Nutr Res Pract.
2011 Feb;5(1):46-51.
Zinc status and growth of Korean infants fed human milk, casein-based, or soy-based formula: three-year longitudinal study
- Affiliations
-
- 1Department of Food and Nutrition, Chungbuk National University, Gaesin-dong, Heungdeok-gu, Cheongju, Chungbuk 361-763, Korea. taisun@chungbuk.ac.kr
- 2Department of Medicine, College of Medicine, Chungbuk National University, Chungbuk 361-763, Korea.
- 3Department of Nutrition Sciences, University of Alabama at Birmingham, Birmingham, AL 35294, USA.
Abstract
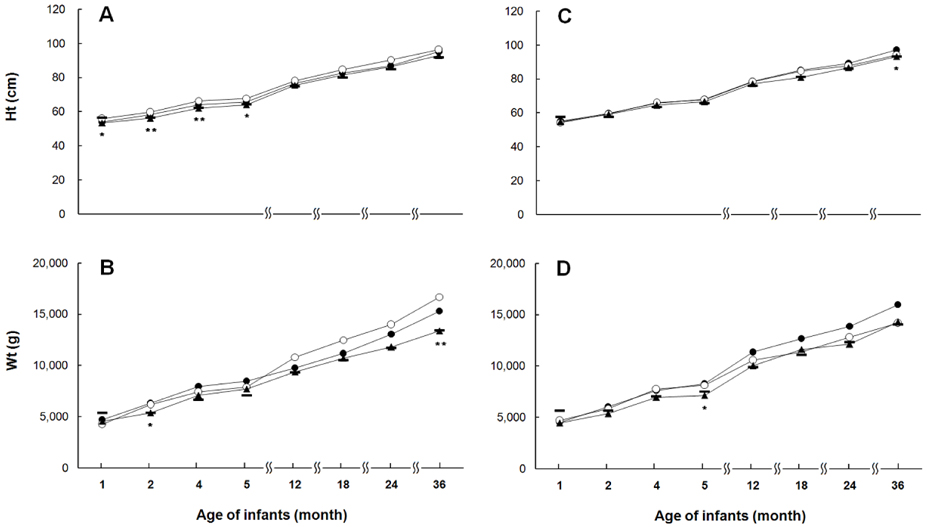
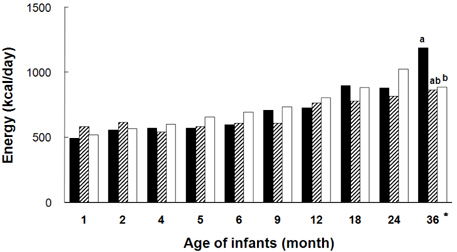
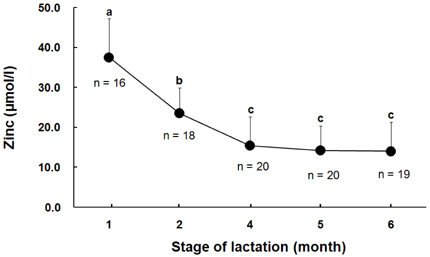
- To evaluate the effect of feeding methods on growth and zinc nutritional status of infants early in life, we monitored from birth to 36 months in 51 infants who were exclusively fed human milk (HM, n = 20), casein-based formula (CBF, n = 12), or soy-based formula (SBF, n = 19) during the first five months of life. Zinc status was assessed by analyzing serum zinc concentrations and zinc intakes. Zinc contents in HM and formulas were measured. Zinc intake was estimated by weighing infants before and after feeding in the HM group and by collecting formula-intake records in the CBF and SBF groups. After solid foods were introduced, all foods consumed were also included to estimate zinc intake. The growth of infants in all groups was similar to that established for normal Korean infants. Human milk zinc concentrations declined as lactation progressed. Zinc concentrations in all formulas tested in this study were higher than HM and were also higher than those claimed by the manufacturers. During the first twelve months, mean serum zinc concentrations of infants were similar in all groups, although infants in the HM group consistently had the lowest zinc intake among the groups, and the overall zinc intake in infants fed SBF was highest. This finding could be explained by the different zinc bioavailability of HM and formulas. In conclusion, infants fed HM, CBF or SBF has normal growth up to three years of age, although HM contained the lowest zinc concentration followed by CBF, then SBF.
