Korean J Urol.
2013 Jan;54(1):42-47.
Is Concomitant Bladder Neck Reconstruction Necessary in Neurogenic Incontinent Patients Who Undergo Augmentation Cystoplasty?
- Affiliations
-
- 1Department of Urology, Seoul National University Hospital, Seoul, Korea. sjo@snu.ac.kr
- 2Department of Urology, Dongguk University Ilsan Hospital, Goyang, Korea.
- 3Department of Urology, Gachon University Gil Medical Center, Incheon, Korea.
Abstract
- PURPOSE
In patients with neurogenic bladder due to spinal cord injury or disease who undergo augmentation cystoplasty (AC) for not only bladder dysfunction but also sphincteric incontinence, the need for concomitant bladder neck reconstruction at the time of AC has not yet been established. The aim of this study was to evaluate whether concomitant bladder neck reconstruction is necessary when performing AC.
MATERIALS AND METHODS
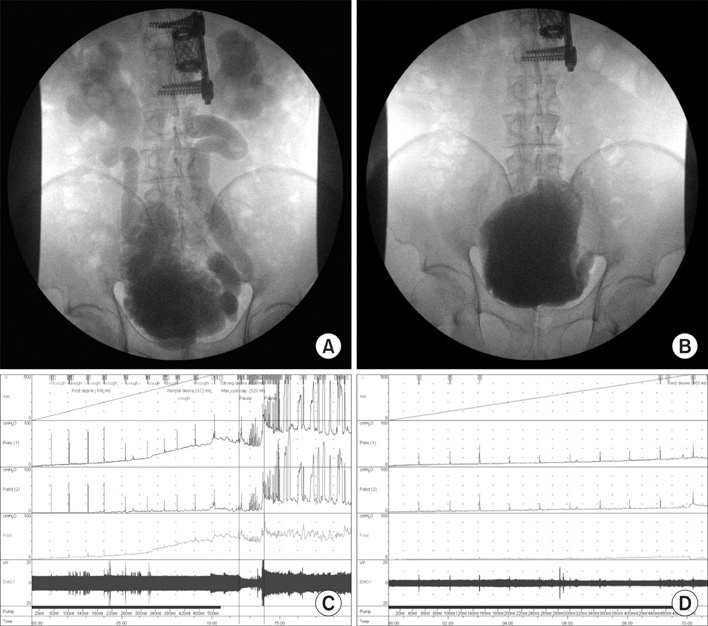
We retrospectively investigated 35 patients who underwent AC from January 2006 to September 2010. Medical history, preoperative and postoperative fluoroscopic urodynamic study (FUDS) parameters, and responses to an incontinence questionnaire (ICIQ Korean version) were reviewed.
RESULTS
A final analysis was performed on 17 patients (9 male, 8 female) who were diagnosed with sphincteric incontinence. Continence status, the number of pads used, and the bother score were significantly improved postoperatively in this subpopulation. Preoperatively, all patients used pads, and the average daily number was 2.2 (median; range 0 to 6). Postoperatively, the number of pads used decreased significantly to 0.9 (median; range 0 to 3) pads a day (p=0.002). Urodynamic parameters including bladder capacity, compliance, involuntary detrusor contraction, and bladder neck incompetence proven by FUDS were also significantly improved.
CONCLUSIONS
Our study demonstrated that both objective urodynamic parameters and subjective incontinence symptoms improved significantly after the completion of AC as a single procedure in patients with sphincteric incompetence. This implies that anti-incontinence bladder outlet surgery does not have to be performed simultaneously and can be considered later as a staged operation.
Keyword
MeSH Terms
Figure
Reference
-
1. Stein R, Wiesner C, Beetz R, Pfitzenmeier J, Schwarz M, Thuroff JW. Urinary diversion in children and adolescents with neurogenic bladder: the Mainz experience. Part II: Continent cutaneous diversion using the Mainz pouch I. Pediatr Nephrol. 2005. 20:926–931.2. Chartier-Kastler E, Genevois S, Game X, Denys P, Richard F, Leriche A, et al. Treatment of neurogenic male urinary incontinence related to intrinsic sphincter insufficiency with an artificial urinary sphincter: a French retrospective multicentre study. BJU Int. 2011. 107:426–432.3. Dave S, Salle JL. Current status of bladder neck reconstruction. Curr Opin Urol. 2008. 18:419–424.4. Avery K, Donovan J, Peters TJ, Shaw C, Gotoh M, Abrams P. ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn. 2004. 23:322–330.5. Fleischmann N, Flisser AJ, Blaivas JG, Panagopoulos G. Sphincteric urinary incontinence: relationship of vesical leak point pressure, urethral mobility and severity of incontinence. J Urol. 2003. 169:999–1002.6. Cho SY, Oh SJ. The clinical significance of rectal contractions that occur during urodynamic studies. Neurourol Urodyn. 2010. 29:418–423.7. Medel R, Ruarte AC, Herrera M, Castera R, Podesta ML. Urinary continence outcome after augmentation ileocystoplasty as a single surgical procedure in patients with myelodysplasia. J Urol. 2002. 168(4 Pt 2):1849–1852.8. Borjeson MC, Lagergren J. Life conditions of adolescents with myelomeningocele. Dev Med Child Neurol. 1990. 32:698–706.9. Kaufman AM, Ritchey ML, Roberts AC, Rudy DC, McGuire EJ. Decreased bladder compliance in patients with myelomeningocele treated with radiological observation. J Urol. 1996. 156:2031–2033.10. Herschorn S, Hewitt RJ. Patient perspective of long-term outcome of augmentation cystoplasty for neurogenic bladder. Urology. 1998. 52:672–678.11. Daher P, Zeidan S, Riachy E, Iskandarani F. Bladder augmentation and/or continent urinary diversion: 10-year experience. Eur J Pediatr Surg. 2007. 17:119–123.12. Quek ML, Ginsberg DA. Long-term urodynamics followup of bladder augmentation for neurogenic bladder. J Urol. 2003. 169:195–198.13. Venn SN, Mundy AR. Long-term results of augmentation cystoplasty. Eur Urol. 1998. 34:Suppl 1. 40–42.14. Siracusano S, Ciciliato S, Benedetto PD, Marega D, Tiberio A, Stacul F. An unusual use of AMS 800 artificial urinary sphincter cuff in the treatment of sphincteric neurogenic incontinence: case report. Spinal Cord. 2004. 42:652–654.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Augmentation cystoplasty in neurogenic bladder
- Surgical Management of Contracted Bladder Due to Tuberculosis
- An Experience of Spastic Neurogenic Bladder Treated with Augmentation Cystoplasty and External Urethral Sphincterotomy
- The Clinical Experience of the Bladder Augmentation with Goodwin's Ileal Cup-patched Bladder
- Antirefluxing Augmentation Cystoplasty with Ileocolic Pouch in Single Kidney with Refluxing Contracted Bladder