Pediatr Gastroenterol Hepatol Nutr.
2012 Dec;15(4):210-219.
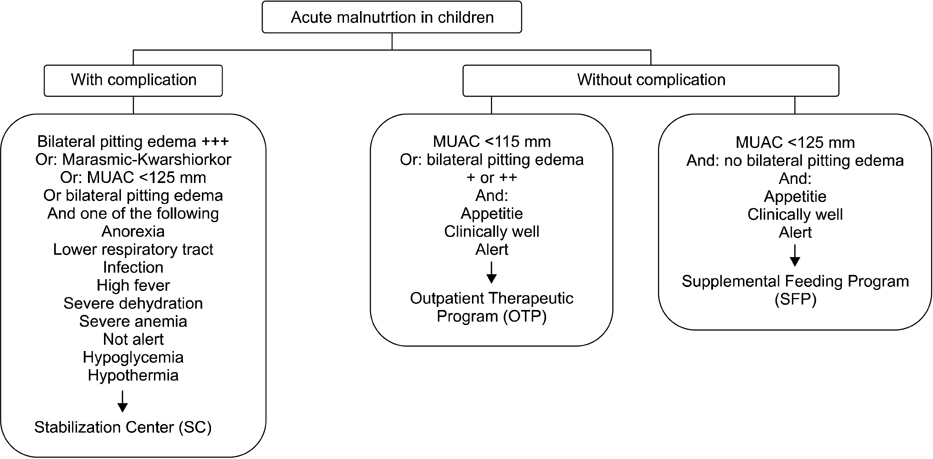
Community Management of Acute Malnutrition in the Developing World
- Affiliations
-
- 1World Vision Korea, Seoul, Korea.
- 2World Vision Eastern Africa Regional Office, Nairobi, Kenya.
- 3The International Vaccine Institute, Seoul, Korea. nsbeck@ivi.int
Abstract
- Globally, acute malnutrition triggers more than 50% of childhood mortality in children under 5 years old, which implies that about 3.5 million children die of malnutrition each year. Prior to the advent of ready-to-use therapeutic food (RUTF), the management of acute malnutrition was limited to hospitals, resulting in low coverage rates with high mortality, as malnourished cases were indentified at later stages often plagued with complications. However, current availability of RUTF has enabled malnourished children to be treated at communities. Further, because RUTF is dehydrated and sealed, it has the added advantage of a lower risk of bacterial contamination, thereby prolonging its storage life at room temperature. Recent data indicate that Community Management of Acute Malnutrition (CMAM) is as cost effective as other high-impact public health measures such as oral rehydration therapy for acute diarrheal diseases, vitamin A supplementation, and antibiotic treatment for acute respiratory infections. Despite the high efficacy of CMAM programs, CMAM still draws insufficient attention for global implementation, suggesting that CMAM programs should be integrated into local or regional routine health systems. Knowledge gaps requiring further research include: the definition of practical screening criteria for malnourished children at communities, the need for systematic antibiotic therapy during malnutrition treatment, and the dietary management of severe malnutrition in children below 6 months of age.
Keyword
MeSH Terms
Figure
Reference
-
1. UNICEF-WHO-The World Bank Joint Child Malnutrition, Levels & Trends in Child Malnutrition. 2012. Accessed on Nov 10, 2012. Available at http://www.who.int/nutgrowthdb/jme_unicef_who_wb.pdf.2. Caulfield LE, de Onis M, Blössner M, Black RE. Undernutrition as an underlying cause of child deaths associated with diarrhea, pneumonia, malaria, and measles. Am J Clin Nutr. 2004. 80:193–198.
Article3. Collins S, Sadler K, Dent N, Khara T, Guerrero S, Myatt M, et al. Key issues in the success of community-based management of severe malnutrition. Food Nutr Bull. 2006. 27:3 Suppl. S49–S82.
Article4. Black RE, Allen LH, Bhutta ZA, Caulfield LE, de Onis M, Ezzati M, et al. Maternal and Child Undernutrition Study Group. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008. 371:243–260.
Article5. Mason JB, Musgrove P, Habicht JP. At least one-third of poor countries' disease burden is due to malnutrition. Disease Control Priorities Project (DCPP) Working Paper No. 1. 2003. 03. Accessed on Nov 10, 2012. Fogarty International Center of the National Institutes of Health;Available at: http://www.dcp2.org/file/17/wp1.pdf.6. Bryce J, Coitinho D, Darnton-Hill I, Pelletier D, Pinstrup-Andersen P. Maternal and Child Undernutrition Study Group. Maternal and child undernutrition: effective action at national level. Lancet. 2008. 371:510–526.
