Tuberc Respir Dis.
2012 Feb;72(2):212-217.
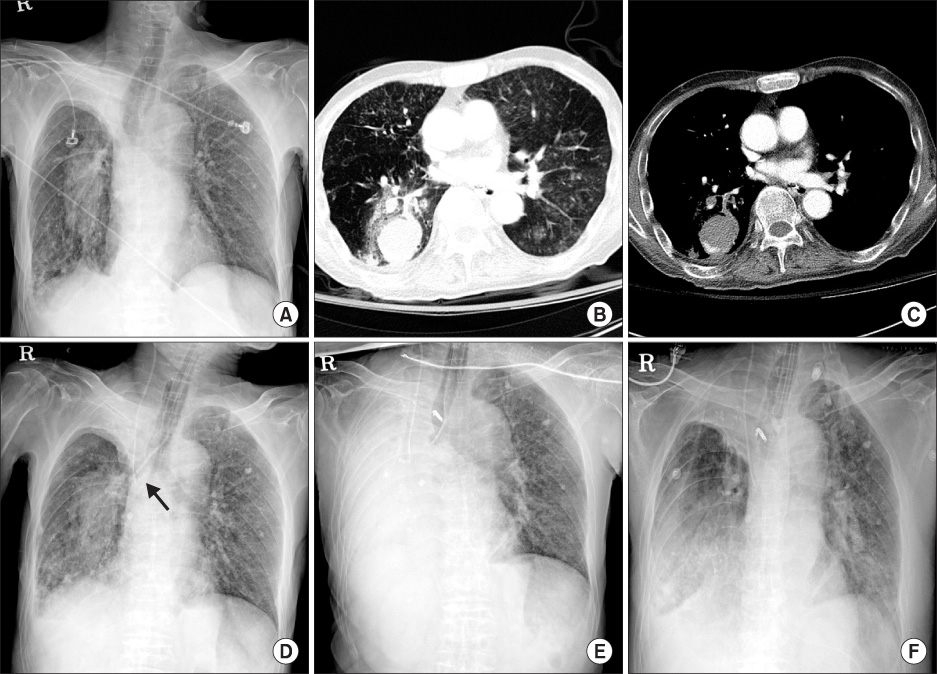
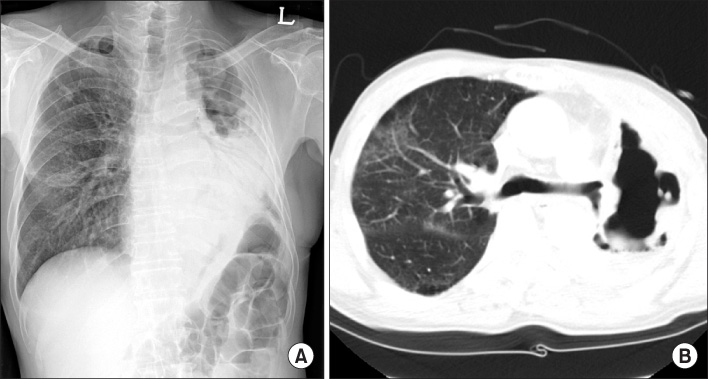
Massive Hemoptysis Cases Intubated with the Univent(R) Bronchial Blocker for Lung Protection
- Affiliations
-
- 1Department of Internal Medicine, Division of Pulmonology and Critical Care Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. yskoh@amc.seoul.kr
- 2Department of Internal Medicine, Division of Oncology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
Abstract
- Massive hemoptysis is a life-threatening condition and sometimes leads to death due to airway obstruction rather than exsanguinations. In a critical hemoptysis, endotracheal intubation may be necessary to maintain adequate gas exchange and protect the unaffected side of the lung. Bronchial blockers (BBs), commonly used technique for one-lung ventilation in thoracic or cardiac surgeries, are valuable devices for protecting the airway in massive endobronchial bleeding. We report three cases intubated with BBs, Univent(R), in massive hemoptysis. We suggest that BBs are one of the indispensable equipments for respiratory specialized wards and intensive care units.
