Korean J Urol.
2010 Jan;51(1):34-39.
Hand-Assisted Laparoscopic Right Donor Nephrectomy: Safety and Feasibility
- Affiliations
-
- 1Department of Urology, The Catholic University of Korea College of Medicine, Seoul, Korea. tkhwang@catholic.ac.kr
Abstract
- PURPOSE
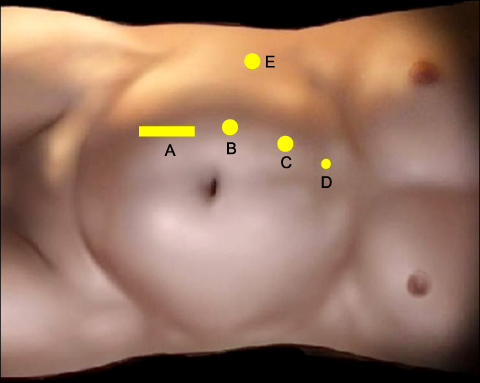
We aimed to prove the safety and feasibility of right-sided hand-assisted laparoscopic donor nephrectomy (HALDN). MATERIALS AND METHODS: Between May 2006 and May 2009, 16 patients underwent right-sided HALDN at our institution. Of these patients, 15 showed significantly lower renal function in the right kidney than in the left one and 1 had a stone in the right kidney. When the right renal vein was divided, an EndoGIA stapling device was placed on the wall of the inferior vena cava to gain a maximal length of the vein. We evaluated intraoperative and postoperative parameters such as operative time, delivery time, warm ischemic time, estimated blood loss, intraoperative and postoperative complication rates, length of hospital stay, and serum creatinine levels of donors (at the time of discharge) and recipients (4 weeks postoperatively), comparing the right-sided HALDN group (our study) with a left-sided HALDN group (from a previously reported study). RESULTS: A total of 16 right-sided HALDNs were successfully performed without any complications or open conversion. All of the intraoperative and postoperative parameters were similar between the right-sided HALDN and left-sided HALDN groups. There were no technical problems in the recipients in the anastomosis of the renal vein, and the ureteral anastomoses were also successful. CONCLUSIONS: Right-sided HALDN is safe and technically feasible in a donor, showing favorable graft outcomes. The results of our study suggest that right-sided HALDN may be preferable in patients with significantly lower renal function in the right kidney than in the left one.
Keyword
MeSH Terms
Figure
Reference
-
1. Choi HW, Jung JW, Jung JU, Cho HJ, Hong SH, Kim JC, et al. Feasibility and safety of performing hand-assisted laparoscopic donor nephrectomy for patients with multiple renal arteries. Korean J Urol. 2008. 49:443–448.2. Leary FJ, Deweerd JH. Living donor nephrectomy. J Urol. 1973. 109:947–948.3. Johnston T, Reddy K, Mastrangelo M, Lucas B, Ranjan D. Multiple renal arteries do not pose an impediment to the routine use of laparoscopic donor nephrectomy. Clin Transplant. 2001. 15:Supppl 6. 62–65.4. Hsu TH, Su LM, Ratner LE, Trock BJ, Kavoussi LR. Impact of renal artery multiplicity on outcomes of renal donors and recipients in laparoscopic donor nephrectomy. Urology. 2003. 61:323–327.5. Husted TL, Hanaway MJ, Thomas MJ, Woodle ES, Buell JF. Laparoscopic living donor nephrectomy for kidneys with multiple arteries. Transplant Proc. 2005. 37:629–630.6. Kim W, Hong J, Kim CS, Ahn H, Ahn TY, Hong B. The preoperative risk factors that influence the postoperative renal function in living donor nephrectomy: the impact of dominant kidney nephrectomy. Korean J Urol. 2008. 49:37–42.7. Yoo ES, Kim BW, Chang SK. Living donor nephrectomy: surgical selection criteria of laterality. Korean J Urol. 2002. 43:923–926.8. Shokeir AA, Gad HM, el-Diasty T. Role of radioisotope renal scans in the choice of nephrectomy side in live kidney donors. J Urol. 2003. 