (TURP)--incidence, management, and prevention. Eur Urol. 2006; 50:969–979.
Article2. Reich O, Seitz M, Gratzke C, Schlenker B, Walther S, Stief C. Benign prostatic hyperplasia (BPH): surgical therapy options. Urologe A. 2010; 49:113–126.3. El-Hakim A. TURP in the new century: an analytical reappraisal in light of lasers. Can Urol Assoc J. 2010; 4:347–349.
Article4. Wilson JD. Role of dihydrotestosterone in androgen action. Prostate Suppl. 1996; 6:88–92.
Article5. Kravchick S, Cytron S, Mamonov A, Peled R, Linov L. Effect of short-term dutasteride therapy on prostate vascularity in patients with benign prostatic hyperplasia: a pilot study. Urology. 2009; 73:1274–1278.
Article6. Zaitsu M, Tonooka A, Mikami K, Hattori M, Takeshima Y, Uekusa T, et al. A dual 5α-reductase inhibitor dutasteride caused reductions in vascular density and area in benign prostatic hyperplasia. ISRN Urol. 2013; 2013:863489.
Article7. Pastore AL, Mariani S, Barrese F, Palleschi G, Valentini AM, Pacini L, et al. Transurethral resection of prostate and the role of pharmacological treatment with dutasteride in decreasing surgical blood loss. J Endourol. 2013; 27:68–70.
Article8. Hahn RG, Fagerström T, Tammela TL, Van Vierssen Trip O, Beisland HO, Duggan A, et al. Blood loss and postoperative complications associated with transurethral resection of the prostate after pretreatment with dutasteride. BJU Int. 2007; 99:587–594.
Article9. Mitterberger M, Pinggera G, Horninger W, Strasser H, Halpern E, Pallwein L, et al. Dutasteride prior to contrastenhanced colour Doppler ultrasound prostate biopsy increases prostate cancer detection. Eur Urol. 2008; 53:112–117.
Article10. Ekman P. Finasteride in the treatment of benign prostatic hypertrophy: an update. New indications for finasteride therapy. Scand J Urol Nephrol Suppl. 1999; 203:15–20.
Article11. Miller MI, Puchner PJ. Effects of finasteride on hematuria associated with benign prostatic hyperplasia: long-term follow-up. Urology. 1998; 51:237–240.
Article12. Pareek G, Shevchuk M, Armenakas NA, Vasjovic L, Hochberg DA, Basillote JB, et al. The effect of finasteride on the expression of vascular endothelial growth factor and microvessel density: a possible mechanism for decreased prostatic bleeding in treated patients. J Urol. 2003; 169:20–23.
Article13. Boccon-Gibod L, Valton M, Ibrahim H, Boccon-Gibod L, Comenducci A. Effect of dutasteride on reduction of intraoperative bleeding related to transurethral resection of the prostate. Prog Urol. 2005; 15:1085–1089.14. Shanmugasundaram R, Singh JC, Kekre NS. Does dutasteride reduce perioperative blood loss and postoperative complications after transurethral resection of the prostate. Indian J Urol. 2007; 23:334–335.15. Martov AG, Ergakov DV. The experience in dutasteride use before transurethral prostatic resection for large adenoma. Urologiia. 2008; (4):46.16. Pastore AL, Mariani S, Barrese F, Palleschi G, Valentini AM, Pacini L, et al. Transurethral resection of prostate and the role of pharmacological treatment with dutasteride in decreasing surgical blood loss. J Endourol. 2013; 27:68–70.
Article17. Woo JH, Kang JY, Kim EK, Yoo TK. The effect of short term dutasteride therapy on microvessel density in benign prostatic hyperplasia. Korean J Urol. 2008; 49:515–519.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hematuria after Transurethral Resection of the Prostate
- The Effect of Short Term Dutasteride Therapy on Microvessel Density in Benign Prostatic Hyperplasia
- Clinical Observation on Transurethral Resection of Prostate and Suprapubic Prostatectomy for Benign Prostatic Hypertrophy
- Positive Role of Dutasteride in the Treatment of Localized Prostate Cancer
- Fluid extravasation caused by bladder perforation during bipolar transurethral resection using saline solution: a case report