Obstet Gynecol Sci.
2015 Nov;58(6):507-513. 10.5468/ogs.2015.58.6.507.
Factors affecting medication discontinuation in patients with overactive bladder symptoms
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Kyung Hee University Hospital, Seoul, Korea.
- 2Department of Obstetrics and Gynecology, Kyung Hee University Hospital at Gangdong, Kyung Hee University College of Medicine, Seoul, Korea. yooe7@khu.ac.kr
- 3Department of Statistics, Sungkyunkwan University, Seoul, Korea.
- KMID: 2314068
- DOI: http://doi.org/10.5468/ogs.2015.58.6.507
Abstract
OBJECTIVE
To find out the factors affecting medication discontinuation in patients with overactive bladder (OAB) symptoms.
METHODS
The clinical data of 125 patients with OAB symptoms who had taken antimuscarinics and behavioral therapy were retrospectively reviewed. Antimuscarinics related outcomes were evaluated by an independent observer with telephone interview. All patients were asked about duration of medication and reason of continuation or discontinuation of antimuscarinics. To determine pre-treatment factors predicting self-report discontinuation of antimuscarinics, variables of only those with P-values <0.25 on the univariate analysis were included in the Cox proportional hazard modeling.
RESULTS
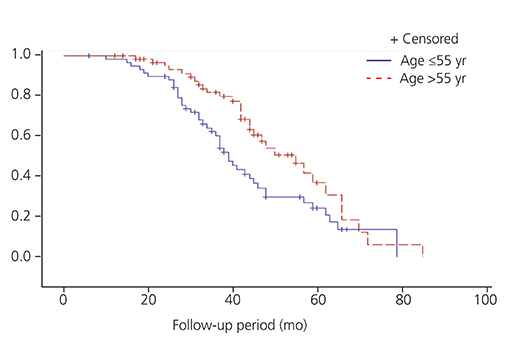
Mean follow-up was 39.6 months and the proportion of discontinuation of antimuscarinics was 60.0% (75/125). The mean duration of medication was 21.2 months in the continuation group and 3.3 months in the discontinuation group. The reasons of discontinuation of antimuscarinics were improved OAB symptoms (46.7%), tolerable OAB symptoms (33.3%), no change of OAB symptoms (1.3%), side-effects (8.0%) and no desire to take long-term medication (10.7%). The variables affecting remaining cumulative probability of antimuscarinics were age, history of anti-incontinence surgery or vaginal surgery, and having stress predominant urinary incontinence on urodynamic study.
CONCLUSION
The lower rate of cumulative continuation of antimuscarinics encourages us to give a more detailed counseling and education to the patients with OAB symptoms before prescription. And explorations about newer agent and non-pharmacologic treatment with good efficacy and lower side-effects are needed.
MeSH Terms
Figure
Reference
-
1. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002; 21:167–178.2. Coyne KS, Sexton CC, Irwin DE, Kopp ZS, Kelleher CJ, Milsom I. The impact of overactive bladder, incontinence and other lower urinary tract symptoms on quality of life, work productivity, sexuality and emotional well-being in men and women: results from the EPIC study. BJU Int. 2008; 101:1388–1395.3. Kannan H, Radican L, Turpin RS, Bolge SC. Burden of illness associated with lower urinary tract symptoms including overactive bladder/urinary incontinence. Urology. 2009; 74:34–38.4. Sexton CC, Coyne KS, Vats V, Kopp ZS, Irwin DE, Wagner TH. Impact of overactive bladder on work productivity in the United States: results from EpiLUTS. Am J Manag Care. 2009; 15:4 Suppl. S98–S107.5. Natalin R, Lorenzetti F, Dambros M. Management of OAB in those over age 65. Curr Urol Rep. 2013; 14:379–385.6. Chapple CR, Khullar V, Gabriel Z, Muston D, Bitoun CE, Weinstein D. The effects of antimuscarinic treatments in overactive bladder: an update of a systematic review and meta-analysis. Eur Urol. 2008; 54:543–562.7. Wagg AS. Antimuscarinic treatment in overactive bladder: special considerations in elderly patients. Drugs Aging. 2012; 29:539–548.8. Mauseth SA, Skurtveit S, Spigset O. Adherence, persistence and switch rates for anticholinergic drugs used for overactive bladder in women: data from the Norwegian Prescription Database. Acta Obstet Gynecol Scand. 2013; 92:1208–1215.9. Michel MC, Schneider T, Krege S, Goepel M. Does gender or age affect the efficacy and safety of tolterodine? J Urol. 2002; 168:1027–1031.10. Richter HE, Burgio KL, Chai TC, Kraus SR, Xu Y, Nyberg L, et al. Predictors of outcomes in the treatment of urge urinary incontinence in women. Int Urogynecol J Pelvic Floor Dysfunct. 