J Korean Fract Soc.
2007 Jul;20(3):239-245. 10.12671/jkfs.2007.20.3.239.
The Surgical Outcomes for Isolated Greater Tuberosity Fracture of Proximal Humerus
- Affiliations
-
- 1Department of Orthopaedic Surgery, College of Medicine, Chonnam National University, Gwangju, Korea. rhamses@chol.com
- KMID: 2296824
- DOI: http://doi.org/10.12671/jkfs.2007.20.3.239
Abstract
- PURPOSE
To evaluate the adequate surgical methods and postoperative rehabilitation by analyzing the outcome of surgical treatment for isolated greater tuberosity fracture of proximal humerus.
MATERIALS AND METHODS
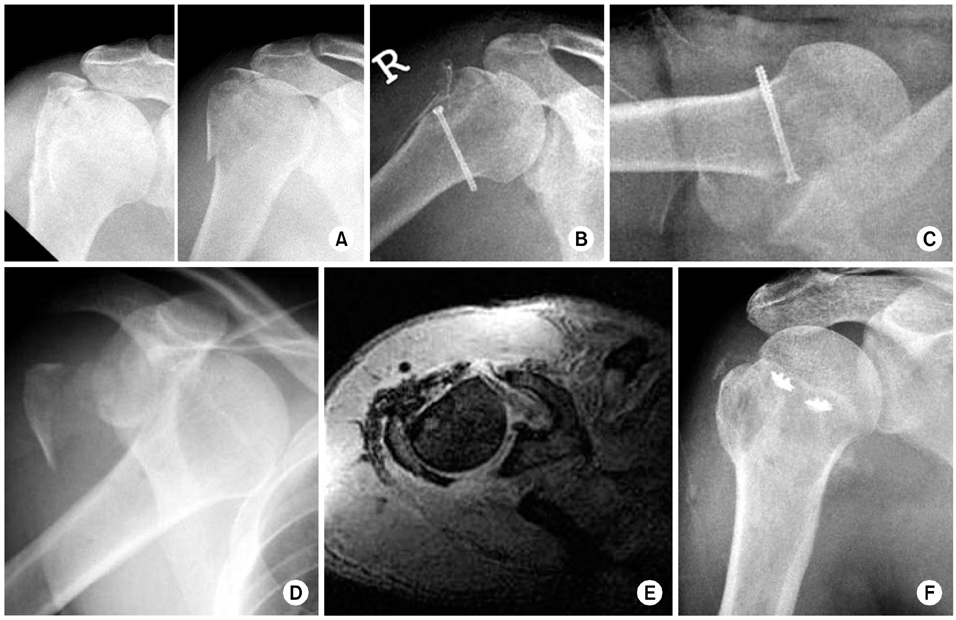
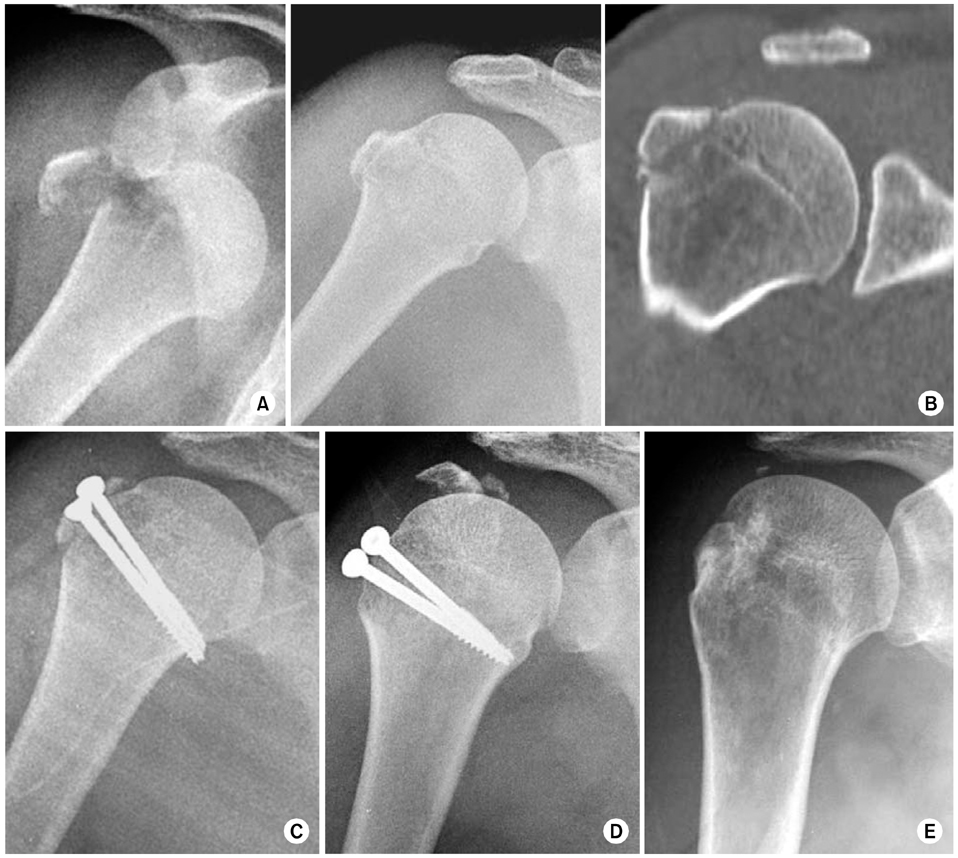
Ten patients who allowed at least 1 year follow up after the surgical treatment of isolated greater tuberosity fractures were evaluated. Their mean age was 52.3 years (range, 28~67) and mean follow up duration was 23.8 months (range, 12~36). We choosed the different approaches and fixation methods according to size, location and presence of comminution of the fragment, and combined injury. The rehabilitation programs were indivisualized and we evaluated the clinical outcomes using UCLA and Constant scoring system.
