Korean J Urol.
2009 Oct;50(10):955-962.
Oncologic Outcome following Laparoscopic Radical Prostatectomy and the Difference in Oncologic Outcomes according to the Site of the Positive Margin: Comparison of the Apical Positive Margin with the Non-Apical Positive Margin
- Affiliations
-
- 1Department of Urology, The Catholic University of Korea College of Medicine, Seoul, Korea. tkhwang@catholic.ac.kr
Abstract
- PURPOSE
The aim of this study was to analyze oncologic outcomes based on 7 years of consecutive experience with laparoscopic radical prostatectomy (LRP) and to assess the prognostic difference between an apical positive margin and a non-apical positive margin.
MATERIALS AND METHODS
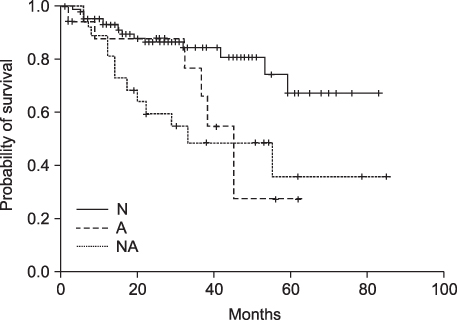
We reviewed 202 patients who underwent LRP between July 2001 and July 2007 (pathologic stage: T2-T3b, without any adjunctive therapy). Biochemical recurrence (bR) was defined as two consecutive prostate-specific antigen (PSA) values greater than 0.2 ng/ml. We analyzed the differences in bR among the negative margin group (N), the apical positive margin group (A), and the non-apical positive margin group (NA) and factors predicting bR. RESULTS: Overall 3-year probability of bR-free survival (bRFS) was 78% (pT2, 83.7%; pT3, 60.9%). For low-, intermediate-, and high-risk cancer, 3-year bRFS was 94.7%, 82.8%, and 60.7%, respectively. Of the 155 men who had negative and single-site positive margins, the numbers in the N, A, and NA groups were 108, 19, and 28, respectively. bR rates for the N, A, and NA groups were 14.8%, 36.8%, and 46.4%, respectively. Kaplan-Meier curves showed that a positive surgical margin had a significant higher bR compared with the N group; however, the A group experienced a similar bRFS compared with the NA group (p=0.613). Multivariate Cox proportional hazards analysis indicated no significant difference of effect on time to bR between the A and NA groups (hazard ratio=1.213; 95% confidence interval: 0.482-3.052).
CONCLUSIONS
Our results were almost identical to previous reports of radical prostatectomy in pT2 disease. With increasing experience, we could expect improved oncologic outcomes. In comparison with the NA group, the A group did not show a significant prognostic difference.
Keyword
MeSH Terms
Figure
Reference
-
1. Geary ES, Dendinger TE, Freiha FS, Stamey TA. Nerve sparing radical prostatectomy: a different view. J Urol. 1995. 154:145–149.2. Swindle P, Eastham JA, Ohori M, Kattan MW, Wheeler T, Maru N, et al. Do margins matter? The prognostic significance of positive surgical margins in radical prostatectomy specimens. J Urol. 2008. 179:5 Suppl. S47–S51.3. Cheng L, Darson MF, Bergstralh EJ, Slezak J, Myers RP, Bostwick DG. Correlation of margin status and extraprostatic extension with progression of prostate carcinoma. Cancer. 1999. 86:1775–1782.4. Grossfeld GD, Chang JJ, Broering JM, Miller DP, Yu J, Flanders SC, et al. Impact of positive surgical margins on prostate cancer recurrence and the use of secondary cancer treatment: data from the CaPSURE database. J Urol. 2000. 163:1171–1177.5. Swindle P, Eastham JA, Ohori M, Kattan MW, Wheeler T, Maru N, et al. Do margins matter? The prognostic significance of positive surgical margins in radical prostatectomy specimens. J Urol. 2005. 174:903–907.6. Cho KS, Hong SJ, Chung BH. The impact of positive surgical margins on biochemical recurrence after radical retropubic prostatectomy. Korean J Urol. 2004. 45:416–422.7. Fesseha T, Sakr W, Grignon D, Banerjee M, Wood DP Jr, Pontes JE. Prognostic implications of a positive apical margin in radical prostatectomy specimens. J Urol. 1997. 158:2176–2179.8. Stamey TA, McNeal JE, Yemoto CM, Sigal BM, Johnstone IM. Biological determinants of cancer progression in men with prostate cancer. JAMA. 1999. 281:1395–1400.9. Shah O, Melamed J, Lepor H. Analysis of apical soft tissue margins during radical retropubic prostatectomy. J Urol. 2001. 165:1943–1948.10. McNeal JE. Normal and pathologic anatomy of prostate. Urology. 1981. 17:Suppl 3. 11–16.11. McNeal JE, Villers AA, Redwine EA, Freiha FS, Stamey TA. Capsular penetration in prostate cancer. Significance for natural history and treatment. Am J Surg Pathol. 