Korean J Urol.
2010 Nov;51(11):745-751.
Prediction of Perineural Invasion and Its Prognostic Value in Patients with Prostate Cancer
- Affiliations
-
- 1Department of Urology, Busan Saint Mary's Medical Center, Busan, Korea.
- 2Department of Urology, Pusan National University School of Medicine, Busan, Korea. hongkooha@naver.com
- 3Department of Urology, Medical Research Institute, Pusan National University Hospital, Busan, Korea.
- 4Department of Urology, Maryknoll Medical Center, Busan, Korea.
Abstract
- PURPOSE
The prognostic significance of perineural invasion by prostate cancer is debated. We investigated the association between perineural invasion and clinicopathological factors and the effect of perineural invasion on survival in patients with prostate cancer.
MATERIALS AND METHODS
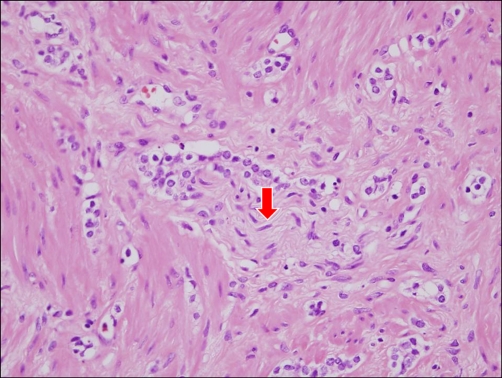
A total of 361 patients with prostate cancer without any neoadjuvant therapies prior to surgery from 1999 to 2010 were analyzed retrospectively. Whole-mount sections of surgical specimens from all patients who underwent radical prostatectomy were evaluated. Positive perineural invasion was defined as infiltration of cancer cells in the perineurium or neural fascicles. The relationship of perineural invasion with clinicopathological features and prognosis of prostate cancer was studied. We also researched preoperative factors that were associated with perineural invasion.
RESULTS
Perineural invasion in a prostatectomy specimen (PNIp) was positive in 188 of 361 patients (52.1%). In the multivariate analysis of the preoperative variables, PNIp was related to the primary Gleason grade (p=0.020), the number of positive cores (p=0.008), and the percentage of tumor cells in positive cores (p=0.021), but not to perineural invasion of a prostate biopsy. In the evaluation between PNIp and pathologic findings of the prostatectomy specimen, PNIp was related to the Gleason score (p=0.010), T-stage (p=0.015), and lymphovascular invasion (p=0.019). However, by multivariate analysis, the PNIp was not an independent prognostic factor of biochemical serum recurrence (p=0.364) or cancer-specific survival (p=0.726).
CONCLUSIONS
PNIp was significantly related to biologically aggressive tumor patterns but was not a prognostic factor for biochemical serum PSA recurrence or cancer-specific survival in patients with prostate cancer.
MeSH Terms
Figure
Reference
-
1. Liebig C, Ayala G, Wilks JA, Berger DH, Albo D. Perineural invasion in cancer: a review of the literature. Cancer. 2009; 115:3379–3391. PMID: 19484787.2. Marchesi F, Piemonti L, Montovani A, Allavena P. Molecular mechanisms of perineural invasion, a forgotten pathway of dissemination and metastasis. Cytokine Growth Factor Rev. 2010; 21:77–82. PMID: 20060768.
Article3. D'Amico AV, Wu Y, Chen MH, Nash M, Renshaw AA, Richie JP. Perineural invasion as a predictor of biochemical outcome following radical prostatectomy for select men with clinically localized prostate cancer. J Urol. 2001; 165:126–129. PMID: 11125380.4. Freedland SJ, Csathy GS, Dorey F, Aronson WJ. Percent prostate needle biopsy tissue with cancer is more predictive of biochemical failure or adverse pathology after radical prostatectomy than prostate specific antigen or Gleason score. J Urol. 2002; 167:516–520. PMID: 11792909.
