Korean Circ J.
2012 Jan;42(1):16-22. 10.4070/kcj.2012.42.1.16.
Atypical Symptom Cluster Predicts a Higher Mortality in Patients With First-Time Acute Myocardial Infarction
- Affiliations
-
- 1Department of Nursing, Chosun University College of Medicine, Gwangju, Korea. seon9772@chosun.ac.kr
- 2Department of Cardiology, Chonnam National University College of Medicine, Gwangju, Korea.
- KMID: 2297903
- DOI: http://doi.org/10.4070/kcj.2012.42.1.16
Abstract
- BACKGROUND AND OBJECTIVES
Identifying symptom clusters of acute myocardial infarction (AMI) and their clinical significance may be useful in guiding treatment seeking behaviors and in planning treatment strategy. The aim of this study was to identify clusters of acute symptoms and their associated factors that manifested in patients with first-time AMI, and to compare clinical outcomes among cluster groups within 1-year of follow-up.
SUBJECTS AND METHODS
A total of 391 AMI patients were interviewed individually using a structured questionnaire for acute and associated symptoms between March 2008 and June 2009 in Korea.
RESULTS
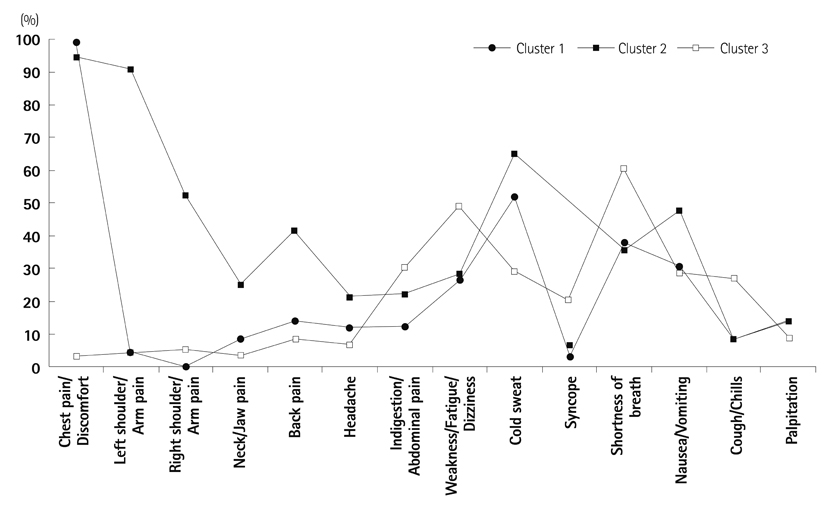
Among 14 acute symptoms, three distinct clusters were identified by Latent Class Cluster Analysis: typical chest symptom (57.0%), multiple symptom (27.9%), and atypical symptom (15.1%) clusters. The cluster with atypical symptoms was characterized by the least chest pain (3.4%) and moderate frequencies (31-61%) of gastrointestinal symptoms, weakness or fatigue, and shortness of breath; they were more likely to be older, diabetic and to have worse clinical markers at hospital presentation compared with those with other clusters. Cox proportional hazards regression analysis showed that, when age and gender were adjusted for, the atypical symptom cluster significantly predicted a higher risk of 1-year mortality compared to the typical chest pain cluster (hazard ratio 3.288, 95% confidence interval 1.087-9.943, p=0.035).
CONCLUSION
Clusters of symptoms can be utilized in guiding a rapid identification of symptom patterns and in detecting higher risk patients. Intensive treatment should be considered for older and diabetic patients with atypical presentation.