2009; 20:489–497.11. Brubaker L, Fanning K, Goldberg EL, Benner JS, Trocio JN, Bavendam T, et al. Predictors of discontinuing overactive bladder medications. BJU Int. 2010; 105:1283–1290.12. Yu YF, Nichol MB, Yu AP, Ahn J. Persistence and adherence of medications for chronic overactive bladder/urinary incontinence in the california Medicaid program. Value Health. 2005; 8:495–505.13. Shaya FT, Blume S, Gu A, Zyczynski T, Jumadilova Z. Persistence with overactive bladder pharmacotherapy in a Medicaid population. Am J Manag Care. 2005; 11:4 Suppl. S121–S129.14. D'Souza AO, Smith MJ, Miller LA, Doyle J, Ariely R. Persistence, adherence, and switch rates among extended-release and immediate-release overactive bladder medications in a regional managed care plan. J Manag Care Pharm. 2008; 14:291–301.15. Benner JS, Nichol MB, Rovner ES, Jumadilova Z, Alvir J, Hussein M, et al. Patient-reported reasons for discontinuing overactive bladder medication. BJU Int. 2010; 105:1276–1282.16. Lawrence M, Guay DR, Benson SR, Anderson MJ. Immediate-release oxybutynin versus tolterodine in detrusor overactivity: a population analysis. Pharmacotherapy. 2000; 20:470–475.17. Balkrishnan R, Bhosle MJ, Camacho FT, Anderson RT. Predictors of medication adherence and associated health care costs in an older population with overactive bladder syndrome: a longitudinal cohort study. J Urol. 2006; 175(3 Pt 1):1067–1071.18. Krueger KP, Berger BA, Felkey B. Medication adherence and persistence: a comprehensive review. Adv Ther. 2005; 22:313–356.19. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005; 353:487–497.20. Malmsten UG, Molander U, Peeker R, Irwin DE, Milsom I. Urinary incontinence, overactive bladder, and other lower urinary tract symptoms: a longitudinal population-based survey in men aged 45-103 years. Eur Urol. 2010; 58:149–156.21. Basra RK, Wagg A, Chapple C, Cardozo L, Castro-Diaz D, Pons ME, et al. A review of adherence to drug therapy in patients with overactive bladder. BJU Int. 2008; 102:774–779.22. Jain P, Jirschele K, Botros SM, Latthe PM. Effectiveness of midurethral slings in mixed urinary incontinence: a systematic review and meta-analysis. Int Urogynecol J. 2011; 22:923–932.23. Kulseng-Hanssen S, Husby H, Schiotz HA. Follow-up of TVT operations in 1,113 women with mixed urinary incontinence at 7 and 38 months. Int Urogynecol J Pelvic Floor Dysfunct. 2008; 19:391–396.24. Kulseng-Hanssen S, Husby H, Schiotz HA. The tension free vaginal tape operation for women with mixed incontinence: do preoperative variables predict the outcome? Neurourol Urodyn. 2007; 26:115–121.25. Bradley CS, Nygaard IE. Vaginal wall descensus and pelvic floor symptoms in older women. Obstet Gynecol. 2005; 106:759–766.26. Digesu GA, Salvatore S, Chaliha C, Athanasiou S, Milani R, Khullar V. Do overactive bladder symptoms improve after repair of anterior vaginal wall prolapse? Int Urogynecol J Pelvic Floor Dysfunct. 2007; 18:1439–1443.27. de Boer TA, Kluivers KB, Withagen MI, Milani AL, Vierhout ME. Predictive factors for overactive bladder symptoms after pelvic organ prolapse surgery. Int Urogynecol J. 2010; 21:1143–1149.28. Miranne JM, Lopes V, Carberry CL, Sung VW. The effect of pelvic organ prolapse severity on improvement in overactive bladder symptoms after pelvic reconstructive surgery. Int Urogynecol J. 2013; 24:1303–1308.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Overactive Bladder
- Changes in Overactive Bladder Symptoms after Discontinuation of a Successful Treatment with Antimuscarinic Agent: A Prospective Trial
- Patient utilization survey of mirabegron prescribed for overactive bladder
- Persistence and compliance with medication management in the treatment of overactive bladder
- Antimuscarinic Agent Treatment Affecting Patient-Reported Outcomes in Overactive Bladder Syndrome With Depressive Symptoms