RESULTS
According to the UCLA scoring system, 5 cases were excellent, 3 cases were satisfactory, and 2 cases were unsatisfactory. By the Constant scoring system, 8 cases were excellent and 2 cases were good. The average bony union time was 7.6 weeks (range, 6~8) except the 2 cases of revision surgery. Two cases were operated using cannulated screws alone, 3 cases using only nonabsorbable sutures and 5 cases using cannulated screws and nonabsorbable sutures. One out of two revision cases was developed from the negligence of preoperative shoulder anterior dislocation with rupture of subscapularis, and the other was caused by improper immobilization of the fracture site postoperatively.
CONCLUSION
Not only the adequate surgical approaches and the fixation methods according to the size and comminution of fragment, but also the identification of combined injuries were very important in the surgical treatment for the isolated greater tuberosity fracture. And we considered that the adequate postoperative rehabilitation and proper protection based on the intraoperative fixation stability play an important role for the better clinical and radiological outcomes.
MeSH Terms
Figure
Cited by 2 articles
-
The Surgical Outcomes of Isolated Greater Tuberosity Fractures of the Proximal Humerus Fixed with the Spring Plate
Dong-Ju Shin, Young-Soo Byun, Se-Ang Chang, Hee-Min Yun, Ho-Won Park, Jae-Young Park
J Korean Fract Soc. 2009;22(3):159-165. doi: 10.12671/jkfs.2009.22.3.159.Clinical Features and Characteristics of Greater Tuberosity Fractures with or without Shoulder Dislocation
Dong-Wan Kim, Young-Jae Lim, Ki-Cheor Bae, Beom-Soo Kim, Yong-Ho Lee, Chul-Hyun Cho
J Korean Fract Soc. 2018;31(4):139-144. doi: 10.12671/jkfs.2018.31.4.139.
Reference
-
1. Bigliani LU, Flatow EL. Acromioclavicular fractures of the proximal humerus. In : Rockwood CA, Matsen FA, editors. The shoulder. 2nd ed. Philadelphia: WB Saunders Co;1998. p. 337–389.2. Carrera EF, Matsumoto MH, Netto NA, Faloppa F. Fixation of greater tuberosity fractures. Arthroscopy. 2004; 20:e109–e111.
Article3. Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987; 214:160–164.
Article4. DePalma AF, Cautilli RA. Fractures of the upper end of the humerus. Clin Orthop. 1961; 20:73–93.5. Ellman H, Hanker G, Bayer M. Repair of the rotator cuff. End-result study of factors influencing reconstruction. J Bone Joint Surg Am. 1986; 68:1136–1144.
Article6. Flatow EL, Cuomo F, Maday MG, Miller SR, McIlveen SJ, Bigliani LU. Open reduction and internal fixation of two-part displaced fractures of the greater tuberosity of the proximal part of the humerus. J Bone Joint Surg Am. 1991; 73:1213–1218.
Article7. Green A, Izzi J. Isolated fractures of the greater tuberosity of the proximal humerus. J Shoulder Elbow Surg. 2003; 12:641–649.
Article8. Kang HJ, Lee DH, Yoon HK, Hahn SB. Cannulated screw fixation for 4 part fractures of the neck of humerus. J Korean Fract Soc. 2005; 18:432–436.
Article9. Kim E, Shin HK, Kim CH. Characteristics of an isolated greater tuberosity fracture of the humerus. J Orthop Sci. 2005; 10:441–444.
Article10. Kim SH, Ha KI. Arthroscopic treatment of symptomatic shoulders with minimally displaced greater tuberosity fracture. Arthroscopy. 2000; 16:695–700.
Article11. Neer CS. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970; 52:1077–1089.12. Park TS, Choi IY, Kim YH, Park MR, Shon JH, Kim SI. A new suggestion for the treatment of minimally displaced fractures of the greater tuberosity of the proximal humerus. Bull Hosp Jt Dis. 1997; 56:171–176.13. Platzer P, Kutscha-Lissberg F, Lehr S, Vecsei V, Gaebler C. The influence of displacement on shoulder function in patients with minimally displaced fractures of the greater tuberosity. Injury. 2005; 36:1185–1189.
Article14. Rockwood CA, Green DP. Fractures in adults. 5th ed. Philadelphia: Lippincott;2001. p. 1012–1017.15. Schai PA, Hintermann B, Koris MJ. Preoperative arthroscopic assessment of fractures about the shoulder. Arthroscopy. 1999; 15:827–835.
Article16. Shin DJ, Chang SA, Byun YS, Hwang DH, Lee SR, Kim SH. T-plate fixation for two- and three-part fractures of the proximal humerus. J Korean Fract Soc. 2005; 18:426–431.
Article17. Taverna E, Sansone V, Battistella F. Arthroscopic treatment for greater tuberosity fractures: rationale and surgical technique. Arthroscopy. 2004; 20:e53–e57.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Surgical Outcomes of Isolated Greater Tuberosity Fractures of the Proximal Humerus Fixed with the Spring Plate
- Isolated Avulsion Fracture of the Lesser Tuberosity of the Humerus: A Case Report
- Analysis of Risk Factors for Occult Surgical Neck Fracture Accompanying Isolated Greater Tuberosity Fracture of Humerus
- Isolated Avulsion Fracture of the Subscapularis from the Lesser Tuberosity of the Humerus in a 12-Year-Old Boy - A Case Report -
- Shoulder Quadruple Dislocation Fracture: Fracture of Glenoid Rim, Coracoid Process, Greater Tuberosity, Surgical Neck of Humerus Associated with Anterior Shoulder Dislocation: A Case Report