Korean J Urol.
2011 Jan;52(1):31-38.
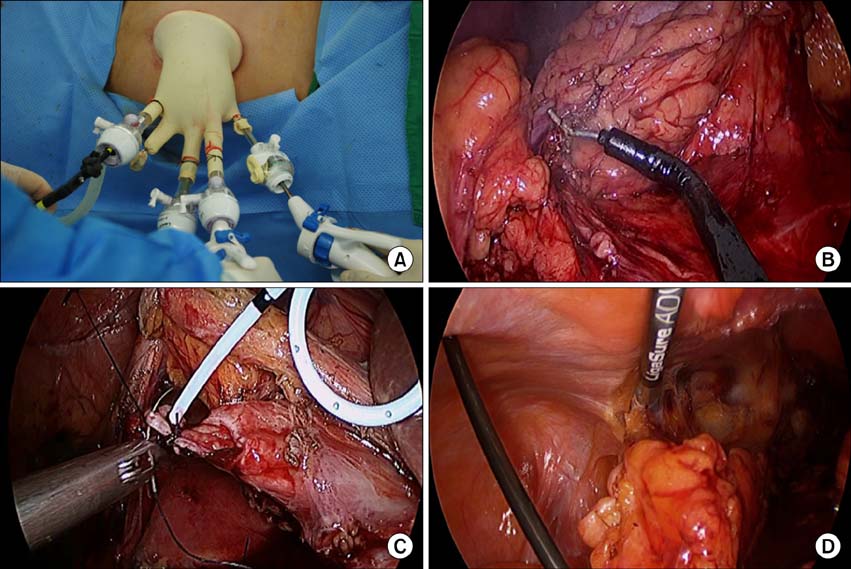
Laparoendoscopic Single-Site Surgeries: A Single-Center Experience of 171 Consecutive Cases
- Affiliations
-
- 1Department of Urology, Urological Science Institute, Yonsei University College of Medicine, Seoul, Korea. hanwk@yuhs.ac
- 2Department of Urology, CHA Bundang Medical Center, CHA University, Seongnam, Korea.
Abstract
- PURPOSE
We report our experience to date with 171 patients who underwent laparoendoscopic single-site surgery for diverse urologic diseases in a single institution.
MATERIALS AND METHODS
Between December 2008 and August 2010, we performed 171 consecutive laparoendoscopic single-site surgeries. These included simple nephrectomy (n=18; robotic surgeries, n=1), radical nephrectomy (n=26; robotic surgeries, n=2), partial nephrectomy (n=59; robotic surgeries, n=56), nephroureterectomy (n=20; robotic surgeries, n=12), pyeloplasty (n=4), renal cyst decortications (n=22), adrenalectomy (n=4; robotic surgeries, n=2), ureterolithotomy (n=10), partial cystectomy (n=3), ureterectomy (n=1), urachal mass excision (n=1), orchiectomy (n=1), seminal vesiculectomy (n=1), and retroperitoneal mass excision (n=1). All procedures were performed by use of a homemade single-port device with a wound retractor and surgical gloves. A prospective study was performed to evaluate outcomes in 171 cases.
RESULTS
Of the 171 patients, 98 underwent conventional laparoendoscopic single-site surgery and 73 underwent robotic laparoendoscopic single-site surgery. Mean patient age was 53 years, mean operative time was 190.8 minutes, and mean estimated blood loss was 204 ml. Intraoperative complications occurred in seven cases (4.1%), and postoperative complications in nine cases (5.3%). There were no complications classified as Grade IIIb or higher (Clavien-Dindo classification for surgical complications). Conversion to mini-incision open surgery occurred in seven (4.1%) cases. Regarding oncologic outcomes, no cancer-related events occurred during follow-up other than one aggressive progression of Ewing sarcoma.
CONCLUSIONS
Laparoendoscopic single-site surgery is technically feasible and safe for various urologic diseases; however, surgical experience and long-term follow-up are needed to test the superiority of laparoendoscopic single-site surgery.