Keyword
MeSH Terms
Figure
Reference
-
1. Garzon AA, Cerruti MM, Golding ME. Exsanguinating hemoptysis. J Thorac Cardiovasc Surg. 1982. 84:829–833.2. Santana-Cabrera L, Arroyo MF, Rodriguez AU, Sanchez-Palacios M. Double-lumen endobronchial tube in the emergency management of massive hemoptysis. J Emerg Trauma Shock. 2010. 3:305.3. Korean Academy of Tuberculosis and Respiratory Disease. Respiratory disease. 2004. Seoul: Koon Ja Publish Inc..4. Fauci AS, Braunwald E, Kasper D, Hauser S, Longo DL, Jameson JL, et al. Harrison's principles of internal medicine. 2008. 17th ed. New York: McGraw-Hill.5. Oh YS, Choi IH, Jung TW, Kwak IY. Clinical evaluation of univent tube for one lung ventilation. Korean J Anesthesiol. 1996. 30:41–45.6. Seo DM, Lee JH, Lee SG, Ban JS, Min BW. One lung ventilation using a uninvent® tube in a patient with permenant tracheostomy after total laryngectomy: a case report. Korean J Anesthesiol. 2006. 50:213–216.7. Jean-Baptiste E. Clinical assessment and management of massive hemoptysis. Crit Care Med. 2000. 28:1642–1647.8. Lopez JK, Lee HY. Bronchial artery embolization for treatment of life-threatening hemoptysis. Semin Intervent Radiol. 2006. 23:223–229.9. Chun JY, Morgan R, Belli AM. Radiological management of hemoptysis: a comprehensive review of diagnostic imaging and bronchial arterial embolization. Cardiovasc Intervent Radiol. 2010. 33:240–250.10. Jougon J, Ballester M, Delcambre F, Mac Bride T, Valat P, Gomez F, et al. Massive hemoptysis: what place for medical and surgical treatment. Eur J Cardiothorac Surg. 2002. 22:345–351.11. Campos JH, Hallam EA, Van Natta T, Kernstine KH. Devices for lung isolation used by anesthesiologists with limited thoracic experience: comparison of double-lumen endotracheal tube, Univent torque control blocker, and Arndt wire-guided endobronchial blocker. Anesthesiology. 2006. 104:261–266.12. Narayanaswamy M, McRae K, Slinger P, Dugas G, Kanellakos GW, Roscoe A, et al. Choosing a lung isolation device for thoracic surgery: a randomized trial of three bronchial blockers versus double-lumen tubes. Anesth Analg. 2009. 108:1097–1101.13. Ueda K, Goetzinger C, Gauger EH, Hallam EA, Campos JH. Use of bronchial blockers: a retrospective review of 302 cases. J Anesth. 2011. 10. 16. [Epub]. DOI:10.1007/s00540-011-1245-x.14. Inoue H, Shohtsu A, Ogawa J, Koide S, Kawada S. Endotracheal tube with movable blocker to prevent aspiration of intratracheal bleeding. Ann Thorac Surg. 1984. 37:497–499.15. Nishiumi N, Nakagawa T, Masuda R, Iwasaki M, Inokuchi S, Inoue H. Endobronchial bleeding associated with blunt chest trauma treated by bronchial occlusion with a Univent. Ann Thorac Surg. 2008. 85:245–250.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Degree of Bronchial Mucosal Damages Related to the Bronchial Blocker Cuff Pressure of Univent(R) Tube
- High Frequency Jet Ventilation of One Lung using a Bronchial Blocker of Univent during Carinal Resection
- Bronchial Cuff Volume of Univent Tube for One Lung Ventilation
- Clinical Evaluation of Univent Tube for One Lung Ventilation
- One Lung Ventilation of Bronchial Trifurcation Patients at the Carina: Two cases report