Korean J Urol.
2011 Apr;52(4):274-278.
Efficacy and Safety of Low-Dose Propiverine in Patients with Lower Urinary Tract Symptoms/Benign Prostatic Hyperplasia with Storage Symptoms: A Prospective, Randomized, Single-Blinded and Multicenter Clinical Trial
- Affiliations
-
- 1Department of Urology, Korea University Medical Center and Korea University Institute of Regenerative Medicine, Seoul, Korea.
- 2Department of Urology, Chonnam National University Medical School, Gwangju, Korea.
- 3Department of Urology, Kyungpook National University, Daegu, Korea.
- 4Department of Urology, Ulsan University Hospital, Ulsan, Korea.
- 5Department of Urology, Dankook University College of Medicine, Cheonan, Korea. killtumor@yahoo.co.kr
Abstract
- PURPOSE
The aim of this study was to evaluate whether low-dose anticholinergics combined with an alpha1-receptor antagonist would continue the effect of an alpha-blocker, decrease the side effects of anticholinergics, and improve the symptoms of lower urinary tract symptoms/benign prostatic hyperplasia (LUTS/BPH).
MATERIALS AND METHODS
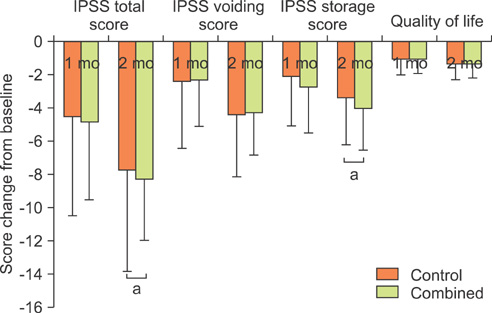
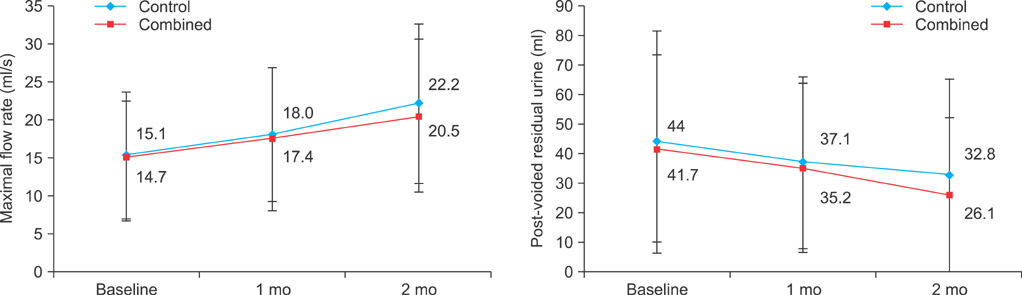
Two hundred nine men with LUTS/BPH with storage symptoms (International Prostate Symptom Score [IPSS] > or =12; storage symptoms > or =4) were randomly assigned in a prospective, multicentered, and single-blind fashion to either the control group (alfuzosin 10 mg, once daily) or the combined group (alfuzosin 10 mg, once daily, and propiverine 10 mg, once daily) for 2 months. IPSS, maximal urinary flow rate (Qmax), and postvoid residual volume (PVR) were used to grade symptoms, side effects, and the impact on quality of life (QoL) at the start of the study and after 1 and 2 months.
RESULTS
There were no significant differences in patient background, including age, prostate size, Qmax, and PVR, between the control group and the combined group. In the combined group, the IPSS total score and the IPSS storage symptom score were significantly improved compared with the control group. The IPSS voiding symptom score, QoL, Qmax, and PVR did not differ significantly. There were no serious side effects in either group.
CONCLUSIONS
Management with an alpha1-receptor antagonist combined with a low-dose anticholinergic improved the total score and storage symptom score of the IPSS compared with alpha1-receptor antagonist only group without causing serious side effects. This initial combination medication can be considered an effective and safe treatment modality for LUTS/BPH patients with storage symptoms.
