Korean J Urol.
2009 Sep;50(9):870-878.
The Feasibility of Robot-Assisted Laparoscopic Radical Cystectomy with Pelvic Lymphadenectomy: from the Viewpoint of Extended Pelvic Lymphadenectomy
- Affiliations
-
- 1Department of Urology, College of Medicine, Korea University, Seoul, Korea. mdksh@korea.ac.kr
Abstract
- PURPOSE
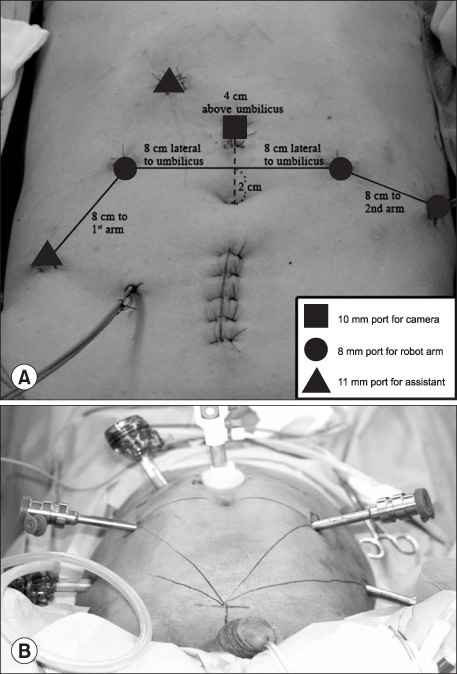
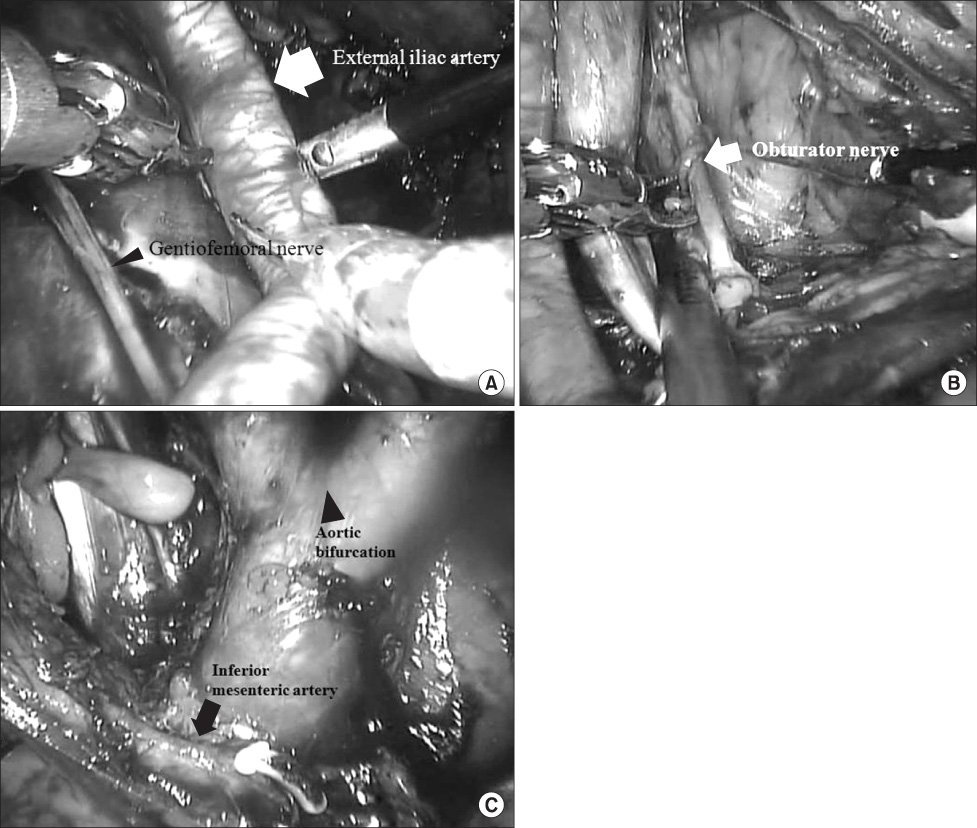
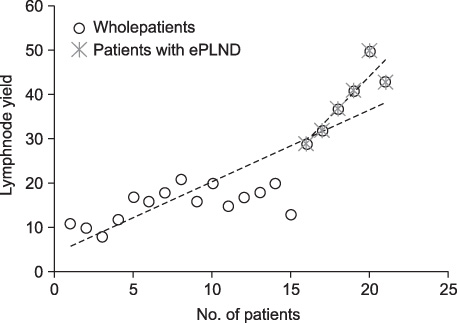
We evaluated the feasibility of robot-assisted laparoscopic radical cystectomy (RARC) with pelvic lymph node dissection (PLND), especially extended PLND (ePLND), during our initial experience with this technique. MATERIALS AND METHODS: From August 2007 to March 2009, prospective data were obtained from the 21 consecutive patients who underwent RARC with PLND at Korea University Hospital. Data included baseline characteristics, perioperative variables, pathological outcomes, and complications. Evidence of the lymph node yield curve was examined by using linear regression to compare the number of lymph nodes obtained. RESULTS: Among 21 patients who underwent RARC, 13 had ileal conduit urinary diversion and 8 had orthotopic neobladder. Standard PLND (sPLND) was performed in the first 15 patients, and ePLND was performed in the more recent 6 patients. The mean total operative time was 515.5+/-145.1 minutes, and the mean estimated blood loss was 346.8+/-205.9 ml. The mean time for PLND was 106.7+/-25.2 minutes in patients with ePLND and 72.1+/-14.1 minutes in patients with sPLND (p=0.001). All patients had negative surgical margins. The mean number of retrieved nodes was 23.5+/-12.8 (range, 8-50) in all patients: 38.6+/-10.8 (range, 29-50) in ePLND and 15.7+/-12.2 (range, 8-21) in sPLND. CONCLUSIONS: Perioperative data and oncologic features showed that RARC with PLND is feasible. Robot-assisted laparoscopic surgery is a safe and effective procedure with acceptable morbidity and good oncologic results from the viewpoint of PLND, especially ePLND.
MeSH Terms
Figure
Reference
-
1. Stein JP, Lieskovsky G, Cote R, Groshen S, Feng AC, Boyd S, et al. Radical cystectomy in the treatment of invasive bladder cancer: long-term results in 1,054 patients. J Clin Oncol. 2001. 19:666–675.2. Madersbacher S, Hochreiter W, Burkhard F, Thalmann GN, Danuser H, Markwalder R, et al. Radical cystectomy for bladder cancer today--a homogeneous series without neoadjuvant therapy. J Clin Oncol. 2003. 21:690–696.3. Herr HW. Extent of surgery and pathology evaluation has an impact on bladder cancer outcomes after radical cystectomy. Urology. 