MeSH Terms
Figure
Reference
-
1. Geneva: The optimal duration of exclusive breastfeeding. Report of an expert consultation. WHO [Internet]. c2002. cited 2010 June 28. Available from: http://www.who.int/nutrition/publications/optimal_duration_of_exc_bfeeding_report_eng.pdf.2. Picciano MF. Nutrient composition of human milk. Pediatr Clin North Am. 2001. 48:53–67.
Article3. Geneva: Global strategy for infant and young child feeding. WHO, UNICEF [Internet]. c2003. cited 2010 June 28. Available from: http://www.unicef.org/india/Global_Strategy_for_Infant_and_Young_Child_Feeding__WHO_and_UNICEF.pdf.4. O'Connor DL, Brennan J, Merko S. Thureen PJ, Hay WW, editors. Formulas for preterm and term infants. Neonatal Nutrition and Metabolism. 2006. 2nd ed. New York: Cambridge University Press;409–436.5. Han YH, Yon M, Han HS, Kim KY, Tamura T, Hyun TH. Folate contents in human milk and casein-based and soya-based formulas, and folate status in Korean infants. Br J Nutr. 2009. 101:1769–1774.
Article6. Standard for infant formula and formulas for special medical purpose intended for infants. Codex Stan 72-1981. CODEX Alimentarius [Internet]. Available from: http://www.codexalimentarius.net/download/standards/288/CXS_072e.pdf.7. Tamura T, Johnston KE, Freeberg LE, Perkins LL, Goldenberg RL. Refrigeration of blood samples prior to separation is essential for the accurate determination of plasma or serum zinc concentrations. Biol Trace Elem Res. 1994. 41:165–173.
Article8. The Korean Nutrition Society. Recommended dietary allowances for Koreans. 2000. 7th revision. Seoul: Joongang Publishing Co;266–435.9. Hyun TH, Barrett-Connor E, Milne DB. Zinc intakes and plasma concentrations in men with osteoporosis: the Rancho Bernardo Study. Am J Clin Nutr. 2004. 80:715–721.
Article10. Seoul: 2007 Korean children and adolescents growth standard. Korea Centers for Disease Control and Prevention, Korean Pediatric Society [Internet]. cited 2008 June 28. Available from: http://www.cdc.go.kr.11. Hotz C, Peerson JM, Brown KH. Suggested lower cutoffs of serum zinc concentrations for assessing zinc status: reanalysis of the second national health and nutrition examination survey data (1976-1980). Am J Clin Nutr. 2003. 78:756–764.
Article12. Schneider JM, Fujii ML, Lamp CL, Lönnerdal B, Zidenberg-Cherr S. The prevalence of low serum zinc and copper levels and dietary habits associated with serum zinc and copper in 12- to 36-month-old children from low-income families at risk for iron deficiency. J Am Diet Assoc. 2007. 107:1924–1929.
Article13. Lasekan JB, Ostrom KM, Jacobs JR, Blatter MM, Ndife LI, Gooch WM 3rd, Cho S. Growth of newborn, term infants fed soy formula for 1 year. Clin Pediatr (Phila). 1999. 38:563–571.
Article14. Mendez MA, Anthony MS, Arab L. Soy-based formulae and infant growth and development: a review. J Nutr. 2002. 132:2127–2130.