Article7. Nassar MF, Younis NT, Tohamy AG, Dalam DM, El Badawy MA. T-lymphocyte subsets and thymic size in malnourished infants in Egypt: a hospital-based study. East Mediterr Health J. 2007. 13:1031–1042.
Article8. Salimonu LS, Johnson AO, Williams AI, Adeleye GI, Osunkoya BO. Lymphocyte subpopulations and antibody levels in immunized malnourished children. Br J Nutr. 1982. 48:7–14.
Article9. Savy M, Edmond K, Fine PE, Hall A, Hennig BJ, Moore SE, et al. Landscape analysis of interactions between nutrition and vaccine responses in children. J Nutr. 2009. 139:2154S–2218S.
Article10. Hafez M, Aref GH, Mehareb SW, Kassem AS, El-Tahhan H, Rizk Z, et al. Antibody production and complement system in protein energy malnutrition. J Trop Med Hyg. 1977. 80:36–39.11. Vesikari T, Itzler R, Matson DO, Santosham M, Christie CD, Coia M, et al. Efficacy of a pentavalent rotavirus vaccine in reducing rotavirus-associated health care utilization across three regions (11 countries). Int J Infect Dis. 2007. 11:Suppl 2. S29–S35.
Article12. Greenwood BM, Bradley-Moore AM, Bradley AK, Kirkwood BR, Gilles HM. The immune response to vaccination in undernourished and well-nourished Nigerian children. Ann Trop Med Parasitol. 1986. 80:537–544.
Article13. Chopra K, Kundu S, Chowdhury DS. Antibody response of infants in tropics to five doses of oral polio vaccine. J Trop Pediatr. 1989. 35:19–23.
Article14. Chandra RK. Reduced secretory antibody response to live attenuated measles and poliovirus vaccines in malnourished children. Br Med J. 1975. 2:583–585.
Article15. Vesikari T, Matson DO, Dennehy P, Van Damme P, Santosham M, Rodriguez Z, et al. Rotavirus Efficacy and Safety Trial (REST) Study Team. Safety and efficacy of a pentavalent human-bovine (WC3) reassortant rotavirus vaccine. N Engl J Med. 2006. 354:23–33.
Article16. Ciarlet M, Schödel F. Development of a rotavirus vaccine: clinical safety, immunogenicity, and efficacy of the pentavalent rotavirus vaccine, RotaTeq. Vaccine. 2009. 27:Suppl 6. G72–G81.
Article17. Block SL, Vesikari T, Goveia MG, Rivers SB, Adeyi BA, Dallas MJ, et al. Pentavalent Rotavirus Vaccine Dose Confirmation Efficacy Study Group. Efficacy, immunogenicity, and safety of a pentavalent human-bovine (WC3) reassortant rotavirus vaccine at the end of shelf life. Pediatrics. 2007. 119:11–18.
Article18. WHO Child Growth Standards and the Identification of Severe Acute Malnutrition in Infants and Children. A Joint Statement by the World Health Organization and the United Nations Children's Fund. 2009. Accessed on Nov 5, 2012. Available at: http://www.who.int/nutrition/publications/severemalnutrition/9789241598163_eng.pdf.19. Mason JB, Hay RW, Leresche J, Peel S, Darley S. Treatment of severe malnutrition in relief. Lancet. 1974. 1:332–335.
Article20. WHO. Management of severe malnutrition: a manual for physicians and other senior health workers. 1999. Accessed on Nov 18, 2012. Geneva: World Health Organization;Available at: http://whqlibdoc.who.int/hq/1999/a57361.pdf.21. Tomkins A, Watson F. Malnutrition and infection. A review. 1989. Accessed on Dec 4, 2012. Geneva: WHO. Advisor committee on coordination/Subcommittee on nutrition;Available at: http://www.unscn.org/layout/modules/resources/files/Policy_paper_No_5.pdf.22. Cunningham-Rundles S. Effects of nutritional status on immunological function. Am J Clin Nutr. 1982. 35:5 Suppl. 1202–1210.