MeSH Terms
Figure
Reference
-
1. Raman JD, Bensalah K, Bagrodia A, Stern JM, Cadeddu JA. Laboratory and clinical development of single keyhole umbilical nephrectomy. Urology. 2007. 70:1039–1042.2. White WM, Haber GP, Goel RK, Crouzet S, Stein RJ, Kaouk JH. Single-port urological surgery: single-center experience with the first 100 cases. Urology. 2009. 74:801–804.3. Jeon HG, Jeong W, Oh CK, Lorenzo EI, Ham WS, Rha KH, et al. Initial experience with 50 laparoendoscopic single site surgeries using a homemade, single port device at a single center. J Urol. 2010. 183:1866–1871.4. Desai MM, Berger AK, Brandina R, Aron M, Irwin BH, Canes D, et al. Laparoendoscopic single-site surgery: initial hundred patients. Urology. 2009. 74:805–812.5. Gill IS, Canes D, Aron M, Haber GP, Goldfarb DA, Flechner S, et al. Single port transumbilical (E-NOTES) donor nephrectomy. J Urol. 2008. 180:637–641.6. Seo IY, Hong HM, Kang IS, Lee JW, Rim JS. Early experience of laparoendoscopic single-site nephroureterectomy for upper urinary tract tumors. Korean J Urol. 2010. 51:472–476.7. Kim TH, Jeong BC, Seo SI, Jeon SS, Han DH. Transumbilical laparoendoscopic single-site ureterolithotomy for large impacted ureteral stones: initial experiences. Korean J Urol. 2010. 51:403–408.8. Park YH, Kang MY, Jeong MS, Choi H, Kim HH. Laparoendoscopic single-site nephrectomy using a homemade single-port device for single-system ectopic ureter in a child: initial case report. J Endourol. 2009. 23:833–835.9. Jeon HG, Kim DS, Jeoung HB, Han SW, Hong CH, Im YJ, et al. Pediatric laparoendoscopic single-site partial nephrectomy: initial report. Urology. 2010. 76:138–141.10. Marietti S, DeCambre M, Fairbanks T, Kling K, Chiang G. Early experience with laparoendoscopic single-site surgery in the pediatric urology patient population. J Endourol. 2010. 24:1321–1324.11. Kaouk JH, Goel RK, Haber GP, Crouzet S, Stein RJ. Robotic single-port transumbilical surgery in humans: initial report. BJU Int. 2009. 103:366–369.12. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009. 250:187–196.13. Han WK, Kim DS, Jeon HG, Jeong W, Oh CK, Choi KH, et al. Robot-assisted laparoendoscopic single-site surgery: partial nephrectomy for renal malignancy. Urology. 2010. Epub ahead of print.14. Autorino R, Stein RJ, Lima E, Damiano R, Khanna R, Haber GP, et al. Current status and future perspectives in laparoendoscopic single-site and natural orifice transluminal endoscopic urological surgery. Int J Urol. 2010. 17:410–431.15. Desai MM, Rao PP, Aron M, Pascal-Haber G, Desai MR, Mishra S, et al. Scarless single port transumbilical nephrectomy and pyeloplasty: first clinical report. BJU Int. 2008. 101:83–88.16. Raybourn JH 3rd, Rane A, Sundaram CP. Laparoendoscopic single-site surgery for nephrectomy as a feasible alternative to traditional laparoscopy. Urology. 2010. 75:100–103.17. Stolzenburg JU, Kallidonis P, Hellawell G, Do M, Haefner T, Dietel A, et al. Technique of laparoscopic-endoscopic single-site surgery radical nephrectomy. Eur Urol. 2009. 56:644–650.18. Aron M, Canes D, Desai MM, Haber GP, Kaouk JH, Gill IS. Transumbilical single-port laparoscopic partial nephrectomy. BJU Int. 2009. 103:516–521.19. Kaouk JH, Goel RK. Single-port laparoscopic and robotic partial nephrectomy. Eur Urol. 2009. 55:1163–1169.20. Tracy CR, Raman JD, Bagrodia A, Cadeddu JA. Perioperative outcomes in patients undergoing conventional laparoscopic versus laparoendoscopic single-site pyeloplasty. Urology. 2009. 74:1029–1034.21. Ryu DS, Park WJ, Oh TH. Retroperitoneal laparoendoscopic single-site surgery in urology: initial experience. J Endourol. 2009. 23:1857–1862.22. Jeong BC, Park YH, Han DH, Kim HH. Laparoendoscopic single-site and conventional laparoscopic adrenalectomy: a matched case-control study. J Endourol. 2009. 23:1957–1960.23. Park YH, Park SY, Kim HH. Laparoendoscopic single-site nephroureterectomy with bladder cuff excision for upper urinary tract transitional-cell carcinoma: technical details based on oncologic principles. J Endourol. 2010. 24:563–566.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hybrid laparoscopic myomectomy: A novel technique
- Robot-assisted laparoendoscopic single-site upper urinary tract surgery with da Vinci Xi surgical system: Initial experience
- Initial Experience with Laparoendoscopic Single-Site Surgery by Use of a Homemade Transumbilical Port in Urology
- Concomitant Laparoendoscopic Single-Site Surgery for Vesicolithotomy and Finger-Assisted Single-Port Transvesical Enucleation of the Prostate
- Laparoendoscopic single-site radical hysterectomy for early stage cervical cancer