2003. 61:105–108.4. Leissner J, Hohenfellner R, Thüroff JW, Wolf HK. Lymph-adenectomy in patients with transitional cell carcinoma of the urinary bladder: significance for staging and prognosis. BJU Int. 2000. 85:817–823.5. Poulsen AL, Horn T, Steven K. Radical cystectomy: extending the limits of pelvic lymph node dissection improves survival for patients with bladder cancer confined to the bladder wall. J Urol. 1998. 160:2015–2019.6. Schuessler WW, Vancaillie TG, Reich H, Griffith DP. Transperitoneal endosurgical lymphadenectomy in patients with localized prostate cancer. J Urol. 1991. 145:988–991.7. Finelli A, Gill IS, Desai MM, Moinzadeh A, Magi-Galluzzi C, Kaouk JH. Laparoscopic extended pelvic lymphadenectomy for bladder cancer: technique and initial outcomes. J Urol. 2004. 172:1809–1812.8. Türk I, Deger S, Winkelmann B, Schönberger B, Loening SA. Laparoscopic radical cystectomy with continent urinary diversion (rectal sigmoid pouch) performed completely intracorporeally: the initial 5 cases. J Urol. 2001. 165:1863–1866.9. Woods M, Thomas R, Davis R, Andrews PE, Ferrigni RG, Cheng J, et al. Robot-assisted extended pelvic lymphadenectomy. J Endourol. 2008. 22:1297–1302.10. Guru KA, Sternberg K, Wilding GE, Tan W, Butt ZM, Mohler JL, et al. The lymph node yield during robot-assisted radical cystectomy. BJU Int. 2008. 102:231–234.11. Martin RC 2nd, Brennan MF, Jaques DP. Quality of complication reporting in the surgical literature. Ann Surg. 2002. 235:803–813.12. Clavien PA, Sanabria JR, Strasberg SM. Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery. 1992. 111:518–526.13. Leadbetter WF, Cooper JF. Regional gland dissection for carcinoma of the bladder; a technique for one-stage cystectomy, gland dissection, and bilateral uretero-enterostomy. J Urol. 1950. 63:242–260.14. Colston JA, Leadbetter WF. Infiltrating carcinoma of the bladder. J Urol. 1936. 36:669.15. Whitmore WF Jr, Marshall VF. Radical total cystectomy for cancer of the bladder: 230 consecutive cases five years later. Trans Am Assoc Genitourin Surg. 1962. 54:20–32.16. Mehrsai A, Mansoori D, Taheri Mahmoudi M, Sina A, Seraji A, Pourmand G. A comparison between clinical and pathologic staging in patients with bladder cancer. Urol J. 2004. 1:85–89.17. Shariat SF, Palapattu GS, Karakiewicz PI, Rogers CG, Vazina A, Bastian PJ, et al. Discrepancy between clinical and pathologic stage: impact on prognosis after radical cystectomy. Eur Urol. 2007. 