Article23. Golden MH, Briend A. Treatment of malnutrition in refugee camps. Lancet. 1993. 342:360.24. WHO. UNHCR. WFP. IFRC. The management of nutrition in major emergencies. 2000. Accessed on Dec 4, 2012. Geneva: WHO;Availabe at: http://whqlibdoc.who.int/publications/2000/9241545208.pdf.25. Boelaert M, Davis A, Le Lin B, Michelet M, Ritmeijer K, Van Der Kam S, et al. Nutrition guidelines. 1995. 1st. Paris: Medecins sans Frontieres.26. WHO. Improving child health. IMCI: the integrated approach. 1997. Accessed on Dec 4, 2012. Geneva: World Health Organization;Available at: http://whqlibdoc.who.int/hq/1997/WHO_CHD_97.12_Rev.2.pdf.27. Ahmed T, Ali M, Ullah MM, Choudhury IA, Haque ME, Salam MA, et al. Mortality in severely malnourished children with diarrhoea and use of a standardised management protocol. Lancet. 1999. 353:1919–1922.
Article28. Deen JL, Funk M, Guevara VC, Saloojee H, Doe JY, Palmer A, et al. Implementation of WHO guidelines on management of severe malnutrition in hospitals in Africa. Bull World Health Organ. 2003. 81:237–243.29. Prudhon C, Briend A, Laurier D, Golden MH, Mary JY. Comparison of weight- and height-based indices for assessing the risk of death in severely malnourished children. Am J Epidemiol. 1996. 144:116–123.
Article30. WHO. WHO global health atlas-human resources for health. Accessed on Nov 10, 2012. http://apps.who.int/globalatlas/docs/HRH/HTML/SASA_Aug08.htm.31. Cook R. Is hospital the place for the treatment of malnourished children? J Trop Pediatr Environ Child Health. 1971. 17:15–25.
Article32. Bengoa JM. Nutrition rehabilitation centres. J Trop Pediatr. 1967. 13:169–176.
Article33. Ashworth A. Efficacy and effectiveness of community-based treatment of severe malnutrition. Food Nutr Bull. 2006. 27:3 Suppl. S24–S48.
Article34. Briend A. Treatment of severe malnutrition with a therapeutic spread. ENN Field Exchange. 1997. 3:15. Available at: http://fex.ennonline.net/2/treatment. (Accessed on Dec 4, 2012).35. Briend A, Golden MH. Treatment of severe child malnutrition in refugee camps. Eur J Clin Nutr. 1993. 47:750–754.36. Briend A, Lacsala R, Prudhon C, Mounier B, Grellety Y, Golden MH. Ready-to-use therapeutic food for treatment of marasmus. Lancet. 1999. 353:1767–1768.
Article37. Diop el HI, Dossou NI, Ndour MM, Briend A, Wade S. Comparison of the efficacy of a solid ready-to-use food and a liquid, milk-based diet for the rehabilitation of severely malnourished children: a randomized trial. Am J Clin Nutr. 2003. 78:302–307.
Article38. Navarro-Colorado C, Laquière S. Clinical trial of BP100 vs F100 milk for rehabilitation of severe malnutrition. ENN Field Exchange. 2005. 24:22–24. Available at: http://fex.ennonline.net/24/clinical. (Accessed on Nov 11 2012).39. Khara T, Collins S. Community-based Therapeutic Care (CTC). Emergency Nutrition Network (ENN) Special Supplement Series No. 2. 2004. 11. Accessed on Nov 11, 2012. Available at http://www.ennonline.net/pool/files/ife/supplement23.pdf.40. Myatt M, Khara T, Collins S. A review of methods to detect cases of severely malnourished children in the community for their admission into community-based therapeutic care programs. Food Nutr Bull. 2006. 27:3 Suppl. S7–S23.
Article41. Pelletier DL. The relationship between child anthropometry and mortality in developing countries: implications for policy, programs and future research. J Nutr. 1994. 124:10 Suppl. 2047S–2081S.42. Briend A, Dykewicz C, Graven K, Mazumder RN, Wojtyniak B, Bennish M. Usefulness of nutritional indices and classifications in predicting death of malnourished children. Br Med J (Clin Res Ed). 1986. 293:373–375.
Article43. Lapidus N, Luquero FJ, Gaboulaud V, Shepherd S, Grais RF. Prognostic accuracy of WHO growth standards to predict mortality in a large-scale nutritional program in Niger. PLoS Med. 2009. 6:e39.
