Obstet Gynecol Sci.
2013 May;56(3):194-197.
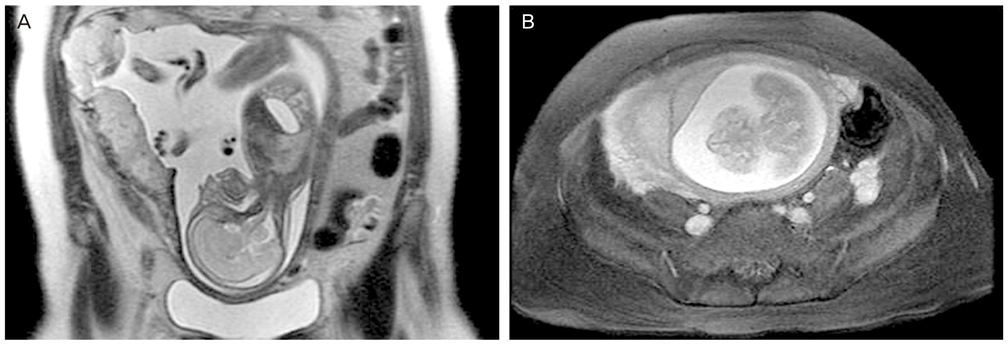
Conservative multidisciplinary management of placenta percreta following in vitro fertilization
- Affiliations
-
- 1Department of Obstetrics and Gynecology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea. jyshim@amc.seoul.kr
- 2Department of Obstetrics and Gynecology, Catholic University of Daegu School of Medicine, Daegu, Korea.
Abstract
- Placenta percreta is an extremely rare and the most severe form of placental invasion, that is associated with severe maternal morbidity and mortality. We report a case of nulliparous woman who underwent 10 cycles of in vitro fertilization (IVF) without any known risk factors. We conserved her uterus by spontaneous vaginal delivery, leaving the placenta in situ, pelvic arterial embolization, and primary resection of the remaining placental tissues. This case demonstrates that repetitive IVF is a possible risk factor for placental invasion, and that conservation of the uterus can be achieved in such cases using a multidisciplinary approach.
Keyword
MeSH Terms
Figure
Reference
-
1. Esmans A, Gerris J, Corthout E, Verdonk P, Declercq S. Placenta percreta causing rupture of an unscarred uterus at the end of the first trimester of pregnancy: case report. Hum Reprod. 2004. 19:2401–2403.2. Esh-Broder E, Ariel I, Abas-Bashir N, Bdolah Y, Celnikier DH. Placenta accreta is associated with IVF pregnancies: a retrospective chart review. BJOG. 2011. 118:1084–1089.3. Derman AY, Nikac V, Haberman S, Zelenko N, Opsha O, Flyer M. MRI of placenta accreta: a new imaging perspective. AJR Am J Roentgenol. 2011. 197:1514–1521.4. Committee on Obstetric Practice. American College of Obstetricians and Gynecologists. ACOG committee opinion. Placenta accreta. Number 266, January 2002. Int J Gynaecol Obstet. 2002. 77:77–78.5. Wong HS, Cheung YK, Zuccollo J, Tait J, Pringle KC. Evaluation of sonographic diagnostic criteria for placenta accreta. J Clin Ultrasound. 2008. 36:551–559.6. Fox H. Placenta accreta 1945-1969: a review. Obstet Gynecol Surv. 1972. 27:475–490.7. Timmermans S, van Hof AC, Duvekot JJ. Conservative management of abnormally invasive placentation. Obstet Gynecol Surv. 2007. 62:529–539.8. Panoskaltsis TA, Ascarelli A, de Souza N, Sims CD, Edmonds KD. Placenta increta: evaluation of radiological investigations and therapeutic options of conservative management. BJOG. 2000. 107:802–806.9. Soliman N, Babar SA. Spontaneous rupture of the uterus secondary to placenta percreta with conservation of the uterus. J Obstet Gynaecol. 2010. 30:517–518.10. Steins Bisschop CN, Schaap TP, Vogelvang TE, Scholten PC. Invasive placentation and uterus preserving treatment modalities: a systematic review. Arch Gynecol Obstet. 2011. 284:491–502.11. Horcajadas JA, Riesewijk A, Polman J, van Os R, Pellicer A, Mosselman S, et al. Effect of controlled ovarian hyperstimulation in IVF on endometrial gene expression profiles. Mol Hum Reprod. 2005. 11:195–205.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Placenta Percreta Involving the Urinary Bladder
- One Case of Placenta Previa Percreta with Bladder Invasion - One Case Report -
- A Case of Placenta Percreta during First Trimester
- Spontaneous uterine rupture from placenta percreta at 33 weeks' gestation after a single gynecologic surgery
- A Case of Placenta Previa-Percreta Treated with Methotrexate Treatment