Article5. Gleason DF, Mellinger GT. Prediction of prognosis for prostatic adenocarcinoma by combined histological grading and clinical staging. J Urol. 1974; 111:58–64. PMID: 4813554.
Article6. Liebig C, Ayala G, Wilks J, Verstovsek G, Liu H, Agarwal N, et al. Perineural invasion is an independent predictor of outcome in colorectal cancer. J Clin Oncol. 2009; 27:5131–5137. PMID: 19738119.
Article7. Ha HK, Yun CJ, Lee SS, Shin DG, Lee W, Lee ZZ, et al. Survival rates and related factors in men with hormone-refractory prostate cancer. Korean J Urol. 2009; 50:649–655.
Article8. Loeb S, Epstein JI, Humphreys EB, Walsh PC. Does perineural invasion on prostate biopsy predict adverse prostatectomy outcomes? BJU Int. 2010; 105:1510–1513. PMID: 19694710.
Article9. Ravery V, Boccon-Gibod LA, Dauge-Geffroy MC, Billebaud T, Delmas V, Meulemans A, et al. Systematic biopsies accurately predict extracapsular extension of prostate cancer and persistent/recurrent detectable PSA after radical prostatectomy. Urology. 1994; 44:371–376. PMID: 7521093.
Article10. Endrizzi J, Seay T. The relationship between early biochemical failure and perineural invasion in pathological T2 prostate cancer. BJU Int. 2000; 85:696–698. PMID: 10759668.
Article11. Ozcan F. Correlation of perineural invasion on radical prostatectomy specimens with other pathologic prognostic factors and PSA failure. Eur Urol. 2001; 40:308–312. PMID: 11684847.
Article12. Ng JC, Koch MO, Daggy JK, Cheng L. Perineural invasion in radical prostatectomy specimens: lack of prognostic significance. J Urol. 2004; 172:2249–2251. PMID: 15538241.
Article13. Quinn DI, Henshall SM, Brenner PC, Kooner R, Golovsky D, O'Neill GF, et al. Prognostic significance of preoperative factors in localized prostate carcinoma treated with radical prostatectomy: importance of percentage of biopsies that contain tumor and the presence of biopsy perineural invasion. Cancer. 2003; 97:1884–1893. PMID: 12673714.14. Lee IH, Roberts R, Shah RB, Wojno KJ, Wei JT, Sandler HM. Perineural invasion is a marker for pathologically advanced disease in localized prostate cancer. Int J Radiat Oncol Biol Phys. 2007; 68:1059–1064. PMID: 17398032.
Article15. Jeon HG, Bae J, Yi JS, Hwang IS, Lee SE, Lee E. Perineural invasion is a prognostic factor for biochemical failure after radical prostatectomy. Int J Urol. 2009; 16:682–686. PMID: 19602004.
Article16. Stone NN, Stock RG, Parikh D, Yeghiayan P, Unger P. Perineural invasion and seminal vesicle involvement predict pelvic lymph node metastasis in men with localized carcinoma of the prostate. J Urol. 1998; 160:1722–1726. PMID: 9783940.
Article17. Miyake H, Sakai I, Harada K, Eto H, Hara I. Limited value of perineural invasion in radical prostatectomy specimens as a predictor of biochemical recurrence in Japanese men with clinically localized prostate cancer. Hinyokika Kiyo. 2005; 51:241–246. PMID: 15912782.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of the Serum Cholesterol Level on the Clinicopathologic Characteristics of Prostate Cancer
- Prognostic Significance of Lymphatic and Perineural Invasions in Patients with Gastric Cancer Who Have No Lymph Node and Serosal Involvement
- Predictors of Biochemical Failure after Radical Perineal Prostatectomy for Localized Prostate Cancer
- Should the Extrahepatic Bile Duct be Resected for T2 Gallbladder Cancer?
- Influence of Blood Vessels, Lymphatics and Perineural Invasion on Prognosis of Patients Treated with Radical Cystectomy for Transitional Cell Carcinoma of Bladder