Prog Med Phys.
2014 Dec;25(4):233-241. 10.14316/pmp.2014.25.4.233.
Development of Quality Assurance Software for PRESAGE(REU) Gel Dosimetry
- Affiliations
-
- 1Department of Radiation Oncology, Boramae Hospital, Seoul, Korea.
- 2Department of Radiation Oncology, Seoul National University Hospital, Seoul, Korea.
- 3Program in Biomedical Radiation Sciences, Department of Transdisciplinary Studies, Graduate School of Convergence Science and Technology, Seoul National University, Seoul, Korea. wuhg@snu.ac.kr
- KMID: 2315762
- DOI: http://doi.org/10.14316/pmp.2014.25.4.233
Abstract
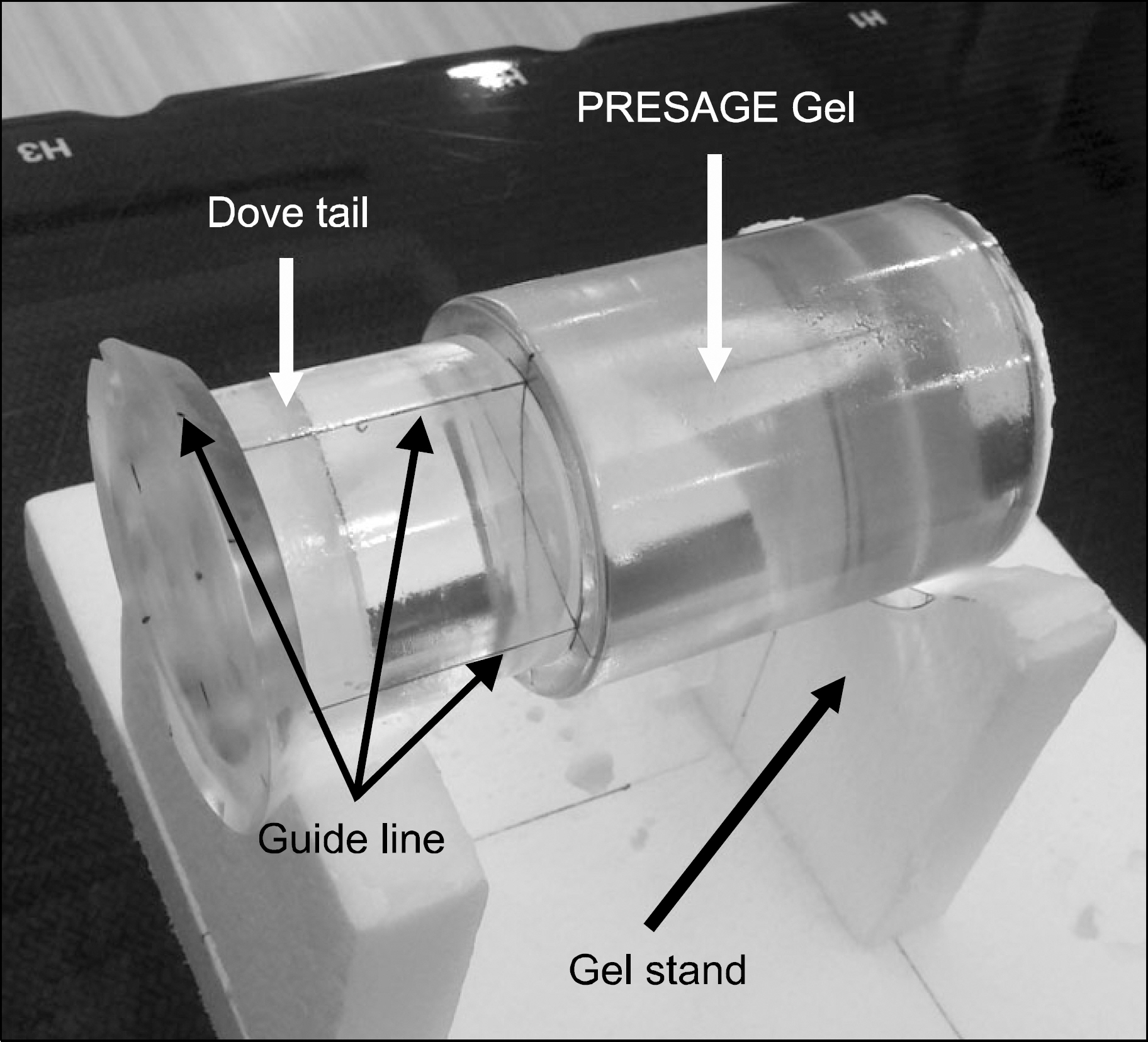
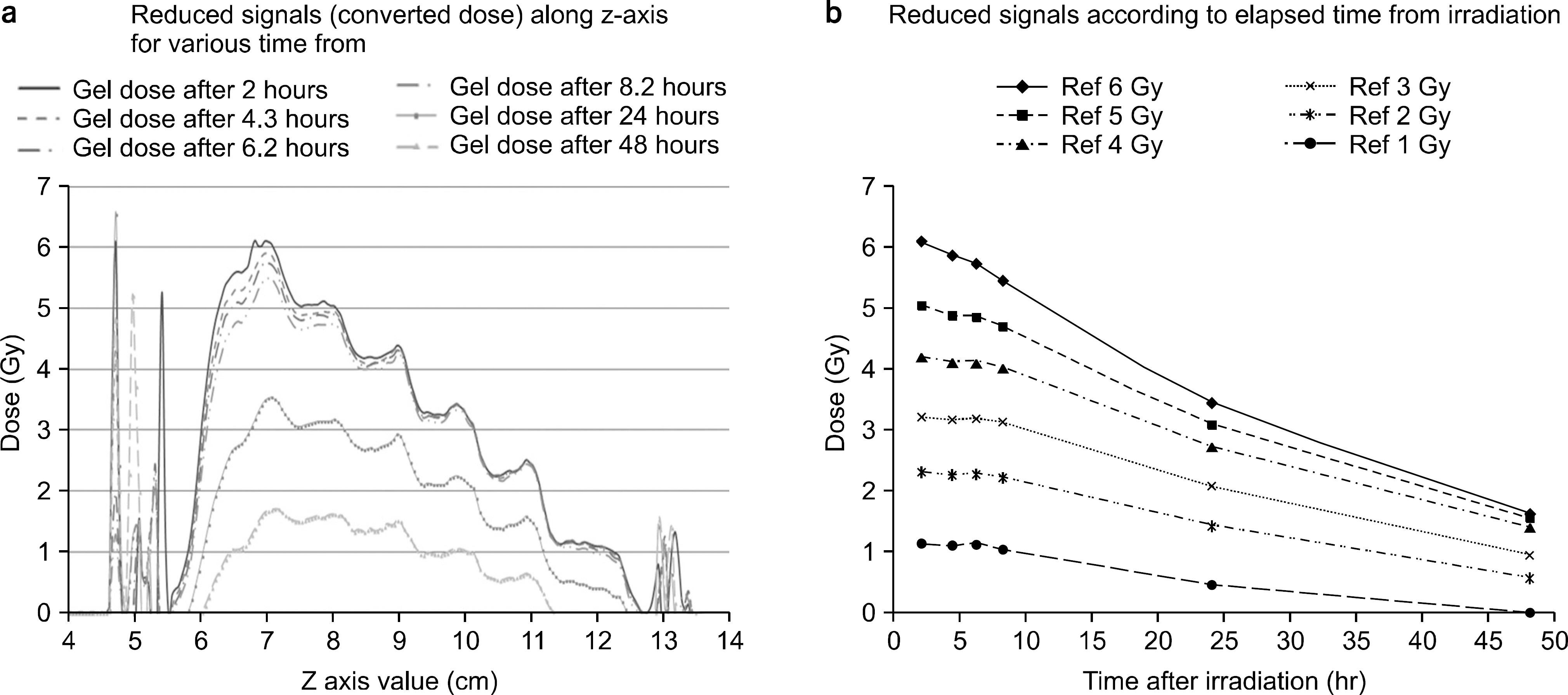
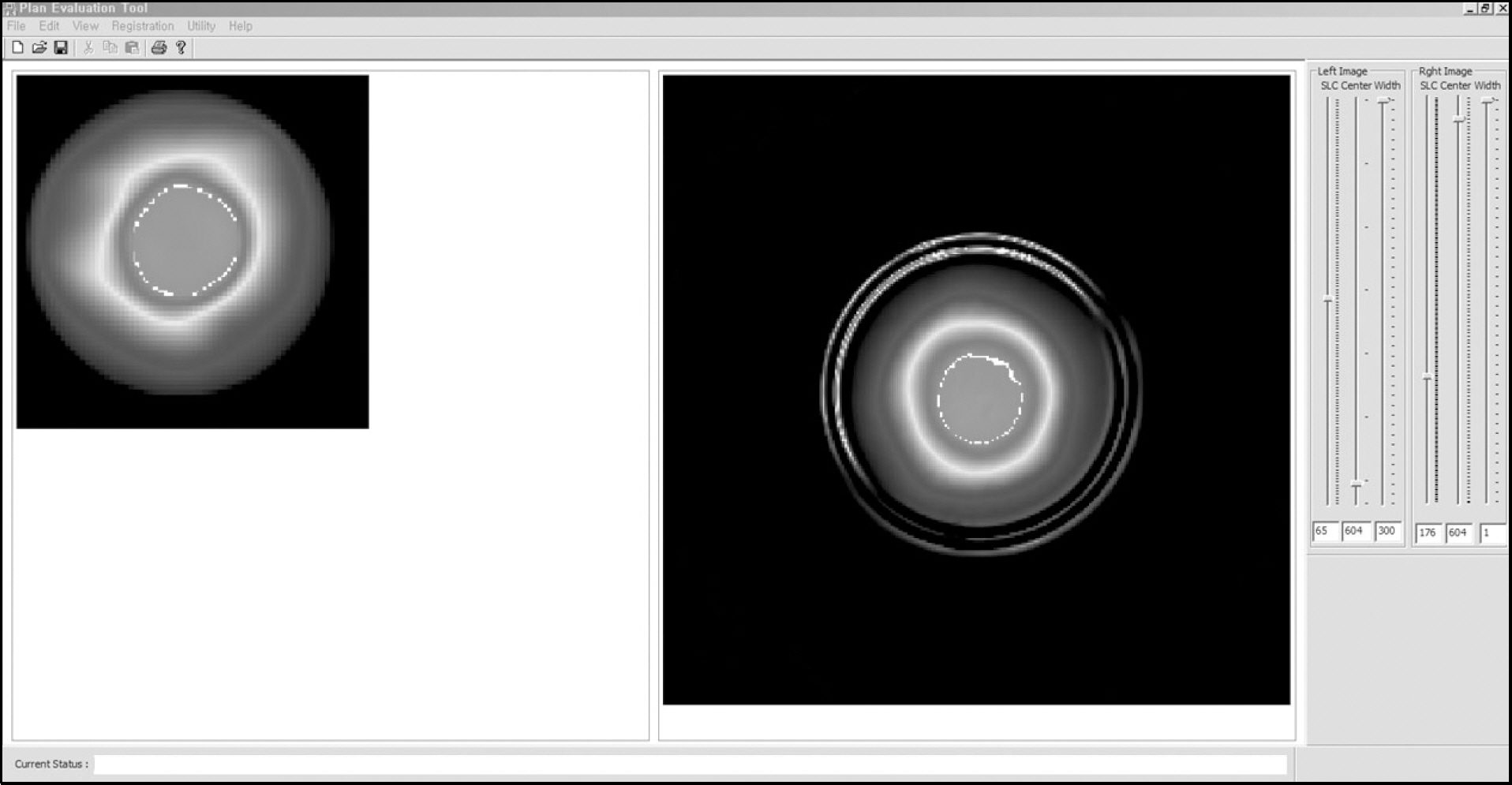
- The aim of this study is to develop a new software tool for 3D dose verification using PRESAGE(REU) Gel dosimeter. The tool included following functions: importing 3D doses from treatment planning systems (TPS), importing 3D optical density (OD), converting ODs to doses, 