J Dent Anesth Pain Med.
2015 Dec;15(4):247-249.
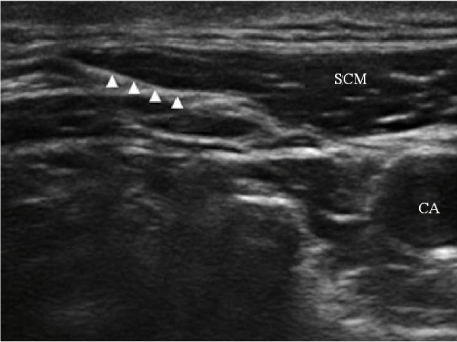
Treatment of herpes zoster with ultrasound-guided superficial cervical plexus block
- Affiliations
-
- 1Anesthesiology and Pain Medicine, School of Medicine, Kyungpook National University Hospital, Daegu, Korea.
- 2Anesthesiology and Pain Medicine, School of Dentistry, Kyungpook National University, Daegu, Korea. jeon68@knu.ac.kr
Abstract
- Herpes zoster most commonly occurs in elderly patients, and usually affects sensory neurons. Therefore, its characteristic symptoms are segmental pain, itching, and sensory changes in the affected areas. A 71-yr-old woman experienced painful herpetic rash on the right cervical 2-4 dermatomes for 16 days. Two days after the onset of the rash, she was diagnosed with herpes zoster, and prescribed 250 mg famciclovir three times a day for 7 days, pregabalin 150 mg twice a day, and tramadol 150 mg once a day for 14 days, by a dermatologist. Despite medication, her pain was rated at an intensity of 6/10 on the numeric rating scale. In addition, she complained of severe itching sensation on the affected dermatomes. Superficial cervical plexus block (SCPB) was performed at the right C4 level with 15 ml 0.5% lidocaine plus triamcinolone 30 mg. Five days after the procedure, pain and itching completely disappeared. SCPB may be an effective option for the treatment of acute pain and itching arising from herpes zoster, and for the prevention of postherpetic neuralgia.
Keyword
MeSH Terms
Figure
Reference
-
1. Johnson RW, Wasner G, Saddier P, Baron R. Herpes zoster and postherpetic neuralgia: Optimizing management in the elderly patient. Drugs Aging. 2008; 25:991–1006.2. Jeon YH. Herpes Zoster and Postherpetic Neuralgia: Practical Consideration for Prevention and Treatment. Korean J Pain. 2015; 28:177–184.
Article3. Manabe H, Dan K, Higa K. Continuous epidural infusion of local anesthetics and shorter duration of acute zoster-associated pain. Clin J Pain. 1995; 11:220–228.
Article4. Hardy D. Relief of pain in acute herpes zoster by nerve blocks and possible prevention of post-herpetic neuralgia. Can J Anaesth. 2005; 52:186–190.
Article5. Pandit JJ, Dutta D, Morris JF. Spread of injectate with superficial cervical plexus block in humans: An anatomical study. Br J Anaesth. 2003; 91:733–735.
Article6. Drolet M, Brisson M, Schmader K, Levin M, Johnson R, Oxman M, et al. Predictors of postherpetic neuralgia among patients with herpes zoster: A prospective study. J Pain. 2010; 11:1211–1221.
Article7. Kumar V, Krone K, Mathieu A. Neuraxial and sympathetic blocks in herpes zoster and postherpetic neuralgia: An appraisal of current evidence. Reg Anesth Pain Med. 2004; 9:454–461.
Article8. Moen V, Dahlgren N, Irestedt L. Severe neurological complications after central neuraxial blockades in Sweden 1990–1999. Anesthesiology. 2004; 101:950–959.
Article9. Johansson A, Bennett GJ. Effect of local methylprednisolone on pain in a nerve injury model: A pilot study. Reg Anesth. 1997; 22:59–65.
Article10. O'Gradaigh D, Merry P. Corticosteroid injection for the treatment of carpal tunnel syndrome. Ann Rheum Dis. 2000; 59:918–919.11. Pandit JJ, Satya-Krishna R, Gration P. Superficial or deep cervical plexus block for carotid endarterectomy: a systematic review of complications. Br J Anaesth. 2007; 99:159–169.
Article12. Shteif M, Lesmes D, Hartman G, Ruffino S, Laster Z. The use of the superficial cervical plexus block in the drainage of submandibular and submental abscesses - An alternative for general anesthesia. J Oral Maxillofac Surg. 2008; 66:2642–2645.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acute Pain Relief by Superficial Cervical Plexus Block in the Patient with Herpes Zoster
- Superficial Cervical Plexus Block for Acute Herpes Zoster at C3-4 Dermatome
- Treatment of Herpes Zoster: Nerve Block
- A Comparison of Combined Superficial Cervical Plexus Block and Interscalene Brachial Plexus Block with General Anesthesia for Clavicle Surgery: Pilot Trial
- Ultrasound-guided superficial cervical plexus block for carotid endarterectomy in a patient with Lemierre syndrome: A case report