Korean J Urol.
2010 Dec;51(12):847-852.
Rethinking Suprapubic Cystostomy in Voiding Dysfunction: New Trial with Timed Drainage
- Affiliations
-
- 1Department of Urology, Bundang Jesaeng Hospital, Seongnam, Korea. sjhwany@hanmail.net
Abstract
- PURPOSE
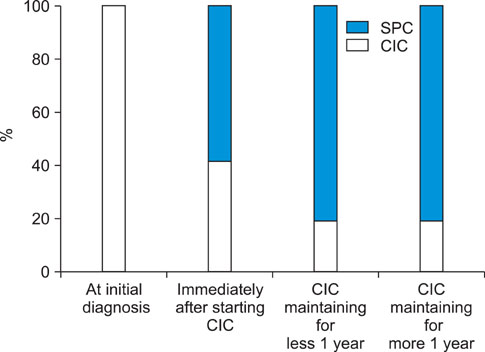
Today, many patients with voiding dysfunction select suprapubic cystostomy (SPC) instead of clean intermittent catheterization (CIC) for practical reasons. There is thus a need to reconsider SPC as a management for voiding dysfunction. We designed SPC with timed drainage (TSPCD) and evaluated its effectiveness compared with continuous drainage with a urine bag (CSPCD).
MATERIALS AND METHODS
Between January 2006 and January 2010, a total of 82 patients underwent SPC. Patients undergoing SPC were randomly assigned to CSPCD or TSPCD. Patient characteristics, complications, and the results of urine cultures were compared between the two groups through retrospective chart reviews. Also, preferences for CSPCD and TSPCD in another 15 patients who had experienced both CSPCD and TSPCD were investigated.
RESULTS
The CSPCD and TSPCD groups comprised 46 and 36 patients, respectively. In a comparison of complications between the two groups, the incidence of acute symptomatic cystitis was significantly lower in the TSPCD group than in the CSPCD group (43% vs. 20%, p=0.032). The incidence of symptomatic urinary tract infection (UTI) was lower in the TSPCD group. Positive urine culture rates were 89.7% and 72.4% in groups 1 and 2, respectively. There was a significant difference between the two groups (p=0.004). In another 15 patients who experienced both CSPCD and TSPCD, 14 patients (93%) stated a preference for TSPCD after converting from CSPCD to TSPCD, and one patient (7%) returned to CSPCD only at night.
CONCLUSIONS
In this study, TSPCD had the advantages of less morbidity as UTI and being more preferable by patients with relatively good daily activity compared with CSPCD. TSPCD is an alternative to CSPCD for the treatment of voiding dysfunction.
Keyword
MeSH Terms
Figure
Reference
-
1. Yang HM, Kim HJ. Clinical significance of suprapubic cystostomy in the treatments of patients with voiding difficulty. Korean J Urol. 2003. 44:283–287.2. Sohng I, Kim HJ. Long term follow up of suprapubic cystostomy. J Korean Continence Soc. 2004. 8:140–144.3. Lapides J, Diokno AC, Silber SJ, Lowe BS. Clean, intermittent self-catheterization in the treatment of urinary tract disease. J Urol. 1972. 107:458–461.4. Consortium for Spinal Cord Medicine. Bladder management for adults with spinal cord injury: a clinical practice guideline for health-care providers. J Spinal Cord Med. 2006. 29:527–573.5. Abrams P, Agarwal M, Drake M, El-Masri W, Fulford S, Reid S, et al. A proposed guideline for the urological management of patients with spinal cord injury. BJU Int. 2008. 101:989–994.6. Stöhrer M, Blok B, Castro-Diaz D, Chartier-Kastler E, Del Popolo G, Kramer G, et al. EAU Guidelines on neurogenic lower urinary tract dysfunction. Eur Urol. 2009. 56:81–88.7. Feifer A, Corcos J. Contemporary role of suprapubic cystostomy in treatment of neuropathic bladder dysfunction in spinal cord injured patients. Neurourol Urodyn. 2008. 27:475–479.8. Nomura S, Ishido T, Teranishi J, Makiyama K. Long-term analysis of suprapubic cystostomy drainage in patients with neuropathic bladder. Urol Int. 2000. 65:185–189.9. Cameron AP, Wallner LP, Tate DG, Sarma AV, Rodriguez GM, Clemens JQ. Bladder management after spinal cord injury in the United States 1972 to 2005. J Urol. 2010. 184:213–217.10. Groah SL, Weitzenkamp DA, Lammertse DP, Whiteneck GG, Lezotte DC, Hamman RF. Excess risk of bladder cancer in spinal cord injury: evidence for an association between indwelling catheter use and bladder cancer. Arch Phys Med Rehabil. 2002. 83:346–351.11. Esclarin De Ruz A, Garcia Leoni E, Herruzo Cabrera R. Epidemiology and risk factors for urinary tract infection in patients with spinal cord injury. J Urol. 2000. 164:1285–1289.12. West DA, Cummings JM, Longo WE, Virgo KS, Johnson FE, Parra RO. Role of chronic catheterization in the development of bladder cancer in patients with spinal cord injury. Urology. 1999. 53:292–297.13. So JG, Oh DJ, Lim YS, Park WH, Shim HB. Urologic complications and management in 337 spinal cord injured patients. Korean J Urol. 1997. 38:1075–1080.14. Lee KY, Jung TY, Shim HB. Analysis of urological complications according to the voiding method for spinal cord injury patients. Korean J Urol. 2004. 45:1252–1257.15. Reid G, Sobel JD. Bacterial adherence in the pathogenesis of urinary tract infection: a review. Rev Infect Dis. 1987. 9:470–487.16. Barford JM, Anson K, Hu Y, Coates AR. A model of catheter-associated urinary tract infection initiated by bacterial contamination of the catheter tip. BJU Int. 2008. 102:67–74.17. Kang JS, Choi NG. Comparative study of bacterial isolation and antibiotic sensitivity test between long-term silicone and nitrofurazone-coated suprapubic catheter indwelling patients. Korean J Urol. 2003. 44:1032–1037.18. Ahluwalia RS, Johal N, Kouriefs C, Kooiman G, Montgomery BS, Plail RO. The surgical risk of suprapubic catheter insertion and long-term sequelae. Ann R Coll Surg Engl. 2006. 88:210–213.19. Sheriff MK, Foley S, McFarlane J, Nauth-Misir R, Craggs M, Shah PJ. Long-term suprapubic catheterisation: clinical outcome and satisfaction survey. Spinal Cord. 1998. 36:171–176.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Long Term Follow up of Suprapubic Cystostomy
- Clinical Significance of Suprapubic Cystostomy in the Treatments of Patients with Voiding Difficulty
- Clinical Results of Transurethral Resection for the Benign Prostatic Hypertrophy -Significance of Suprapubic Cystostomy before Transurethral Resection-
- Clinicel Observetion of Urethroplasty after Suprapubic Cystostomy in 11 Cases Urethral Injuries
- Squamous Cell Carcinoma of the Suprapubic Cystostomy Tract With Bladder Involvement