Restor Dent Endod.
2014 Feb;39(1):63-67.
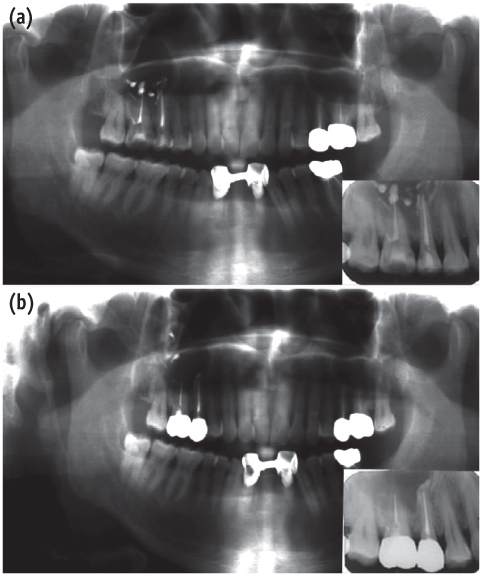
Chronic maxillary sinusitis caused by root canal overfilling of Calcipex II
- Affiliations
-
- 1Department of Conservative Dentistry, Gangneung-Wonju National University College of Dentistry, Gangneung, Korea.
- 2Department of Oral Pathology, Gangneung-Wonju National University College of Dentistry, Gangneung, Korea. sklee@kangnung.ac.kr
Abstract
- This is a case report of chronic maxillary sinusitis caused by root canal overfilling of Calcipex II (Techno-Dent). A 60 year-old male complained of dull pain in the right maxillary molar area after complicated endodontic treatment using Calcipex II paste and was finally diagnosed with a chronic maxillary sinusitis through a clinical and radiological observation. In the biopsy examination, the periapical granuloma contained a lot of dark and translucent Calcipex II granules which were not stained with hematoxylin and eosin. They were usually engulfed by macrophages but rarely resorbed, resulting in scattering and migrating into antral mucosa. Most of the Calcipex II granules were also accumulated in the cytoplasms of secretory columnar epithelial cells, and small amount of Calcipex II granules were gradually secreted into sinus lumen by exocytosis. However, chronic granulomatous inflammation occurred without the additional recruitment of polymorphonuclear leukocytes (PMNs) and lymphocytes, and many macrophages which engulfed the Calcipex II granules were finally destroyed in the processes of cellular apoptosis. It is presumed that Calcipex II granules are likely to have a causative role to induce the granulomatous foreign body inflammation in the periapical region, and subsequently to exacerbate the chronic maxillary sinusitis in this study.
MeSH Terms
-
Apoptosis
Biopsy
Cytoplasm
Dental Pulp Cavity*
Eosine Yellowish-(YS)
Epithelial Cells
Exocytosis
Foreign Bodies
Granuloma, Foreign-Body
Hematoxylin
Humans
Inflammation
Lymphocytes
Macrophages
Male
Maxillary Sinus*
Maxillary Sinusitis*
Middle Aged
Molar
Mucous Membrane
Neutrophils
Periapical Granuloma
Eosine Yellowish-(YS)
Hematoxylin
Figure
Reference
-
1. Kim JW, Cho KM, Park SH, Song SG, Park MS, Jung HR, Song JY, Kim YS, Lee SK. Overfilling of calcium hydroxide-based paste Calcipex II produced a foreign body granuloma without acute inflammatory reaction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 107:e73–e76.
Article2. Hosoya N, Kurayama H, Iino F, Arai T. Effects of calcium hydroxide on physical and sealing properties of canal sealers. Int Endod J. 2004; 37:178–184.
Article3. Manisali Y, Yücel T, Erişen R. Overfilling of the root. A case report. Oral Surg Oral Med Oral Pathol. 1989; 68:773–775.
