Tuberc Respir Dis.
2014 Oct;77(4):167-171. 10.4046/trd.2014.77.4.167.
Effect of Inhaled Tiotropium on Spirometric Parameters in Patients with Tuberculous Destroyed Lung
- Affiliations
-
- 1Department of Internal Medicine, Inje University Seoul Paik Hospital, Inje University College of Medicine, Seoul, Korea. pulho@korea.com
- KMID: 2320573
- DOI: http://doi.org/10.4046/trd.2014.77.4.167
Abstract
- BACKGROUND
In Korea, patients with destroyed lung due to tuberculosis (TB) account for a significant portion of those affected by chronic pulmonary function impairment. The objective of our research was to evaluate the efficacy of inhaled tiotropium bromide in TB destroyed lung.
METHODS
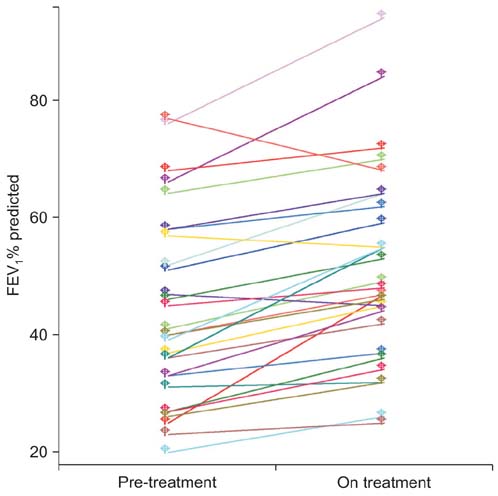
We compared the effectiveness of inhaled tiotropium bromide for 2 months between pre- and post-treatment pulmonary function tests performed on 29 patients with destroyed lung due to TB.
RESULTS
The mean age of the total number of patients was 63+/-9 years, where 15 patients were male. The pre-treatment mean forced expiratory volume in 1 second (FEV1) was 1.02+/-0.31 L (44.1+/-16.0% predicted). The pre-treatment mean forced vital capacity (FVC) was 1.70+/-0.54 L (52.2+/-15.8% predicted). Overall, the change in FEV1% predicted over baseline with tiotropium was 19.5+/-19.1% (p<0.001). Twenty patients (72%) got better than a 10% increase in FEV1 over baseline with tiotropium, but one patient showed more than a 10% decrease in FEV1. Overall, the change in FVC% predicted over baseline with tiotropium was 18.5+/-19.9% (p<0.001). Seventeen patients (59%) experienced greater than a 10% increase in FVC over baseline with tiotropium; 12 (41%) patients had stable lung function.
CONCLUSION
The inhaled tiotropium bromide therapy may lead to improve lung functions in patients with TB destroyed lung. However, the long-term effectiveness of this treatment still needs to be further assessed.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Factors Associated with Indacaterol Response in Tuberculosis-Destroyed Lung with Airflow Limitation
Tae Hoon Kim, Chin Kook Rhee, Yeon-Mok Oh
Tuberc Respir Dis. 2019;82(1):35-41. doi: 10.4046/trd.2018.0050.