170:373–376.9. Liu KL, Chiang YJ, Wu CT, Lai WJ, Wang HH, Chu SH. Why we consistently use the left donor kidney in living related transplantation: initial experience of right laparoscopic donor nephrectomy and comparison with left nephrectomy. Transplant Proc. 2006. 38:1977–1979.10. Maciel RF. Hand-assisted laparoscopic live donor nephrectomy (right-sided approach): experience obtained from 31 cases. Transplant Proc. 2007. 39:2476–2477.11. Meyer F, Santos LS, Varaschin AE, Patriani AH, Pimpao BF. Hand-assisted right laparoscopic nephrectomy in living donor. Int Braz J Urol. 2005. 31:17–21.12. Wolf JS Jr, Tchetgen MB, Merion RM. Hand-assisted laparoscopic live donor nephrectomy. Urology. 1998. 52:885–887.13. Yeo WG, Kim HH. Hand-assisted laparoscopic live donor nephrectomy; comparison to open donor nephrectomy. Korean J Urol. 2004. 45:141–148.14. Abrahams HM, Freise CE, Kang SM, Stoller ML, Meng MV. Technique, indications and outcomes of pure laparoscopic right donor nephrectomy. J Urol. 2004. 171:1793–1796.15. Wang DS, Bird VG, Winfield HN, Rayhill S. Hand-assisted laparoscopic right donor nephrectomy: surgical technique. J Endourol. 2004. 18:205–209.16. Rao MM, Russell CH. Laparoscopic live donor nephrectomy. ANZ J Surg. 2005. 75:6–9.17. El-Galley R. Novel technique for hand assisted laparoscopic right donor nephrectomy. J Urol. 2007. 178:2062–2066.18. Ko EY, Castle EP, Desai PJ, Moss AA, Reddy KS, Mekeel KL, et al. Utility of the endovascular stapler for right-sided laparoscopic donor nephrectomy: a 7-year experience at Mayo Clinic. J Am Coll Surg. 2008. 207:896–903.19. Chandak P, Kessaris N, Challacombe B, Olsburgh J, Calder F, Mamode N. How safe is hand-assisted laparoscopic donor nephrectomy?--results of 200 live donor nephrectomies by two different techniques. Nephrol Dial Transplant. 2009. 24:293–297.20. Keller JE, Dolce CJ, Griffin D, Heniford BT, Kercher KW. Maximizing the donor pool: use of right kidneys and kidneys with multiple arteries for live donor transplantation. Surg Endosc. 2009. 23:2327–2331.21. Sawatzky M, Altaf A, Ellsmere J, Klassen D, Walsh M, Molinari M, et al. Is right laparoscopic donor nephrectomy right? Surg Endosc. 2009. 23:1321–1325.22. Saad S, Paul A, Treckmann J, Nagelschmidt M, Heiss M, Arns W. Laparoscopic live donor nephrectomy for right kidneys: experience in a German community hospital. Surg Endosc. 2008. 22:674–678.23. Dols LF, Kok NF, Alwayn IP, Tran TC, Weimar W, Ijzermans JN. Laparoscopic donor nephrectomy: a plea for the right-sided approach. Transplantation. 2009. 87:745–750.24. Chin JL, Yip SK, McFarlane N. Clinical impact of adjunctive donor microvascular reconstruction on renal transplantation. Can J Urol. 2003. 10:1803–1808.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Severe Hypercarbia by Subcutaneous Emphysema Occurring during Hand Assisted Laparoscopic Donor Nephrectomy: A case report
- Feasibility and Safety of Performing Hand-assisted Laparoscopic Donor Nephrectomy for Patients with Multiple Renal Arteries
- Comparison of Hand-assisted Laparoscopic Versus Retroperitoneo-scopic Radical Nephrectomy
- Hand-Assisted Laparoscopic Nephrectomy and Auto-Transplantation for a Hilar Renal Artery Aneurysm: A Case Report
- Donor Nephrectomy : Comparison of Open, Hand-assisted and Laparoscopic Donor Nephrectomy