Article4. Eda S, Kawakami T, Hasegawa H, Watanabe I, Kato K. Clinico-pathological studies on the healing of periapical tissues in aged patients by root canal filling using pastes of calcium hydroxide added iodoform. Gerodontics. 1985; 1:98–104.5. Nurko C, Garcia-Godoy F. Evaluation of a calcium hydroxide/iodoform paste (Vitapex) in root canal therapy for primary teeth. J Clin Pediatr Dent. 1999; 23:289–294.6. Mohammed M, Saujanya KP, Deepak J, Sangameshwar S, Arun A, Laxmi U, Mahnoor K. Role of calcium hydroxide in endodontics: a review. Glob J Med Public Health. 2012; 1:66–70.7. Lee JH, Baek SH, Bae KS. Evaluation of the cytotoxicity of calcium phosphate root canal sealers. J Korean Acad Conserv Dent. 2003; 28:295–302.
Article8. Nair PN, Sjögren U, Krey G, Sundqvist G. Therapy-resistant foreign body giant cell granuloma at the periapex of a root-filled human tooth. J Endod. 1990; 16:589–595.
Article9. Segura JJ, Llamas R, Rubio-Manzanares AJ, Jimenez-Planas A, Guerrero JM, Calvo JR. Calcium hydroxide inhibits substrate adherence capacity of macrophages. J Endod. 1997; 23:444–447.
Article10. Verdon C, Holz J. Root canal obturation based on Sealapex calcium hydroxide. A clinical and radiological follow-up after 1 year. Schweiz Monatsschr Zahnmed. 1990; 100:829–834.11. Soares J, Santos S, César C, Silva P, Sá M, Silveira F, Nunes E. Calcium hydroxide induced apexification with apical root development: a clinical case report. Int Endod J. 2008; 41:710–719.
Article12. De Moor RJ, De Witte AM. Periapical lesions accidentally filled with calcium hydroxide. Int Endod J. 2002; 35:946–958.
Article13. Lee Y. Effect of calcium hydroxide application time on dentin. Restor Dent Endod. 2013; 38:186.
Article14. Cruz EV, Kota K, Huque J, Iwaku M, Hoshino E. Penetration of propylene glycol into dentine. Int Endod J. 2002; 35:330–336.
Article15. McIntosh MP, Schwarting N, Rajewski RA. In vitro and in vivo evaluation of a sulfobutyl ether beta-cyclodextrin enabled etomidate formulation. J Pharm Sci. 2004; 93:2585–2594.
Article16. Faergemann J, Swanbeck G. Treatment of onychomycosis with a propylene glycol-urea-lactic acid solution. Mycoses. 1989; 32:536–540.
Article17. Horiguchi Y, Honda T, Fujii S, Matsushima S, Osaki Y. A case of allergic contact dermatitis from propylene glycol in an ultrasonic gel, sensitized at a leakage skin injury due to transcatheter arterial chemoembolization for hepatocellular carcinoma. Int J Dermatol. 2005; 44:681–683.
Article18. Nater JP, Baar AJ, Hoedemaeker J. Histological aspects of skin reactions to propylene glycol. Contact Dermatitis. 1977; 3:181–185.
Article19. Senthilmohan ST, McEwan MJ, Wilson PF, Milligan DB, Freeman CG. Real time analysis of breath volatiles using SIFT-MS in cigarette smoking. Redox Rep. 2001; 6:185–187.
Article20. Bledsoe KA, Kramer AH. Propylene glycol toxicity complicating use of barbiturate coma. Neurocrit Care. 2008; 9:122–124.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The fate of overfilling in root canal treatments with long-term follow-up: a case series
- A Case of Subactue Maxillary Sinusitis due to Dental Material
- Unilateral maxillary central incisor root resorption after orthodontic treatment for Angle Class II, division 1 malocclusion with significant maxillary midline deviation: A possible correlation with root proximity to the incisive canal
- Oroantral Fistula Originating from Osteomyelitis Accompanied by Maxillary Sinusitis
- The canal system in the mesiobuccal root of the maxillary first molar