51:137–149.18. Anjos DA, Etchebehere EC, Ramos CD, Santos AO, Albertotti C, Camargo EE. 18F-FDG PET/CT delayed images after diuretic for restaging invasive bladder cancer. J Nucl Med. 2007. 48:764–770.19. Sherif A, Garske U, de la Torre M, Thörn M. Hybrid SPECT-CT: an additional technique for sentinel node detection of patients with invasive bladder cancer. Eur Urol. 2006. 50:83–91.20. Herr HW, Bochner BH, Dalbagni G, Donat SM, Reuter VE, Bajorin DF. Impact of the number of lymph nodes retrieved on outcome in patients with muscle invasive bladder cancer. J Urol. 2002. 167:1295–1298.21. Leissner J, Ghoneim MA, Abol-Enein H, Thüroff JW, Franzaring L, Fisch M, et al. Extended radical lymph-adenectomy in patients with urothelial bladder cancer: results of a prospective multicenter study. J Urol. 2004. 171:139–144.22. Bochner BH, Herr HW, Reuter VE. Impact of separate versus en bloc pelvic lymph node dissection on the number of lymph nodes retrieved in cystectomy specimens. J Urol. 2001. 166:2295–2296.23. Skinner DG. Management of invasive bladder cancer: a meticulous pelvic node dissection can make a difference. J Urol. 1982. 128:34–36.24. Dhar NB, Klein EA, Reuther AM, Thalmann GN, Madersbacher S, Studer UE. Outcome after radical cystectomy with limited or extended pelvic lymph node dissection. J Urol. 2008. 179:873–878.25. Stein JP. Lymphadenectomy in bladder cancer: how high is "high enough"? Urol Oncol. 2006. 24:349–355.26. Brossner C, Pycha A, Toth A, Mian C, Kuber W. Does extended lymphadenectomy increase the morbidity of radical cystectomy? BJU Int. 2004. 93:64–66.27. Kwak JJ, Kim TH, Sung GT. Short term outcomes of laparoscopic radical cystectomy with an extracorporeal ileal conduit: comparative analysis with the open method. Korean J Urol. 2007. 48:938–944.28. Haber GP, Gill IS. Laparoscopic radical cystectomy for cancer: oncological outcomes at up to 5 years. BJU Int. 2007. 100:137–142.29. Abraham JB, Young JL, Box GN, Lee HJ, Deane LA, Ornstein DK. Comparative analysis of laparoscopic and robot-assisted radical cystectomy with ileal conduit urinary diversion. J Endourol. 2007. 21:1473–1480.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radical Cystectomy with Pelvic Lymphadenectomy in Bladder Tumor: Review of 14 Cases
- Laparoscopic Pelvic Lymphadenectomy in Cervical Cancer
- The Impact of Pelvic Lymphadenectomy on the Survival of Patients Who Underwent Radical Cystectomy for Transitional Cell Carcinoma of the Bladder
- Robot-assisted extraperitoneal paraaortic lymphadenectomy (RAePAL) performed with the bipolar cutting method
- Laparoscopic pelvic and para-aortic lymphadenectomy