Reference
-
1. Kim HY, Song KS, Goo JM, Lee JS, Lee KS, Lim TH. Thoracic sequelae and complications of tuberculosis. Radiographics. 2001; 21:839–858.2. Ramos LM, Sulmonett N, Ferreira CS, Henriques JF, de Miranda SS. Functional profile of patients with tuberculosis sequelae in a university hospital. J Bras Pneumol. 2006; 32:43–47.3. Plit ML, Anderson R, Van Rensburg CE, Page-Shipp L, Blott JA, Fresen JL, et al. Influence of antimicrobial chemotherapy on spirometric parameters and pro-inflammatory indices in severe pulmonary tuberculosis. Eur Respir J. 1998; 12:351–356.4. Lee JH, Chang JH. Lung function in patients with chronic airflow obstruction due to tuberculous destroyed lung. Respir Med. 2003; 97:1237–1242.5. Lam KB, Jiang CQ, Jordan RE, Miller MR, Zhang WS, Cheng KK, et al. Prior TB, smoking, and airflow obstruction: a cross-sectional analysis of the Guangzhou Biobank Cohort Study. Chest. 2010; 137:593–600.6. Pasipanodya JG, Miller TL, Vecino M, Munguia G, Bae S, Drewyer G, et al. Using the St. George respiratory questionnaire to ascertain health quality in persons with treated pulmonary tuberculosis. Chest. 2007; 132:1591–1598.7. Pasipanodya JG, Miller TL, Vecino M, Munguia G, Garmon R, Bae S, et al. Pulmonary impairment after tuberculosis. Chest. 2007; 131:1817–1824.8. Long R, Maycher B, Dhar A, Manfreda J, Hershfield E, Anthonisen N. Pulmonary tuberculosis treated with directly observed therapy: serial changes in lung structure and function. Chest. 1998; 113:933–943.9. Menezes AM, Hallal PC, Perez-Padilla R, Jardim JR, Muino A, Lopez MV, et al. Tuberculosis and airflow obstruction: evidence from the PLATINO study in Latin America. Eur Respir J. 2007; 30:1180–1185.10. Willcox PA, Ferguson AD. Chronic obstructive airways disease following treated pulmonary tuberculosis. Respir Med. 1989; 83:195–198.11. Snider GL, Doctor L, Demas TA, Shaw AR. Obstructive airway disease in patients with treated pulmonary tuberculosis. Am Rev Respir Dis. 1971; 103:625–640.12. Saito Y, Azuma A, Morimoto T, Fujita K, Abe S, Motegi T, et al. Tiotropium ameliorates symptoms in patients with chronic airway mucus hypersecretion which is resistant to macrolide therapy. Intern Med. 2008; 47:585–591.13. Maesen FP, Smeets JJ, Sledsens TJ, Wald FD, Cornelissen PJ. Dutch Study Group. Tiotropium bromide, a new long-acting antimuscarinic bronchodilator: a pharmacodynamic study in patients with chronic obstructive pulmonary disease (COPD). Eur Respir J. 1995; 8:1506–1513.14. Celli BR, MacNee W. ATS/ERS Task Force. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J. 2004; 23:932–946.15. World Health Organization. Global tuberculosis control: surveillance, planning, financing: WHO report 2006. Geneva: World Health Organization;2008.16. American Thoracic Society. American Thoracic Society (ATS). the European Respiratory Society (ERS). Idiopathic pulmonary fibrosis: diagnosis and treatment. International consensus statement. Am J Respir Crit Care Med. 2000; 161(2 Pt 1):646–664.17. Chakrabarti B, Calverley PM, Davies PD. Tuberculosis and its incidence, special nature, and relationship with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2007; 2:263–272.18. Elkington PT, Friedland JS. Matrix metalloproteinases in destructive pulmonary pathology. Thorax. 2006; 61:259–266.19. Hnizdo E, Singh T, Churchyard G. Chronic pulmonary function impairment caused by initial and recurrent pulmonary tuberculosis following treatment. Thorax. 2000; 55:32–38.20. Salorinne Y, Stenius-Aarniala B, Poppius H. Effect of ipratropium bromide and fenoterol on airway obstruction in chronic pulmonary tuberculosis. Respiration. 1979; 38:151–154.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of inhaled tiotropium on patients with COPD
- Efficacy of Inhaled Iloprost in Cor Pulmonale and Severe Pulmonary Hypertension Associated with Tuberculous Destroyed Lung
- Validity and Reliability of CAT and Dyspnea-12 in Bronchiectasis and Tuberculous Destroyed Lung
- Change in Pulmonary Function Following Empyemectomy and Decortication in Tuberculous and Non-Tuberculous Chronic Empyema Thoracis
- Issues on Safety of Long-Acting Muscarinic Antagonist