Article15. Seppo L, Korpela R, Lönnerdal B, Metsäniitty L, Juntunen-Backman K, Klemola T, Paganus A, Vanto T. A follow-up study of nutrient intake, nutritional status, and growth in infants with cow milk allergy fed either a soy formula or an extensively hydrolyzed whey formula. Am J Clin Nutr. 2005. 82:140–145.
Article16. Vuori E, Kuitunen P. The concentrations of copper and zinc in human milk. A longitudinal study. Acta Paediatr Scand. 1979. 68:33–37.
Article17. Krebs NF, Hambidge KM, Jacobs MA, Rasbach JO. The effects of a dietary zinc supplement during lactation on longitudinal changes in maternal zinc status and milk zinc concentrations. Am J Clin Nutr. 1985. 41:560–570.
Article18. Karra MV, Kirksey A. Variation in zinc, calcium, and magnesium concentrations of human milk within a 24-hour period from 1 to 6 months of lactation. J Pediatr Gastroenterol Nutr. 1988. 7:100–106.
Article19. Lamounier JA, Danelluzzi JC, Vannucchi H. Zinc concentrations in human milk during lactation: a 6-month longitudinal study in southern Brazil. J Trop Pediatr. 1989. 35:31–34.
Article20. Nagra SA. Longitudinal study in biochemical composition of human milk during first year of lactation. J Trop Pediatr. 1989. 35:126–128.
Article21. Nyazema NZ, Mahomva O, Andifasi W. The levels of zinc in breast milk of urban African women in Zimbabwe. Afr J Med Med Sci. 1989. 18:159–162.22. Simmer K, Ahmed S, Carlsson L, Thompson RP. Breast milk zinc and copper concentrations in Bangladesh. Br J Nutr. 1990. 63:91–96.
Article23. Moser-Veillon PB, Reynolds RD. A longitudinal study of pyridoxine and zinc supplementation of lactating women. Am J Clin Nutr. 1990. 52:135–141.
Article24. Ohtake M, Tamura T. Changes in zinc and copper concentrations in breast milk and blood of Japanese women during lactation. J Nutr Sci Vitaminol (Tokyo). 1993. 39:189–200.
Article25. Hurley LS, Duncan JR, Sloan MV, Eckhert CD. Zinc-binding ligands in milk and intestine: a role in neonatal nutrition? Proc Natl Acad Sci U S A. 1977. 74:3547–3549.
Article26. Ohtake M, Chiba R, Mochizuki K, Tada K. Zinc and copper concentrations in human milk and in serum from exclusively-breast-fed infants during the first 3 months of life. Tohoku J Exp Med. 1981. 135:335–343.
Article27. Craig WJ, Balbach L, Harris S, Vyhmeister N. Plasma zinc and copper levels of infants fed different milk formulas. J Am Coll Nutr. 1984. 3:183–186.
Article28. Hambidge KM, Walravens PA, Casey CE, Brown RM, Bender C. Plasma zinc concentrations of breast-fed infants. J Pediatr. 1979. 94:607–608.
Article29. Sandström B, Cederblad Å, Lönnerdal B. Zinc absorption from human milk, cow's milk, and infant formulas. Am J Dis Child. 1983. 137:726–729.
Article30. Casey CE, Walravens PA, Hambidge KM. Availability of zinc: loading tests with human milk, cow's milk, and infant formulas. Pediatrics. 1981. 68:394–396.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effects of Soy-Based Infant Formula on Growth and Development, and the Isoflavone Concentration of Plasma and Urine in Full-Term Infants
- A Longitudinal Study of the Iron and Zinc Intakes of Korean Infants from 1 to 3 Months-Breast-Fed vs Formula-Fed Infants
- A Longitudinal Study of Calcium and Phosphorus Intakes of Korean Infants from 1 to 3 Months in Breast-Fed vs Formula-Fed Infants
- Growth Patterns of Indonesian Infants with Cow's Milk Allergy and Fed with Soy-Based Infant Formula
- Effects of soy-based formula on infants' growth and blood laboratory values spanning 3 years after birth