MeSH Terms
Figure
Reference
-
1. Milner KA, Funk M, Richards S, Vaccarino V, Krumholz HM. Symptom predictors of acute coronary syndromes in younger and older patients. Nurs Res. 2001. 50:233–241.2. Leslie WS, Urie A, Hooper J, Morrison CE. Delay in calling for help during myocardial infarction: reasons for the delay and subsequent pattern of accessing care. Heart. 2000. 84:137–141.3. Horne R, James D, Petrie K, Weinman J, Vincent R. Patients' interpretation of symptoms as a cause of delay in reaching hospital during acute myocardial infarction. Heart. 2000. 83:388–393.4. Canto JG, Shlipak MG, Rogers WJ, et al. Prevalence, clinical characteristics, and mortality among patients with myocardial infarction presenting without chest pain. JAMA. 2000. 283:3223–3229.5. Brieger D, Eagle KA, Goodman SG, et al. Acute coronary syndromes without chest pain, an underdiagnosed and undertreated high-risk group: insights from the Global Registry of Acute Coronary Events. Chest. 2004. 126:461–469.6. Barsevick AM, Whitmer K, Nail LM, Beck SL, Dudley WN. Symptom cluster research: conceptual, design, measurement, and analysis issues. J Pain Symptom Manage. 2006. 31:85–95.7. Dodd M, Janson S, Facione N, et al. Advancing the science of symptom management. J Adv Nurs. 2001. 33:668–676.8. Miaskowski C, Dodd M, Lee K. Symptom clusters: the new frontier in symptom management research. J Natl Cancer Inst Monogr. 2004. 32:17–21.9. Ryan CJ, DeVon HA, Horne R, et al. Symptom clusters in acute myocardial infarction: a secondary data analysis. Nurs Res. 2007. 56:72–81.10. McSweeney JC, Cleves MA, Zhao W, Lefler LL, Yang S. Cluster analysis of women's prodromal and acute myocardial infarction symptoms by race and other characteristics. J Cardiovasc Nurs. 2010. 25:311–322.11. Lindgren TG, Fukuoka Y, Rankin SH, Cooper BA, Carroll D, Munn YL. Cluster analysis of elderly cardiac patients' prehospital symptomatology. Nurs Res. 2008. 57:14–23.12. Fukuoka Y, Lindgren TG, Rankin SH, Cooper BA, Carroll DL. Cluster analysis: a useful technique to identify elderly cardiac patients at risk for poor quality of life. Qual Life Res. 2007. 16:1655–1663.13. Vermunt JK, Magidson J. Latent Gold user's guide. 2000. Belmont: Statistical Innovations.14. Fraley C, Raftery AE. How many clusters? Which clustering method? Answers via model-based cluster analysis. Comput J. 1998. 41:578–588. doi: 10.1093/comjnl/41.8.578.15. Riegel B, Hanlon AL, McKinley S, et al. Differences in mortality in acute coronary syndrome symptom clusters. Am Heart J. 2010. 159:392–398.16. Thuresson M, Jarlöv MB, Lindahl B, Svensson L, Zedigh C, Herlitz J. Thoughts, actions, and factors associated with prehospital delay in patients with acute coronary syndrome. Heart Lung. 2007. 36:398–409.17. Moser DK, Kimble LP, Alberts MJ, et al. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: a scientific statement from the American Heart Association Council on Cardiovascular Nursing and Stroke Council. Circulation. 2006. 114:168–182.18. Hwang SY. Comparison of clinical manifestations and treatment-seeking behaviors in younger and older patients with first-time acute coronary syndrome. J Korean Acad Nurs. 2009. 39:888–898.19. Berg J, Björck L, Dudas K, Lappas G, Rosengren A. Symptoms of a first acute myocardial infarction in women and men. Gend Med. 2009. 6:454–462.20. Hwang SY, Park EH, Shin ES, Jeong MH. Comparison of factors associated with atypical symptoms in younger and older patients with acute coronary syndromes. J Korean Med Sci. 2009. 24:789–794.21. Then KL, Rankin JA, Fofonoff DA. Atypical presentation of acute myocardial infarction in 3 age groups. Heart Lung. 2001. 30:285–293.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Can time delay be shortened in the treatment of acute myocardial infarction?: Experience from Korea acute myocardial infarction registry
- The Impact of Initial Treatment Delay Using Primary Angioplasty on Mortality among Patients with Acute Myocardial Infarction: from the Korea Acute Myocardial Infarction Registry
- Serum Myoglobin in the Early Phase of Acute Myocardial Infarction
- Three Cases of Ventricular Septal Rupture after Acute Myocardial Infarction
- Symptom Clusters in Korean Patients with Acute Myocardial Infarction