Korean J Urol.
2010 May;51(5):354-357.
The Value of Estimation of Distal Ureteral Dilatation in Primary Vesicoureteral Reflux
- Affiliations
-
- 1Department of Urology, School of Medicine, Kyungpook National University, Daegu, Korea. skchung@mail.knu.ac.kr
Abstract
- PURPOSE
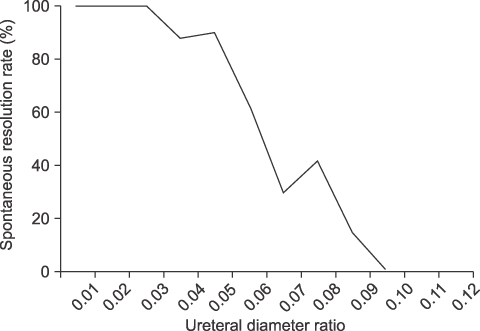
Recently, several studies have suggested that distal ureteral dilatation is an important factor influencing the spontaneous resolution of primary vesicoureteral reflux (VUR). We evaluated the relationship between distal ureteral dilatation and the spontaneous resolution of primary VUR. MATERIALS AND METHODS: The medical records of 114 patients with primary VUR maintained on prophylactic antibiotics from April 1999 to August 2008 were retrospectively reviewed. The patients' mean age was 24.2 months (range, 6-108 months). There were 66 male patients and 48 female patients. The mean follow-up was 37.6 months (range, 12-102 months). We analyzed various factors including age, gender, grade of reflux, laterality, and ureteral diameter ratio (UDR; the largest ureteral diameter was divided by the distance from the L1-4 vertebral body to minimize the differences in diameter by age) to determine whether these factors influenced the spontaneous resolution of primary VUR. RESULTS: Unilateral, low-grade reflux and low UDR were significantly associated with the spontaneous resolution of reflux (p=0.048, p<0.001, and p<0.001, respectively). The multivariate analysis revealed that the spontaneous resolution rate of primary reflux was significantly higher in patients with low UDR than in patients with high UDR (p<0.001). CONCLUSIONS: The degree of distal ureteral dilatation is expected to be another important factor in determining therapeutic course and predicting the spontaneous resolution of VUR.
Keyword
MeSH Terms
Figure
Reference
-
1. Bailey R. Hodson J, Kincaid-Smith P, editors. Vesicoureteric reflux in healthy infants and children. Reflux nephropathy. 1979. New York: Masson;59–61.2. Lebowitz RL, Olbing H, Parkkulainen KV, Smellie JM, Tamminen-Möbius TE. International system of radiographic grading of vesicoureteric reflux. Inernational Reflux Study in Children. Pediatr Radiol. 1985. 15:105–109.3. Smellie JM, Jodal U, Lax H, Möbius TT, Hirche H, Olbing H. Outcome at 10 years of severe vesicoureteric reflux managed medically: report of the International Reflux Study in Children. J Pediatr. 2001. 139:656–663.4. Atla A, Keating MA. Walsh PC, Retik AB, Vaughan ED, Wein AJ, editors. Vesicoureteral reflux and megaureter. Campbell's urology. 2007. 9th ed. Philadelphia: Saunders;3423–3481.5. Méndez R, Somoza I, Tellado MG, Liras J, Sanchez A, Pais E, et al. Predictive value of clinical factors for successful endoscopic correction of primary vesicoureteral reflux grades III-IV. J Pediatr Urol. 2006. 2:545–550.6. Lee DW, Kang KM, Oh WS, Kim JS, Chung SK. Risk factors for treatment failure after endoscopic subureteral injection of dextranomer/hyaluronic acid copolymer (Deflux®) for vesicoureteral reflux. Korean J Urol. 2009. 50:61–66.7. Currarino G, Williams B, Reisch JS. Linear growth of the thoracic spine in chest roentgenograms from birth to 16 years. Skeletal Radiol. 1986. 15:628–630.8. Yeung CK, Godley ML, Dhillon HK, Gordon I, Duffy PG, Ransley PG. The characteristics of primary vesico-ureteric reflux in male and female infants with pre-natal hydronephrosis. Br J Urol. 1997. 80:319–327.9. Park SY, Park HY, Woo YN. The factors affecting the outcome after medical management of vesicoureteral reflux. Korean J Urol. 2006. 47:994–1000.10. Chand DH, Rhoades T, Poe SA, Kraus S, Strife CF. Incidence and severity of vesicoureteral reflux in children related to age, gender, race and diagnosis. J Urol. 2003. 170:1548–1550.11. Yeom MH, Chung SK, Lee KS, Kim KS, Park JS, Ryu DS, et al. Incidnece of vesicoureteral reflux for prepuberty patients in Daegu city and Gyeongbuk area according to the clinical indications, gender, and age. Korean J Urol. 2005. 46:1284–1289.12. Schwab CW Jr, Wu HY, Selman H, Smith GH, Snyder HM 3rd, Canning DA. Spontaneous resolution of vesicoureteral reflux: a 15-year perspective. J Urol. 2002. 168:2594–2599.13. Sjöström S, Sillén U, Bachelard M, Hansson S, Stokland E. Spontaneous resolution of high grade infantile vesicoureteral reflux. J Urol. 2004. 172:694–698.14. Estrada CR Jr, Passerotti CC, Graham DA, Peters CA, Bauer SB, Diamond DA, et al. Nomograms for predicting annual resolution rate of primary vesicoureteral reflux: results from 2,462 children. J Urol. 2009. 182:1535–1541.15. Tamminen-Möbius T, Brunier E, Ebel KD, Lebowitz R, Olbing H, Seppänen U, et al. Cessation of vesicoureteral reflux for 5 years in infants and children allocated to medical treatment. The International Reflux Study in Children. J Urol. 1992. 148:1662–1666.16. Zerati Filho M, Calado AA, Barroso U Jr, Amaro JL. Spontaneous resolution rates of vesicoureteral reflux in Brazilian children: a 30-year experience. Int Braz J Urol. 2007. 33:204–212.17. Arant BS Jr. Medical management of mild and moderate vesicoureteral reflux: followup studies of infants and young children. A preliminary report of the Southwest Pediatric Nephrology Study Group. J Urol. 1992. 148:1683–1687.18. Barroso U Jr, Barroso VA, de Bessa J Jr, Calado AA, Zerati Filho M. Predictive factors for contralateral reflux in patients with conservatively treated unilateral vesicoureteral reflux. J Urol. 2008. 180:297–299.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Influence on the Upper Urinary Tract by Dilatation to Vesicoureteral Junction in Rabbit
- Experience of Posterior Urethral Valves with Vesicoureteral Reflux
- Clinical Aspects of Vesicoureteral Reflux
- The Role of Terminal Ureter in Vesicoureteral Reflux and Its Histological Analysis
- Bladder Neck Contracture in 3 Patients