Article44. English M, Esamai F, Wasunna A, Were F, Ogutu B, Wamae A, et al. Assessment of inpatient paediatric care in first referral level hospitals in 13 districts in Kenya. Lancet. 2004. 363:1948–1953.
Article45. Berkley J, Mwangi I, Griffiths K, Ahmed I, Mithwani S, English M, et al. Assessment of severe malnutrition among hospitalized children in rural Kenya: comparison of weight for height and mid upper arm circumference. JAMA. 2005. 294:591–597.
Article46. Valid International, Community Based Therapeutic Care, first edition 2006. Accessed on Nov 20, 2012. Available at: http://www.fantaproject.org/downloads/pdfs/CTC_Manual_v1_Oct06.pdf.47. Schofield C, Ashworth A. Why have mortality rates for severe malnutrition remained so high? Bull World Health Organ. 1996. 74:223–229.48. Golden M. The effects of malnutrition in the metabolism of children. Trans R Soc Trop Med Hyg. 1988. 82:3–6.
Article49. Golden MHN. Severe Malnutrition. The Oxford Textbook of Medicine. 1996. Oxford: Oxford University Press;1278–1296.50. Collins S, Sadler K. Outpatient care for severely malnourished children in emergency relief programmes: a retrospective cohort study. Lancet. 2002. 360:1824–1830.
Article51. Sphere Project Team. The Sphere Project: Humanitarian charter and minimum standards in disaster response. 2011. Accessed on Nov 20, 2012. Geneva: The Sphere Project;Available at http://www.spherehandbook.org/en/management-of-acute-malnutrition-and-micronutrient-deficiencies-standard-2-severe-acute-malnutrition/.52. Tectonidis M. Crisis in Niger--outpatient care for severe acute malnutrition. N Engl J Med. 2006. 354:224–227.
Article53. Collins S, Dent N, Binns P, Bahwere P, Sadler K, Hallam A. Management of severe acute malnutrition in children. Lancet. 2006. 368:1992–2000.
Article54. Vygen SB, Roberfroid D, Captier V, Kolsteren P. Treatment of severe acute malnutrition in infants aged <6 months in niger. J Pediatr. 2012. [Epub ahead of print].55. WHO. Report of an informal consultation on the community-based management of severe malnutrition in children. Accessed on Nov 11, 2012. Accessible at: http://www.who.int/nutrition/topics/Meeting_report.pdf.56. Van Damme W. Medical assistance to self-settled refugees. Guinea 1990-1996. 1998. Assessed on Dec 4, 2012. Antwerp: ITG Press;Available at http://dspace.itg.be/bitstream/10390/4986/1/1998shso0011.pdf.57. Jha P, Bangoura O, Ranson K. The cost-effectiveness of forty health interventions in Guinea. Health Policy Plan. 1998. 13:249–262.
Article58. Sandige H, Ndekha MJ, Briend A, Ashorn P, Manary MJ. Home-based treatment of malnourished Malawian children with locally produced or imported ready-to-use food. J Pediatr Gastroenterol Nutr. 2004. 39:141–146.
Article59. Manary MJ, Ndkeha MJ, Ashorn P, Maleta K, Briend A. Home based therapy for severe malnutrition with ready-to-use food. Arch Dis Child. 2004. 89:557–561.
Article60. Ndekha MJ, Manary MJ, Ashorn P, Briend A. Home-based therapy with ready-to-use therapeutic food is of benefit to malnourished, HIV-infected Malawian children. Acta Paediatr. 2005. 94:222–225.
Article61. Ashraf H, Alam NH, Chisti MJ, Mahmud SR, Hossain MI, Ahmed T, et al. A follow-up experience of 6 months after treatment of children with severe acute malnutrition in Dhaka, Bangladesh. J Trop Pediatr. 2012. 58:253–257.
Article62. Puett C, Sadler K, Alderman H, Coates J, Fiedler JL, Myatt M. Cost-effectiveness of the community-based management of severe acute malnutrition by community health workers in southern Bangladesh. Health Policy Plan. 2012. [Epub ahead of print].
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Fibrocalculous Pancreatic Diabetes With Familial Tendency
- Early nutrition and adult health: Perspectives for international and community nutrition programs and policies
- Potential opportunities to reduce cervical cancer by addressing risk factors other than HPV
- Co-occurrence of Frailty, Possible Sarcopenia, and Malnutrition in Community-Dwelling Older Outpatients: A Multicentre Observational Study
- Nutritional Management in Dementia