1990. 14:240–247.12. Myers RP, Goellner JR, Cahill DR. Prostate shape, external striated urethral sphincter and radical prostatectomy: the apical dissection. J Urol. 1987. 138:543–550.13. Jang J, Cha SH, Kim DB, Kim JC, Hwang TK. Laparoscopic radical prostatectomy. Korean J Urol. 2002. 43:342–345.14. True LD. Surgical pathology examination of the prostate gland. Practice survey by American society of clinical pathologists. Am J Clin Pathol. 1994. 102:572–579.15. Catalona WJ, Smith DS. Cancer recurrence and survival rates after anatomic radical retropubic prostatectomy for prostate cancer: intermediate-term results. J Urol. 1998. 160:2428–2434.16. Han M, Partin AW, Pound CR, Epstein JI, Walsh PC. Long-term biochemical disease-free and cancer-specific survival following anatomic radical retropubic prostatectomy. The 15-year Johns Hopkins experience. Urol Clin North Am. 2001. 28:555–565.17. Guillonneau B, el-Fettouh H, Baumert H, Cathelineau X, Doublet JD, Fromont G, et al. Laparoscopic radical prostatectomy: oncological evaluation after 1,000 cases a Montsouris Institute. J Urol. 2003. 169:1261–1266.18. Rassweiler J, Stolzenburg J, Sulser T, Deger S, Zumbe J, Hofmockel G, et al. Laparoscopic radical prostatectomy--the experience of the German Laparoscopic Working Group. Eur Urol. 2006. 49:113–119.19. Vickers AJ, Savage CJ, Hruza M, Tuerk I, Koenig P, Martinez-Pineiro L, et al. The surgical learning curve for laparoscopic radical prostatectomy: a retrospective cohort study. Lancet Oncol. 2009. 10:475–480.20. Kim SW, Hong SH, Hwang TK. Laparoscopic radical prostatectomy: the learning curve of the initial 150 cases. Korean J Urol. 2008. 49:879–885.21. Epstein JI, Partin AW, Sauvageot J, Walsh PC. Prediction of progression following radical prostatectomy. A multivariate analysis of 721 men with long-term follow-up. Am J Surg Pathol. 1996. 20:286–292.22. D'Amico AV, Whittington R, Malkowicz SB, Schultz D, Schnall M, Tomaszewski JE, et al. Combined modality staging of prostate carcinoma and its utility in predicting pathologic stage and postoperative prostate specific antigen failure. Urology. 1997. 49:3A Suppl. 23–30.23. Blute ML, Bostwick DG, Bergstralh EJ, Slezak JM, Martin SK, Amling CL, et al. Anatomic site-specific positive margins in organ-confined prostate cancer and its impact on outcome after radical prostatectomy. Urology. 1997. 50:733–739.24. van den Ouden D, Bentvelsen FM, Boeve ER, Schröder FH. Positive margins after radical prostatectomy: correlation with local recurrence and distant progression. Br J Urol. 1993. 72:489–494.25. Epstein JI, Pizov G, Walsh PC. Correlation of pathologic findings with progression after radical retropubic prostatectomy. Cancer. 1993. 71:3582–3593.26. Obek C, Sadek S, Lai S, Civantos F, Rubinowicz D, Soloway MS. Positive surgical margins with radical retropubic prostatectomy: anatomic site-specific pathologic analysis and impact on prognosis. Urology. 1999. 54:682–688.27. Sofer M, Hamilton-Nelson KL, Civantos F, Soloway MS. Positive surgical margins after radical retropubic prostatectomy: the influence of site and number on progression. J Urol. 2002. 167:2453–2456.28. Ohori M, Abbas F, Wheeler TM, Kattan MW, Scardino PT, Lerner SP. Pathological features and prognostic significance of prostate cancer in the apical section determined by whole mount histology. J Urol. 1999. 161:500–504.29. Eastham JA, Kuroiwa K, Ohori M, Serio AM, Gorbonos A, Maru N, et al. Prognostic significance of location of positive margins in radical prostatectomy specimens. Urology. 2007. 70:965–969.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic Radical Prostatectomy: the Learning Curve of the Initial 150 Cases
- Extraperitoneal Laparoscopic Radical Prostatectomy: Clinical Experience and Learning Curve with 103 Cases
- Oncologic Outcomes of Patients With Gleason Score 7 and Tertiary Gleason Pattern 5 After Radical Prostatectomy
- Learning Curve for Robot-Assisted Laparoscopic Radical Prostatectomy for Pathologic T2 Disease
- Cribriform Pattern at the Surgical Margin is Highly Predictive of Biochemical Recurrence in Patients Undergoing Radical Prostatectomy