MeSH Terms
Figure
Reference
-
1. Chapple CR, Smith D. The pathophysiological changes in the bladder obstructed by benign prostatic hyperplasia. Br J Urol. 1994. 73:117–123.2. Park HK, Park H, Cho SY, Bae J, Jeong SJ, Hong SK, et al. The prevalence of benign prostatic hyperplasia in elderly men in Korea: a community-based study. Korean J Urol. 2009. 50:843–847.3. Milsom I, Abrams P, Cardozo L, Roberts RG, Thüroff J, Wein AJ. How widespread are the symptoms of an overactive bladder and how are they managed? A population-based prevalence study. BJU Int. 2001. 87:760–766.4. Kim HW, Seo SI, Ko JS, Jung JH, Lee JY. Incidence of overactive bladder in benign prostatic hyperplasia and the efficacy of combination therapy of alpha blocker with tolterodine. Korean J Urol. 2003. 44:1006–1010.5. Abrams PH, Farrar DJ, Turner-Warwick RT, Whiteside CG, Feneley RC. The results of prostatectomy: a symptomatic and urodynamic analysis of 152 patients. J Urol. 1979. 121:640–642.6. Kakizaki H, Machino R, Koyanagi T. Clinical experience in lower urinary tract symptoms. BJU Int. 2001. 88:Suppl 2. 23–26.7. Seaman EK, Jacobs BZ, Blaivas JG, Kaplan SA. Persistence or recurrence of symptoms after transurethral resection of the prostate: a urodynamic assessment. J Urol. 1994. 152:935–937.8. Engström G, Henningsohn L, Walker-Engström ML, Leppert J. Impact on quality of life of different lower urinary tract symptoms in men measured by means of the SF 36 questionnaire. Scand J Urol Nephrol. 2006. 40:485–494.9. Sountoulides P, van Dijk MM, Wijkstra H, de la Rosette JJ, Michel MC. Role of voiding and storage symptoms for the quality of life before and after treatment in men with voiding dysfunction. World J Urol. 2010. 28:3–8.10. Chapple CR, Rechberger T, Al-Shukri S, Meffan P, Everaert K, Huang M, et al. Randomized, double-blind placebo- and tolterodine-controlled trial of the once-daily antimuscarinic agent solifenacin in patients with symptomatic overactive bladder. BJU Int. 2004. 93:303–310.11. Otsuka A, Shinbo H, Hasebe K, Matsumoto R, Ozono S. Effects of a novel beta(3)-adrenoceptor agonist, AJ-9677, on relaxation of the detrusor muscle: an in vitro study. Int J Urol. 2008. 15:1072–1076.12. Zagorodnyuk VP, Brookes SJ, Spencer NJ, Gregory S. Mechanotransduction and chemosensitivity of two major classes of bladder afferents with endings in the vicinity to the urothelium. J Physiol. 2009. 587:3523–3538.13. Jang J, Park EY, Seo SI, Hwang TK, Kim JC. Effects of intravesical instillation of cyclooxygenase-2 inhibitor on the expression of inducible nitric oxide synthase and nerve growth factor in cyclophosphamide-induced overactive bladder. BJU Int. 2006. 98:435–439.14. Abrams P, Kaplan S, De Koning Gans HJ, Millard R. Safety and tolerability of tolterodine for the treatment of overactive bladder in men with bladder outlet obstruction. J Urol. 2006. 175:999–1004.15. Kaplan SA, Roehrborn CG, Rovner ES, Carlsson M, Bavendam T, Guan Z. Tolterodine and tamsulosin for treatment of men with lower urinary tract symptoms and overactive bladder: a randomized controlled trial. JAMA. 2006. 296:2319–2328.16. Lee KS, Choo MS, Kim DY, Kim JC, Kim HJ, Min KS, et al. Combination treatment with propiverine hydrochloride plus doxazosin controlled release gastrointestinal therapeutic system formulation for overactive bladder and coexisting benign prostatic obstruction: a prospective, randomized, controlled multicenter study. J Urol. 2005. 174:1334–1338.17. Staskin DR, Rosenberg MT, Dahl NV, Polishuk PV, Zinner NR. Effects of oxybutynin transdermal system on health-related quality of life and safety in men with overactive bladder and prostate conditions. Int J Clin Pract. 2008. 62:27–38.18. Irani J. Anticholinergic drugs in patients with bladder outlet obstruction and lower urinary tract symptoms: Where do we stand in 2006? Eur Urol. 2006. 50:653–654.19. Novara G, Galfano A, Ficarra V, Artibani W. Anticholinergic drugs in patients with bladder outlet obstruction and lower urinary tract symptoms: a systematic review. Eur Urol. 2006. 50:675–683.20. Rackley R, Weiss JP, Rovner ES, Wang JT, Guan Z. Nighttime dosing with tolterodine reduces overactive bladder-related nocturnal micturitions in patients with overactive bladder and nocturia. Urology. 2006. 67:731–736.21. Feinberg M. The problems of anticholinergic adverse effects in older patients. Drugs Aging. 1993. 3:335–348.22. Hong WS, Chung H, Lee JM, Kim TW, Kim HS, Kim HJ, et al. Polypharmacy and central nervous system adverse effects of anticholinergic agents in the men with benign prostate hyperplasia. J Korean Continence Soc. 2007. 11:24–29.23. Abrams P, Freeman R, Anderström C, Mattiasson A. Tolterodine, a new antimuscarinic agent: as effective but better tolerated than oxybutynin in patients with an overactive bladder. Br J Urol. 1998. 81:801–810.24. Kelleher CJ, Cardozo LD, Khullar V, Salvatore S. A medium-term analysis of the subjective efficacy of treatment for women with detrusor instability and low bladder compliance. Br J Obstet Gynaecol. 1997. 104:988–993.25. Milsom I, Abrams P, Cardozo L, Roberts RG, Thüroff J, Wein AJ. How widespread are the symptoms of an overactive bladder and how are they managed? A population-based prevalence study. BJU Int. 2001. 87:760–766.26. Versi E, Appell R, Mobley D, Patton W, Saltzstein D. The Ditropan XL Study Group. Dry mouth with conventional and controlled-release oxybutynin in urinary incontinence. Obstet Gynecol. 2000. 95:718–721.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Efficacy and Safety of Combination Therapy with Alpha-Blocker and Low-Dose Propiverine Hydrochloride for Benign Prostatic Hyperplasia Accompanied by Overactive Bladder Symptoms
- Current Trend of the Primary Treatment in Lower Urinary Tract Symptom/Benign Prostatic Hyperplasia
- Efficacy of Propiverine for Chronic Prostatitis / Chronic Pelvic Pain Syndrome
- Effect of Transurethral Resection of the Prostate on Storage Symptoms in Patients with Benign Prostatic Hyperplasia of Less than 30 ml
- The Urinary Tract Microbiome in Male Genitourinary Diseases: Focusing on Benign Prostate Hyperplasia and Lower Urinary Tract Symptoms