3D registration between two volumetric data by translational and rotational transformations, and evaluation with 3D gamma index. To acquire correlation between ODs and doses, CT images of a PRESAGE(REU) Gel with cylindrical shape was acquired, and a volumetric modulated arc therapy (VMAT) plan was designed to give radiation doses from 1 Gy to 6 Gy to six disk-shaped virtual targets along z-axis. After the VMAT plan was delivered to the targets, 3D OD data were reconstructed from 512 projection data from Vista(TM) optical CT scanner (Modus Medical Devices Inc, Canada) per every 2 hours after irradiation. A curve for converting ODs to doses was derived by comparing TPS dose profile to OD profile along z-axis, and the 3D OD data were converted to the absorbed doses using the curve. Supra-linearity was observed between doses and ODs, and the ODs were decayed about 60% per 24 hours depending on their magnitudes. Measured doses from the PRESAGE(REU) Gel were well agreed with the TPS doses at central region, but large under-doses were observed at peripheral region at the cylindrical geometry. Gamma passing rate for 3D doses was 70.36% under the gamma criteria of 3% of dose difference and 3 mm of distance to agreement. The low passing rate was resulted from the mismatching of the refractive index between the PRESAGE gel and oil bath in the optical CT scanner. In conclusion, the developed software was useful for 3D dose verification from PRESAGE gel dosimetry, but further improvement of the Gel dosimetry system were required.
Figure
Reference
-
References
1. Fraass B, Doppke K, Hunt M, et al. American Association of Physicists in Medicine Radiation Therapy Committee Task Group 53: Quality assurance for clinical radiotherapy treatment planning. Med. Phys. 25(10):1773–1829. 1998.
Article2. Schreibmann E, Dhabaan A, Elder E, Fox T. Patientspecific quality assurance method for VMAT treatment delivery. Med. Phys. 36(10):4530–4535. 2009.
Article3. Zhen H, Benjamin EN, Wolfgang A, Tomé: Moving from gamma passing rates to patient DVH-based QA metrics in pretreatment dose QA. Med. Phys. 38(10):5477–5489. 2011.4. Benjamin EN, Zhen H, Wolfgang A, Tomé: Per-beam, planar IMRT QA passing rates do not predict clinically relevant patient dose errors. Med. Phys. 38(2):1037–1044. 2011.5. Wu C, Kelly E. Hosier, Kristen E. Beck, et al: On using 3D γ-analysis for IMRT and VMAT pretreatment plan QA. Med. Phys. 39(6):3051–3059. 2012.6. Carrasco P, Jornet N, Latorre A, Eudaldo T, Ruiz A, Ribas M. 3D DVH-based metric analysis versus per-beam planar analysis in IMRT pretreatment verification. Med. Phys. 39(8):5040–5049. 2012.
Article7. Visser R, Wauben DJL, Groot M, et al. Efficient and reliable 3D dose quality assurance for IMRT by combining independent dose calculations with measurements. Med. Phys. 40(2):021710–1. -6 (. 2013.
Article8. Fredh A, Scherman JB, Fog LS, Rosenschöld PM. Patient QA systems for rotational radiation therapy: A comparative experimental study with intentional errors. Med. Phys. 40:031716. 2013.
Article9. Juang T, Newton J, Niebanck M, Benning R, Adamovics J, Oldham M. Customising PRESAGE® for diverse applications. Journal of Physics: Conference Series. 444:1–5. 2013.10. Qian X, Adamovics J, Wuu C. Performance of an improved first generation optical CT scanner for 3D dosimetry. Phys. Med. Biol. 58:N321–N331. 2013.11. Juang T, Grant R, Adamovics J, Ibbott G, Oldham M. On the feasibility of comprehensive high-resolution 3D remote dosimetry. Med. Phys. 41(7):071706–1. -11 (. 2014.
Article12. Cho SJ, Chung YL, Lee SH, et al. A Study of Optimized MRI Parameters for Polymer Gel Dosimetry, Korean J Med Phys. 23(2):71–80. 2012.13. Jang JS, Kwon SI. 3-Dimensional Dosimetry of Small Field Photon Beam, Korean J Med Phys. 23(1):54–61. 2012.14. Lee KN, Lee DJ, Suh TS. 3-Dimensional Verification Technique for Target Point Error, Korean J Med Phys. 22(1):35–41. 2011.15. Jung JY, Lee CI, Min JH, Kim YL, Lee SY, Suh TS. A Study on Dose Response of MAGAT (Methacrylic Acid, Gelatin Gel and THPC) Polymer Gel Dosimeter Using X-ray CT Scanner. Korean J Med Phys. 21(1):1–8. 2010.16. Lopatiuk-Tirpak O, Langen KM, Meeks SL, Kupelian PA, Zeidan OA, Maryanski MJ. Performance evaluation of an improved optical computed tomography polymer gel dosimeter system for 3D dose verification of static and dynamic phantom deliveries, Med. Phys. 35(9):3847–3859. 2008.17. Jirasek A. Experimental investigations of polymer gel dosimeters, Journal of Physics: Conference Series. 56:23–34. 2006.18. Jordan K. Review of recent advances in radiochromic materials for 3D dosimetry, Journal of Physics: Conference Series. 250:1–7. 2010.19. Pierquet M, Thomas A, Adamovics J, Oldham M. An investigation into a new re-useable 3D radiochromic dosimetry material, PresageREU, Journal of Physics: Conference Series. 250:1–4. 2010.20. Adamovics J, Maryanski MJ. CHARACTERISATION OF PRESAGETM: A NEW 3-D RADIOCHROMIC SOLID POLYMER DOSEMETER FOR IONISING RADIATION, Radiation Protection Dosimetry, 120 (1–4):. 107–112. (. 2006.21. Doran SJ, Krstajic N, Adamovics J, Jenneson PM. Optical CT scanning of PRESAGETM polyurethane samples with a CCD-based readout system, Journal of Physics: Conference Series. 3:240–243. 2004.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Comparison between Portal Dosimetry and Mobius3D Results for Patient-Specific Quality Assurance in Radiotherapy
- Three-Dimensional Dosimetry Using Magnetic Resonance Imaging of Polymer Gel
- Clinical performance of FractionLab in patient-specific quality assurance for intensity-modulated radiotherapy: a retrospective study
- Development of Preliminary Quality Assurance Software for GafChromic(R) EBT2 Film Dosimetry
- Development of an Analytic Software Using Pencil Beam Scanning Proton Beam